Progression of periodontal disease
Machine translation
Original article is written in RU language (link to read it).
The purpose of this article is to expand the understanding of the mechanisms of development of periodontal diseases, the transition from one stage of the disease to another. It is important to understand that gingivitis is rarely an independent disease; it is the initial form of periodontal disease, or it occurs against the background of one of the forms of periodontitis.
Detailed and scientifically based information on surgical and non-surgical methods of treating periodontitis is presented in the online course Periodontitis: surgical and non-surgical methods of treatment .
The initial stage of periodontal disease
Gingivitis is an inflammatory gum disease that develops due to the influence of a combination of various local and systemic factors. The main distinguishing feature of gingivitis, as an independent disease, is the absence of destruction of the periodontal attachment.
The first initial symptoms may appear several days after the next accumulation of microbial plaque on the surface of a healthy gum. The triggering of inflammation is the result of the influence of an antigenic substance in the area of the gingival sulcus.

Figure 1. Initial manifestations of periodontal disease.
Visually, the gums look absolutely healthy. The first manifestations of the disease can be stated only at the level of pathohistological examination.
In response to the accumulation of waste products of pathological microorganisms in dental plaque in the area of the gingival sulcus, connective epithelial cells trigger the production of a chemotoxin.
The accumulation of chemotoxin attracts polymorphonuclear leukocytes to the initial lesion area, and bacterial polysaccharides cause activation of the complement system. As a result of these processes, degranulation of mast cells occurs, which results in the release of histamine, prostaglandins and leukotriene, mediators of inflammation. The latter cause the following changes in surrounding tissues:
vascular permeability increases,
vasodilation, local vasodilation,
the adhesiveness of molecules increases,
leukocytes leave the vascular bed.
Characteristics of initial damage to periodontal tissues
The development of typical vascular vasculitis (against the background of increased permeability of their walls, progressive loss of perivascular collagen), which are located under the connective epithelium.
The volume of gingival fluid gradually increases.
Extravascular fibrin is produced.
There is disorganization of the attached epithelium in the area of the coronal zone.
Polymorphonuclear leukocytes accumulate in the gingival sulcus in the area of the attached epithelium, where, with the support of complement, phagocytosis of pathological microorganisms and their metabolic products is observed.
At the initial stage of inflammation, only isolated plasma cells and lymphocytes are histologically noted.

Figure 2. Clinic of periodontitis in the area of the anterior teeth.
Progression
The initial clinical symptoms of gingivitis appear as soon as the inflammatory mechanisms have started; they do not have clear boundaries, and the constant presence of plaque is a prerequisite. A gradual increase in vascular permeability also causes an increase in the intensity of plasma protein release.
Polymorphonuclear granulocytes continue to penetrate in large numbers into the area of the connective epithelium. The result of this process is a gradual loosening of the bottom of the gingival sulcus, and the basal cells begin to proliferate laterally.
Active macrophages continue to produce cytokines and collagenase, resulting in an accumulation of T-lymphocytes released from the vascular bed. An infiltrate is formed in the connective tissue of the gingival sulcus, consisting mainly of T-lymphocytes; it occupies from 10 to 15% of the volume of the entire free gum. There is a progressive decrease in the network of collagen fibers, a rapid increase in basal cells and attached epithelium.
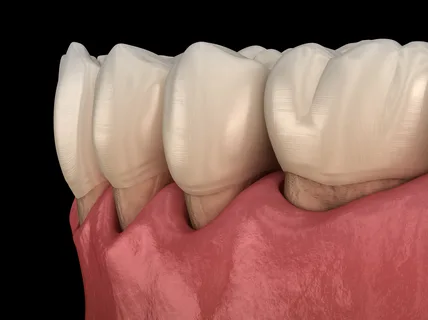
Figure 3. Clinic of periodontitis in the area of chewing teeth.
Due to damage to the microcirculatory system, initial clinical symptoms appear:
edema,
redness,
bleeding when probing the gingival sulcus.
The first clinically significant damage is diagnosed approximately a week after the onset of the first pathological reactions. The duration of the early inflammatory stage is not constant, it can be 3 weeks, or maybe longer.
Against the background of the continued constant presence of plaque in the gum tissue, clinically more pronounced disorders develop over time.
There is lateral proliferation of the connective epithelium into the infiltrated connective tissue of the gums.
Microulceration is observed between the strands of epithelium at the microscopic level.
Plaque gradually moves under the gingival margin, where a subgingival accumulation of microorganisms develops, the waste products of which directly affect the connective tissue.
The following cell populations predominate in connective tissue: macrophages, plasmacytes, lymphocytes. In damaged connective tissue structures of the periodontium, plasmacytes and B-lymphocytes predominate.
The gum condition described above, the gingivitis stage, is the most common and can be diagnosed in most adult patients. The next stage in the progression of the pathological process is periodontitis.
Development of periodontitis
Periodontitis is the next stage in the progression of the pathological process in the gum tissue, an inflammatory disease of the periodontal tissues, which has a polyetiological genesis, which is accompanied by the destruction of the periodontal ligament, increasing destruction of bone tissue, causing future tooth loss.
General characteristics of chronic simple periodontitis
It is a type of inflammatory periodontal disease and can be considered as the next stage of gingivitis.
It is characterized by destructive periodontal lesions.
Generalization of inflammatory and immunopathological processes in periodontal tissues.
Gradual lysis of alveolar bone.
Destruction of the periodontal ligament.
Loss of collagen fibers.
Fibrosis in distant areas.
Formation of periodontal pockets.
Gradual replacement of bone marrow with fibrous connective tissue.
Pathogenesis
Against the background of the constant presence of subgingival dental plaque, the aggression of the latter only increases over time, and a weakening of the protective capabilities of periodontal tissues is observed.

Figure 4. Local manifestations of gingivitis.
The triggering of attachment loss is directly determined by a shift in the microbiological composition of subgingival plaque towards anaerobic flora. The level of attachment loss corresponding to the bottom of the pathological pocket reaches the enamel-cementum interface and extends apically. Histologically, proliferation of thinned pocket epithelium in the form of epithelial strands is observed, along with apical displacement of the junctional epithelium on the surface of the cementum.
In the area of the periodontal pocket, microorganisms reach damaged cement through resorption lacunae. The destruction of bone tissue is carried out by osteoclasts, which are activated under the influence of an increase in the amount of interleukins and prostaglandins.
Clinical manifestations
As chronic simple periodontitis develops, diagnostic radiography can reveal uniform horizontal resorption of alveolar bone.
In order for the progression of the inflammatory process to go in the direction of chronic complex periodontitis, it is necessary to add such an unfavorable factor as occlusal trauma.
Chronic complex periodontitis
Occlusal trauma is a set of structural and functional damage to periodontal tissues caused by pathological occlusal load.
It is necessary to distinguish between acute occlusal trauma, which is associated with externally directed forces, and chronic, caused by internal occlusal disorders (parafunctions, supercontacts).
In turn, chronic occlusal injury is divided into two types: primary and secondary.

Figure 5. Bone resorption.
Primary is determined by the following factors:
non-physiological, excessive loads that affect the teeth, against the background of the absence of an inflammatory component, having a healthy intact periodontium.
the application of this force can extend in one direction to the periodontium, then this is an orthodontic force, or in several directions at once, then these forces are called rocking forces.
Secondary occlusal trauma is characterized by the traumatic effects of excessive loads against the background of the existing inflammatory process in periodontal tissues.
In the course of laboratory studies, it was possible to find out that supercontacts and increased occlusal load are prerequisites for the development of periodontal diseases, since they create favorable conditions for the penetration of the inflammatory component into deep periodontal structures.
A distinctive feature of complex periodontitis associated with exposure to occlusal trauma is the vertical type of alveolar bone resorption and the formation of intraosseous defects.
The online course Advanced Treatment of Periodontal Diseases is devoted to the principles of treatment of periodontal diseases .


