Types of injuries to the oral mucosa
Machine translation
Original article is written in RU language (link to read it).
The oral mucosa is constantly exposed to some irritants. Even when eating food, the oral mucosa is affected by both mechanical factors (the very element of chewing food) and chemical factors: spicy and salty foods, hot drinks, alcohol, smoking. However, with the significant strength of local and general immunity, these effects do not cause significant harm to the mucous membrane, since the mucous membrane has good protective and regenerative properties.
More relevant information on diseases of the oral mucosa in the section of our website Training in Periodontology .
In this article we will look at traumatic lesions of the oral mucosa.

The protective mechanisms of the oral mucosa are specific, that is, immune defense, and nonspecific. Nonspecific protective factors include saliva and its components, such as lysozyme, dextrans, proteases and glycolytic enzymes, phagocytic factors, and complement factors.
All of the above protective factors of the oral mucosa do not always cope with their task, and when exposed to external (exogenous) factors, traumatic lesions of the oral mucosa occur.
Classification of traumatic lesions of the oral mucosa
The classification of traumatic lesions of the oral mucosa includes the course of injury:
acute traumatic injury to the oral mucosa;
chronic traumatic damage to the oral mucosa;
By their nature, traumatic lesions of the oral mucosa are divided into:
mechanical damage to the oral mucosa;
physical (radiation and thermal) damage to the oral mucosa;
chemical damage to the oral mucosa.
It is possible to distinguish a classification of traumatic lesions of the oral mucosa according to the factor that had a pathological effect:
domestic injury (domestic);
sports;
road;
production.
It is not difficult to determine the nature of the injury, its course and the nature of its occurrence by carefully collecting an anamnesis.
Mechanical injury to the oral mucosa
Mechanical injury to the oral mucosa can be either acute or chronic. Determining the course of a mechanical injury to the oral cavity is not difficult; you just need to clarify the time of occurrence of the resulting mechanical injury.

Mechanical injury to the oral mucosa is one of the most common injuries, especially among men and children, meaning acute mechanical injury to the oral mucosa.
Etiology of acute mechanical trauma of the oral mucosa
The leading causes of acute mechanical injury to the oral mucosa are considered to be:
Strikes. Blows can be with a fist or an object, or against an object, a fall.
Bites.
Injuries from cutting and piercing objects.
Clinic of acute mechanical trauma of the oral mucosa
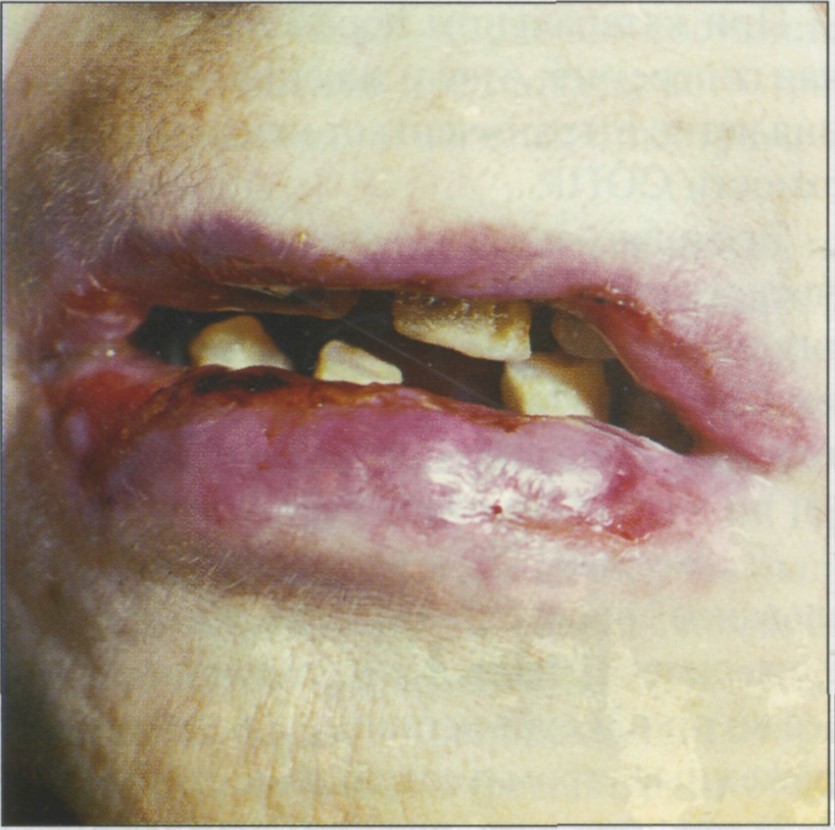
The clinical picture of acute mechanical injury is accompanied by slight pain. At the site of an acute mechanical injury there may be either erosion, an ulcer, or an area of hemorrhage. Often erosion and ulcers are irregular in shape, with unclear edges. Erosion on the oral mucosa heals quickly, but with secondary infection the erosion turns into an ulcer. If there was hemorrhage, then after 1-3 days the color will change to bluish-purple or black-violet.
Treatment of acute mechanical trauma of the oral mucosa
Treatment of acute mechanical trauma to the oral mucosa does not present any difficulties. So, if there is bleeding, use hydrogen peroxide 1.5%; Treat the damaged area with a warm antiseptic solution; if there is significant pain, you can use an anesthetic, for example, 2% lidocaine. The patient is prescribed oral baths with a warm antiseptic solution and applications of foam aerosols (pentanol, hyposol). If the wound was very deep, then stitches should be applied.

Chronic injury to the oral mucosa
Chronic injury to the oral mucosa involves exposure to an irritating factor for a long time. The main reasons for the occurrence of chronic trauma to the oral mucosa are:
overhanging edges of fillings;
unrestored contact point;
low-quality prostheses;
dental anomalies (teeth outside the dental arch, deep, open, cross bite);
metal ligatures;
poor quality tires;
bad habits.

All these factors trigger the catarrhal reaction. The severity of the inflammatory phases (exudation and proliferation) in these cases depends on the location of the stimulus, its strength and duration of action. Thus, some chronic mechanical injuries of the oral mucosa can be accompanied by serous, serous-purulent and purulent discharge. With purulent exudation, erosion occurs on the oral mucosa; in the absence of treatment for erosion, an ulcer appears on the oral mucosa; with mechanical trauma, it is called decubital (i.e., traumatic).

Clinic for chronic mechanical trauma of the oral mucosa
The clinical picture of chronic mechanical trauma to the oral mucosa is not characterized by a clear picture. Patients most often do not complain. Complaints from chronic mechanical trauma of the oral mucosa are most often a feeling of awkwardness, discomfort, complaints of swelling, soreness.
Erosion due to chronic mechanical trauma of the oral mucosa is not characterized by severe pain, which cannot be said about decubital ulcers. Decubital ulcers are very painful when eating and talking. If you examine it, the doctor may notice uneven edges, hyperemia along the periphery, fibrinous plaque in the center, which, when removed, exposes the bleeding surface. When an ulcer persists for a long time, its edges become denser and it is capable of epithelialization. Decubital ulcers can be of different depths; in the clinic, there have been cases when the depth of a decubital ulcer in chronic trauma of the oral mucosa reached the muscle layer.
Treatment of chronic mechanical trauma of the oral mucosa
First of all, treatment of chronic mechanical trauma to the oral mucosa should be aimed at eliminating the irritating factor. All fillings must be restored, dentures must be adjusted (in principle, dentures are not recommended to be worn during treatment of ulcers).
If it is painful, the erosion/ulcer should be treated with a warm anesthetic solution, the same 2% lidocaine. To facilitate the removal of necrotic or fibrin films, it is necessary to treat the wound with proteolytic enzymes for 1-2 minutes before starting this procedure. Foam aerosols, healing ointments such as solcoseryl, and keratoplastics (sea buckthorn and rosehip oil) are applied.
Thermal damage to the oral mucosa
Thermal damage to the oral mucosa occurs when exposed to excessive temperature. Hot food, drinks, careless work with the coagulator, incorrect electrophoresis technique. The degree of damage to the mucous membrane depends on the duration of the temperature stimulus. Therefore, a wound that occurs due to thermal damage to the oral mucosa can be:
limited;
spilled;
hyperemic;
vesicular;
with secondary infection;
without secondary infection.
Clinic for thermal damage to the oral mucosa
The clinic of thermal damage to the oral mucosa is characterized by constant pain, aggravated by eating, talking, and any impact on the affected area. Often, with thermal damage to the oral mucosa, blisters appear, after opening which erosions occur. In more severe cases, a dark gray or black area of necrosis may appear.


Treatment of thermal damage to the oral mucosa
Treatment of thermal damage to the oral mucosa consists of the application of painkillers (2% lidocaine), treatment with low-concentration antiseptic ointments, and the use of foam aerosols. If erosion does not heal for a long time, keratoplasty can be used.
Radiation damage to the oral mucosa
Radiation injury is often an occupational injury due to non-compliance with radiation therapy. All radiation injuries are called radiomucositis.

Etiology of radiation damage to the oral mucosa
The etiology of radiation injuries includes:
inadequate exposure to radioactive substances;
non-compliance with the techniques and rules of radiation therapy (radiography, gamma irradiation, radio irradiation).
Clinic of radiation injuries of the oral mucosa
The clinical picture of radiation injuries is progressive and dynamic. The clinic of radiation injuries has several periods.
The first period of radiation damage to the oral mucosa is observed in the first hours after injury. Patients complain of dry mouth, loss of taste and sensitivity.
Period 2 (period of well-being) is characterized by both subjective and objective facts. There are no complaints, the doctor will not notice anything during the examination in the second period.
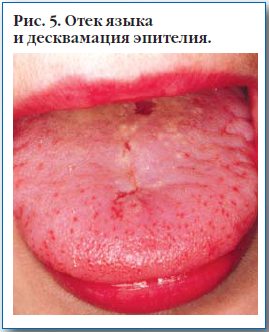
Period 3 – the peak period. The mucous membrane of the oral cavity is hyperemic, swollen, loses its shine, thickens, becomes dry, and folds appear. The gingival papillae begin to swell. Bleeding gums are pronounced. On the mucous membrane of the cheeks, the back of the tongue, and the hard palate - desquamation of the epithelium with the formation of erosions. Erosion due to radiation damage to the oral mucosa is covered with necrotic plaque. Erosion can have different shapes and lengths. In the worst case, necrosis can reach the muscle layer. Salivation increases, but the saliva is white and viscous, with an unpleasant odor.
Radiation damage to the oral mucosa can occur as a primary chronic process, when the mucous membrane is constantly exposed to radioactive substances, or chronicization of acute radiation damage can occur.

Treatment of radiation injuries of the oral mucosa
Treatment of radiation injuries of the oral mucosa is primarily aimed at increasing the body's resistance to radiation exposure, reducing the permeability of blood vessels, and slowing down radiochemical reactions. Therefore, patients are prescribed antihistamines, calcium supplements, and B vitamins. It is recommended to rinse the mouth with weak antiseptic solutions and carry out a complete thorough sanitation of the oral cavity. If there are metal orthopedic structures, such patients are recommended to replace the metal structures with ceramic or plastic ones. Anesthesia of the mucous membrane is carried out with the help of weak warm applications with analgesics, ointments aimed at regeneration, and within 2-3 months the positive dynamics of treatment will be noticeable.
As can be seen from the article, traumatic lesions of the oral mucosa are a fairly common pathology in practice, so the main task of a dentist is not only correct diagnosis, but also high-quality treatment in order to help a person.
You will always find new and interesting information on all sections of dentistry on our website .







