Decoupling With Time: A Solution to the Problem of the Hierarchy of Bondability
Abstract
Polymerization dynamics, which govern the movement of composite restoratives as they cure, dictate that shrinkage occurs in the direction of the most bondable surface or, in larger volumes, toward the center mass of the material. When polymerizing, composite shrinks toward the wall or walls of the preparation that are the most mineralized and dry and away from thewalls that are the most moist and organic as dictated by the hierarchy of bondability. Immediately sealing the dentin with a dentin bonding system after preparation, applying a thin coating of resin, and allowing the developing dentin hybrid layer to mature for an appropriate amount of time improves the overall bond strength significantly and prevents the shrinkage stress created by larger overlying volumes of composite from causing debonding in a process known as decoupling with time. Additional techniques, such as deep margin elevation, stress-reduced direct composite layering, and the placement of fiber reinforcement also leverage decoupling with time to improve bond strengths. This article explores the development and use of these and other techniques to improve bond strengths to dentin, discusses the impact of the hierarchy of bondabiliy on composite failure, and presents the biomimetic restorative dentistry protocols that incorporate this information to create restorations that possess a long-term seal to prevent reinfection, maintain pulp vitality, maximize the preservation of tooth structure, and minimize residual stresses in the tooth/restoration complex.
You have the opportunity to gather more in-depth information about biomimetic approach in our course "The biomimetic concept: composite restoration protocols".
Learning objectives
Describe the techniques of immediate dentin sealing, resin coating, deep margin elevation, stress-reduced direct composite layering, and fiber reinforcement.
Summarize the concepts of decoupling with time and the hierarchy of bondability.
Discuss the maximization of dentin bond strength and the causes of composite failure regarding polymerization dynamics.
Discuss the protocols of biomimetic restorative dentistry that decouple with time to neutralize the hierarchy of bondabilty and increase the longevity of composite restorations.
Twenty-three years ago, a team of researchers from the University of Minnesota set out to answer the question, "Do dental composites al-ways shrink toward the curing light?" and found that the answer was "No." Dental composites shrink toward the most bondable surface that they are connected to or toward the center of their mass during the first 5 to 30 minutes after placement. Knowledge regarding how composites move during curing is referred to as the science of polymerization dynamics. The volume of a polymerizing mass of composite greatly influences the direction of its movement as it shrinks. The larger the volume ofa light-cure composite, the more the shrinkage is directed to the center of its mass and away from the walls of the preparation.
A primary goal of biomimetic restorative dentistry protocols is to place small volumes of composite that move toward the developing dentin hybrid layer during their maturation. This positive dynamic movement can only occur if the initial volume of composite that is placed on top of the dentin bonding system is kept very thin (less than 1.5 mm) during the first 5 minutes of its polymerization reaction. This is one of the secrets to successful biomimetic restorative dentistry. Other protocols of biomimetic restorative dentistry that take advantage of polymerization dynamics to achieve long-term success include immediate dentin sealing, resin coating, deep margin elevation, stress-reduced direct composite layering, and polyethylene fiber placement.
Dentin Sealing, Resin Coating, and Deep Margin Elevation
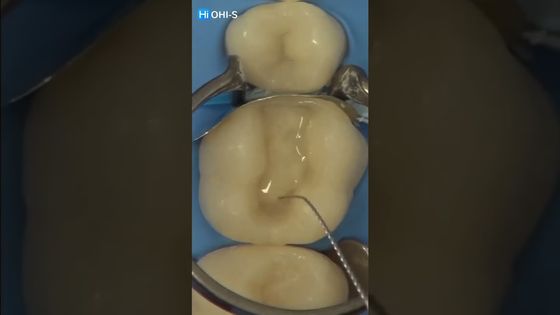
For every partial coverage restoration placed using biomimetic restorative dentistry protocols, there is a fundamental direct restorative component – the immediate sealing of the freshly prepared dentin. In immediate dentin sealing, the freshly prepared dentin is infiltrated with resin to create a hybrid layer that mimics the dentinoenamel complex, protecting it from bacterial leakage and the remnants of temporary cements. The companion concept of immediately placing a thin layer of microfilled flowable composite to protect the underlying hybrid layer is referred to as "resin coating." These two protocols were introduced in Japan and Europe in the mid-1990s. Immediate dentin sealing and resin coating procedures have been shown to increase the strength of the bond to dentin by 400%.
Introduced in 1998 by Dietschi and Spreafico, deep margin elevation is another biomimetic restorative dentistry protocol that leverages polymerization dynamics. Deep margin elevation is performed immediately after immediate dentin sealing and resin coating to restore subgingival defects. By executing deep margin elevation as a separate step, the volume of composite used subgingivally was reduced and allowed to remain unconnected to any larger masses of composite for a period of time. Deep margin elevation allows a strong bond to develop in this most difficult area to restore.
The concepts of immediate dentin sealing, resin coating, and deep margin elevation have been used and taught at the University of Geneva, Switzerland, for more than 20 years, and great successes using these three fundamental protocols in partial coverage restorations have been documented and published during that time. Why do these three techniques produce such a dramatic increase in the bond strength to dentin and, subsequently, the longevity of adhesive dentistry? Because traditional techniques used to bond partial coverage restorations (with or without subgingival defects) delayed the dentin bonding procedure until the time that the final restoration was placed. This reduced the potential bond strength by approximately 80% because it failed to allow the dentin hybrid layer enough time to mature in a stress-free environment. Enamel hybrid layers develop quickly because enamel is dry. However, dentin is moist and flexible, making it more difficult to encapsulate with the developing resin polymers of the dentin bonding system beingused. lt requires roughly twice as much time to develop a strong bond to dentin as it does to develop a strong bond to enamel, but when a mature bond to dentin is established, it is roughly twice as strong as the bond to enamel.
Decoupling With Time
Immediate dentin sealing, resin coating, and deep margin elevation all provide sufficient time for the dentin bonding system to create a mature hybrid layer that is better able to resist any shrinkage stresses associated with the resin cements or subsequent composite layers to which it is connected (ie, "coupled"). Therefore, by delaying or "decoupling" the bonded connection between the dentin hybrid layer and the subsequent restorative layers for a period of time, the maximum cohesive strength of the tooth/restoration complex can be achieved. This concept of first establishing a bonded seal of the dentin with a thin layer of resin and then, after a period of time, connecting or coupling the rest of the restoration to it has been referred to in the literature as "decoupling with time." Decoupling with time can help overcome the differences among the multiple types of dental hard tissue involved in bonding procedures. Those differences have been used to establish what is referred to as the "hierarchy ofbondability."
The Hierarchy of Bondability
The hierarchy of bondability dictates the direction of shrinkage of composite layers and the amount of stress that is concentrated on the developing dentin hybrid layer. When polymerizing, composite shrinks toward the wall or walls of the preparation that are the most mineralized and dry and away from the walls that are the most moist and organic.
The hierarchy of bondability is based on the science that has shown that preparations have multiple types of dental hard tissues that can be hybridized. These hard tissues have different percentages of mineral content, and that level of mineralization affects how easy or difficult it is to form a strong bond to each of them. Commonly encountered dental hard tissues ranked in the order of their mineral content from the most mineralized and dry to the least mineralized and moist include enamel, sound superficial dentin, sound intermediate dentin, affected superficial dentin, affected intermediate dentin, sound deep dentin, affected deep dentin, and infected deep dentin. The first six of these hard tissues can establish bonds in the range of 30 to 50 MPa if C-factor stresses are eliminated or delayed and a "gold standard" dentin bonding system is used. The last two hard tissues, affected deep dentin and infected deep dentin, can only achieve a bonded seal in the range ofl0 to 20 MPa. If the bond strengths of immediate dentin sealing and resin coating are allowed to be established during the first 5 to 30 minutes, greater durability of the bond to dentin is achieved under occlusal loading.
Because biomimetic restorative dentistry protocols that promote decoupling with time, including immediate dentin sealing, resin coating, and deep margin elevation, make all of the resin coated dentin surfaces equally bondable, the hierarchy of bondability is neutralized. The stresses from subsequent composite layers will not be concentrated on the deep dentin hybrid layer until the deep dentin hybrid layer's strength has been maximized. This secures the bond to that most critical part of the restoration, Immediate dentin sealing and resin coating result in a strong interface of two different materials that mimics the dentinoenamel complex.
Direct Decoupling Techniques
After immediate dentin sealing, resin coating, and deep margin elevation were introduced for indirect and semi-direct approaches, other techniques were developed to create direct adhesive restorations that had characteristics similar to those of the ''biomimetic" indirect restorations. These new techniques also incorporated decoupling with time in order to overcome the problems associated with the hierarchy ofbondability.
Separation
In 2000, Wilson and colleagues published a technique that introduced the word decoupling into the literature. Intended to prevent sensitivity after class II direct composite restoration in the posterior dentition, this decoupling protocol involved a permanent separation of the deepest 1-mm layer of composite from the more superficial 2-mm layers through the addition of an unbonded separating layer. The technique sealed the tooth and prevented the hydrodynamic movement of pulpal fluid that causes pain after dental restorations. However, because the bottom of the restoration was disconnected from the top, the biomechanical function of the tooth under loading was altered. This could lead to early tooth fractures and required retention forms similar to those of traditional cavity preparations.
Stress-Reducing Direct Composite Layering
In 2002, Deliperi and Bardwell introduced what would become known as the stress-reducing direct composite layering protocol. This technique also had the goal of preventing postoperative sensitivity, but it eliminated the need for retention and resistance forms in preparations. In the protocol, the dentin and the enamel were restored as two different substrates and in three different stages using a selective composite technique.
After immediate dentin sealing, the first stage of composite layering involved the replacement of the proximal/facial/lingual enamel shell. In the second stage, dentin replacement began with the placement of a 0.5-mm to 1.0-mm layer offlowable composite on the floor of the preparation over the filled adhesive of the bonding system used to hybridize the dentin. Then, after this initial thin increment of composite was created, the rest of the dentin was replaced using the same small volume increment technique to place 1.0-mm to 1.5-mm, wedge-shaped increments using slow-start pulse polymerization protocols, decreasing the C-factor ratio. The third stage involved replacing the occlusal surface via a successive cusp buildup protocol.
Although the stress-reducing direct composite layering protocol employed decoupling with time, the layers of the restorations were ultimately coupled from top to bottom instead ofbeing left disconnected in the manner of the protocol developed by Wilson and colleagues. The stress-reducing direct composite layering protocol could also be used for cusp replacing restorations
In 2004, a comparative study provided solid in vitro clinical evidence to support the use of decoupling approaches to improve the strength of bonds to dentin. The results indicated that the thinner the horizontal layers of composite placed, the higher the microtensile bond strength achieved in the deepest floor of the preparations. According to the data, a 1-mm horizontal layer achieved a microtensile bond strength of 30 MPa, whereas a 4-mm bulk-filled layer only achieved a microtensile bond strength of 11 MPa.
Then in 2014, a team from Brazil produced more in vitro support for the concept of decoupling using finite elemental analysis at the University of Tennessee. The conclusions of these studies reinforce that maximizing the bond strength of the adhesive layers nearest the pulp is best accomplished by placing multiple horizontal layers of small volume.
Polyethylene Fiber
Another decoupling technique involves placing ultra-high molecular weight woven polyethylene fibers into the first thin 0.5- to 1.0-mm layer of flowable microfilled composite coupled to the dentin bonding system. This innovation was developed at the Selcuk University in Turkey and the Tokyo Medical and Dental University in Japan under the direction of Belli and Inokoshi, respectively. The technique was shown to eliminate the stress to the dentin hybrid layer that causes microleakage. These experiments were confirmed in 2007 by El-Mowafy and colleagues and in 2009 by Ozel and colleages. By placing polyethylene fiber in the first 1 mm of composite, an effective decoupling of the lowest sealing layers of composite from the overlying layers of composite was achieved. In 2008, Erkut and colleagues used scanning electron microscope visualization to demonstrate the mechanism of stress relief, which involved the fibers separating as the small intertwining masses of composite moved in two different directions. In 2020, this technique of "decoupling with fiber" was confirmed by Sadr and colleagues through in vitro tests that permitted real-time visualization of the fibers acting as a decoupling mechanism using optical coherence tomography.
Maximizing Dentin Bond Strength
Each of the aforementioned decoupling protocols adds to the time that it takes to complete the restoration. This extra time for the polymerization reaction allows the dentin hybrid layer to mature in its seal and its strength. Every restorative procedure takes time to perform, including both amalgam placement and composite placement. Is delivering a direct adhesive composite restoration or an indirect bonded restoration worth the added time that it takes to place? Only if there is a benefit to the patient regarding better outcomes and greater longevity. This is the goal of the "post-amalgam era."
The average age of a large composite restoration in the United States is a little more than 5 years. Many protocols utilizing biomimetic approaches have been developed during the last 25 years that have been able to extend the life of large composite restorations to more than 20 years. By combining the best decoupling techniques with the concepts of polymerization dynamics and time allowance for the hybrid layer to mature, restorations can be created that act like natural tooth structure and that are strongly connected from side to side, top to bottom, and front to back with cohesive strengths in the range of 30 to 50 MPa-the same as the natural tooth components.
In a summary of biomimetic restorative dentistry protocols that was published in Inside Dentistry in 2017, the authors listed 18 different protocols that have been shown to maximize the bond to dentin in the developing hybrid layer. Without employing stress reducing protocols that permit decoupling with time, it is impossible to achieve longterm successes in structurally compromised teeth with large defects from decay and fracture. Maximum dentin bond strengths are needed to achieve the goals of biomimetic restorative dentistry, which include establishing a long-term seal of dental hard tissues to prevent reinfection under the restoration, maintaining pulp vitality, maximizing the preservation of tooth structure, and minimizing residual stresses in the tooth/ restoration complex.
Composite Failure
Why do large non-stress-reduced composite restorations fail? They fail because of recurrent decay, fracture of the tooth, and/or fracture of the restoration. All three of these failure modes are a manifestation of the stresses of polymerization that in the first hours of placement resulted in either weakening of the dentin hybrid layer, residual strain in the remaining tooth structure, internal stress in the polymer networks in the large composite mass, or a combination of these conditions. Although all of these failure modes require repair or replacement, recurrent decay often leads to pulpal infection, which may cause pulpal necrosis. A major goal ofbiomimetic restorative dentistry is to prevent this type of failure mode. Therefore, priority is given to avoiding polymerization stress on the maturing dentin hybrid layer.
Adhesive dentistry in large defects could be expressed as a simple relationship between dentin bonds and the polymerization stress caused by composite shrinkage. If a dentin bond can withstand the stresses applied to it during its initial formation, then it can better withstand the stresses of occlusion. In 1984, Davidson and colleagues were the first to study the development of composite-dentin bond strength in relation to polymerization shrinkage stress as a function of the polymerization time.
By utilizing biomimetic restorative dentistry protocols from the published scientific literature, occurrences of superficial clinical failure modes, such as the chipping ofreplaced enamel, can be reduced greatly for decades, and the occurrence of catastrophic/ biologic failure modes, such as those involving dentin and pulpal vitality, can be almost completely eliminated.
Biomimetic Restorative Dentistry Protocols
There are seven main protocols used in biomimetic restorative dentistry that help to neutralize the hierarchy ofbondability and permit decoupling with time to maximize the bond strength to dentin:
Create a peripheral seal zone inside the dentinoenamel complex that is free of carious dentin by using caries detecting dye. The dye's differential staining will allow the hard tissues that will present the most difficulty in establishing the dentin hybrid layer to be visualized and then treated in ways to maximize their seal and bonded strength.
Use an immediate dentin sealing technique that can establish a hybrid layer with a microtensile bond strength in the 30 to 50 MPa range.
Resin coat the immediately sealed dentin with a 0.5-mm layer of microfilled or nanofilled flowable composite to increase the thickness of the adhesive layer of the dentin bonding system.'
Allow the dentin hybrid layer 5 to 30 minutes to mature before placing an overlying increment with a thickness greater than 1.5 mm.
When the amount of dentin to be replaced is greater than 1.5 mm in thickness, use a stress-reducing direct composite layering technique to restore the dentin and then the enamel separately.
When vertical defects are deeper than 4 mm, use a deep margin elevation technique.
Incorporate polyethylene and fiber glass fibers to relieve polymerization stresses to the hybrid layer and improve fracture resistance under occlusal loading.
The use of all or some of these protocols results in the development a highly bonded foundation. This foundation, which has become known as the ''bio-base" at the Academy of Biomimetic Dentistry in the United States and in the Philippines, is an intrinsic part of every biomimetic restorative dentistry restoration. The bio-base eliminates the need for traditional external ferrule.
All of the protocols that occur after immediate dentin sealing (ie, 3 through 7) take time to perform. During the time that it takes to perform these five protocols, something very critical is happening, The free radical polymerization reaction that is forming the hybrid layer in dentin is completing 80% to 90% of its potential monomer conversion, which directly relates to it strength. The conversion of monomers to oligomers, then to small polymers, and finally, to larger polymers takes 5 to 30 minutes. The adhesive layer in the dentin bonding system needs to be a minimum of 80 µm thick to polymerize because 10 to 20 µm of its thickness will be inhibited from conversion by the air inhibiting of the dentin bonding system initiators that cause the start of monomer chain formation.
Immediate dentin sealing may be performed with either a filled, lightly filled, or unfilled dentin bonding system to achieve the goal of high bond strengths. However, the combination of a filled dentin bonding system and a flowable composite for the resin coating creates an ideal gradient of elasticity that can best absorb stresses from polymerization and occlusal loading. The concept of making an unfilled adhesive layer thicker by adding a flowable composite as a resin coating or "filled adhesive" is a proven biomimetic restorative dentistry protocol. The process of resin coating also reduces the chance of pulpal fluid transudations turning from nanoleakage into microleakage due to perforations of the adhesive layer of the dentin bonding system.
There are additional details about adhesion and bonding you can obtain in our course "Modern adhesion".
Discussion
For the overlying composite to not adversely affect the strength of the hybrid layer, the polymerization dynamics (ie, directional movements) of the composite layers need to be understood in terms of the configuration of the tooth preparation and the volume of the composite used, The configuration of the defect in the tooth and the overall volume of the restoration both have an effect on the amount of stress associated with the polymerization of the different composite layers in the restoration.
Configuration factor or "C-factor;' which was established in the mid to late 1980s by Davidson, Feilzer, and de Gee, refers to the ratio of a restoration's bonded to unbonded surfaces. When composite was bonded to only one surface, the masses of composite shrank in mostly one direction and were not very stressful to the bond. However, when 3D cavities were filled, the shrinkage toward multiple walls caused so much stress that the bonds of the dentin hybrid layers established with dentin bonding systems that had strengths in the 18 MPa range failed. This caused gaps in the deepest parts of the preparations that were closest to the pulp. None of the early dentin bonding systems were able to achieve bonds to flat surfaces (low C-factor) in the biomimetic range of 30 to 50 MPa until the late 1980s and early 1990s.
One technique pioneered by Fusayama in the 1980s demonstrated some success in higher C-factor preparations using a chemical cure dentin bonding system and a chemical cure composite that had a 5-minute gel point delay. This 5-minute delay in the polymer formation allowed more time for the dentin bonding system to mature; therefore, the polymerization stresses from the volume of composite were delayed. Unfortunately, the successes of this "directed shrinkage" technique were not consistent, and there was reported sensitivity from sealed gaps filled with pulpal fluid, which caused pain during function from hydrodynamic movement of the fluid.
Why was the failure of these early techniques always associated with debonding at the pulpal floor and not at the enamel margin? Because the movement of the composite shrinkage was toward the enamel and away from the pulpal floor as dictated by the hierarchy of bondability. This occurred because it is easier for a hybrid layer to develop to highly mineralized dental hard tissues such as enamel and superficial dentin than it is for it to develop to intermediate dentin, deep dentin, and root dentin, which require more time to develop a strong bond.
Dentin bonds can achieve strengths in the 50 to 60 MPa range, which are potentially twice the strong as bonds to enamel in the 25 to 30 MPa range. However, within the first 3 minutes of polymerization, the early bond strength to enamel is twice as strong (16 MPa) as the early bond strength to dentin (8 MPa).11 Dentin is only approximately 50% hydroxyapatite, whereas enamel is more than 95% hydroxyapatite, so it takes longer for the bond to dentin to mature. Dentin is also approximately 30% collagen and 20% water, which makes it "slippery" and more difficult for the enveloping polymers to "grab ahold of" than the dryer enamel. If you connect or couple an overlying composite mass of a larger volume too soon, then the dentin hybrid layer can be stretched to a weaker connection or even broken during the first hours of the polymerization reaction. This is because the polymerization of the overlying composite is stretching the dentin hybrid layer toward its center of mass and away from the dentin.
Another method developed during the 1980s that attempted to overcome the problem of polymerization shrinkage was the "semi-direct'' technique. This concept involved a composite inlay or onlay that was polymerized outside of the mouth and then cemented into place using a dentin bonding system and a resin cement applied at the same time. Removing the large volume of composite from the cavity during shrinkage was a good idea, but the clinical results were not great. Again, this was due to the differences in the bondable surfaces when the dentin bonding system was applied to the semi-direct restoration at the same time as the resin cement. Delaying dentin bonding instead of immediately sealing the freshly prepared tissues decreased the bond to dentin to less than 11 MPa. This is because the movement of the shrinking cement layer moved in accordance with the hierarchy ofbondability. It shrunk toward the most bondable surface at the moment of coupling, which was the dry intaglio surface of the composite inlay or onlay. The weaker surface was the moist and flexible dentin hybrid layer that was being developed at that time.
Although the directed shrinkage and semidirect techniques that were developed were found wanting, new approaches fefe being developed that were successful. The new techniques of immediate dentin sealing, resin coating, and deep margin elevation to seal the preparation before the impression was made were game changers that led to more protocols that decoupled with time and neutralized the hierarchy of bondability. The resin coating or "dual bonding" technique was shown to eliminate the gaps on the pulpal and axial walls of restorations and increase the bond strength to dentin by as much as 400% to the range of 50 to 60 MPa when using a gold standard dentin bonding system.
Further testing revealed that delayed composite placement of the direct components of direct and indirect restorations were improved with decoupling with time because it takes time for the chemical reactions of the dentin bonding system to occur. All biomimetic restorative dentistry techniques delay the coupling of the dentin hybrid layer to larger volumes of shrinking composites for a period of time. The time that the dentin hybrid layer is allowed to mature can range from 5 minutes for shallow stress-reducing direct composite restorations to 2 weeks for indirect final restorations that are bonded to bio-bases.
Conclusion
Having small volumes of composite move toward the dentin hybrid layer as they cure is the primary goal of biomimetic restorative dentistry protocols. This ensures that large layers of composite that are thicker than 1 mm are not connected to the developing hybrid layer during at least the first 5 minutes of its polymerization reaction. The hierarchy of bondability dictates the direction of the movement of the composite. Thin layers move toward the tooth and improve the strength of the hybrid layer. Thick layers move away from the tooth and toward the center of their mass, which can weaken or break the hybrid layer.1 When the dentin hybrid layer is allowed to fully mature by decoupling with time, then all of the surfaces in the hierarchy ofbondability become as bondable as enamel and can establish high bond strengths in 3 minutes. With the hierarchy of bondability neutralized by decoupling with time, tooth restoration becomes very predictable and all of the goals ofbiomimetic restorative dentistry can be achieved.
List of authors:
David Alleman
Davey Alleman
Simone Deliperi
Jorje Aravena Dias
Leandro Martins
Filip Keulemans
References
1. Versluis A, Tantbirojn D, Douglas WH. Do dental composites always shrink toward tl!e light? J Dent Res. 1998;77( 6):1435-1445.
2. Satoh M, Gotoh H, Inai N, et al, How to use the "liner bond" system as a dentin and pulp protector in indirect restorations.Adhesive Dentistry.1994;12(1):41-4 7.
3. Bertschinger C, Paul SJ, Lutl!y H, Scherrer P. Dual application of dentin bonding agents: effect on bond strengfu.Am J Dent.1996;9(3):115-119.
4. Jayasooriya P, Pereira P, Nikaido T, Tagami J. Efficacy of a resin coating on bond strengtl!s of resin cement to dentin. J EsthetRestor Dent 2003;15(2):105-113.
5.Magne P, Kim TH, Cassione, Donavan TE. Immediate dentin sealing improves bond strengtl!s of indirect restorations. J Prosthetic Dent. 2005;94(6):511-519.
6. Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthet Dent. 1998;10(1):47-54,
7. Magne P, Spreafico R. Deep margin elevation: a paradigm shift. Am J Esthet Dent 2012;2(2):86-96.
8. SarfatiA, Tirlet G. Deep margin elevation versus crown lengtl!ening: biologic widtl! revisited Int J of Esth Dent. 2018;13(3)334-356,
9. Bresser RA, Gerdolle D, van den Heijkant IA, et al. Up to 12 years clinical evaluation ofl97 partial indirect restorations with deep margin elevation in posterior region. J Dent. 2019;91:103227.
10. Bottacchiari S. Composite Inlays and Onlays: Structural Periodontal andEndodonticAspects. Milan, Italy: Quintessenza Edizioni; 2016.
11. Irie M, Suzuki K, Watts DC. Marginal gap formation of light-activated restorative material: effects of immediate setting shrinkage and bond strength. Dent Mater. 2002;18(3):203-210.
12. Van Meerbeek B, De Munck J, Mattar D, et al. Mictotensile bond strengths of an etch&rinse and self-etch adhesive to enamel and dentin as a function of surface treatment Oper Dent. 2003;28(5):647-660.
13. Cho M, Dickens S, Hae J, et al. Effect of interfacial bond quality on the direction of polymerization shrinkage flow in resin composite restorations. Oper Dent. 2002;27(3):297-304.
14. Nakajima M, Ogata M, Okuda M, et al. Bonding to caries-affected dentin using self-etching primers. Am J Dent.1999;12(6):309-314.
15. Yoshiyama M, Tay F, Torri Y, et al. Resin adhesion to carious dentin.AmJ Dent. 2003;16(1):47-52.
16. Doi J, Itota T, YoshiyamaM, etal. Bonding to root caries by a self-etching adhesive system containing MDPB. AmJ Dent. 2004;17(2):89-93.
17. Sattabanasuk V, Shimada Y, Tagami J. The bond of resin to different dentin surface characteristics. Oper Dent. 2004;29(3):333-341.
18. Sattabanasuk V, Burrows MF, Shimada Y, Tagami J. Resin adhesion to caries-affected dentine after different removal methods.Aust Dent J. 2006;51(2):162-169.
19.NikaidoT, Kunzehnann K, Chen H,etal.Evaluation of thermal cycling and mechanical loading on bond strength of a self-etching primer system to dentin. Dent Mater. 2002;18(3):269-275.
20. Alleman D, Nejad M, Alleman D. The protocols of biomimetic restorative dentistry: 2002-2017. Inside Dentistry. 2017;13(6):64-73.
21. Kishikawa R, Koiwa A, Chikawa H, et al. Effect of cavity form on adhesion to cavity floor. Am J Dent. 2005;18( 6):311-314.
22. Magne P, Belser U. Bonded Porcelain Restorations in theAnterior Dentition:ABiomimeticApproach. Chicago, IL: Quintessence; 2002:38-42.
23. Wilson NH, CowanAJ, Unterbrink G, et al.A clinical evaluation of class II composites placed using a decoupling technique. J Adhes Dent. 2000;2( 4);319-329.
24. Brannstrom M. Dentin and Pulp in Restorative Dentistry. London, England: Wolfe Medical; 1982:87-93. 25. Deliperi S, Bardwell D. An alternative method to reduce polymerization shrinkage in direct posterior composite restorations. J Am Dent Assoc. 2002;133:(10):1387-1398.
26. Deliperi S, Bardwell D N. Clinical evaluation of direct cusp coverage direct posterior composite resin restorations. J Esthet Rest Dent. 2006;18(5):256-267.
27. Nikolaenko S, Lohbauer U, Roggendorf M, et al. Influence of c-factor and layering technique on micro tensile bond strength to dentin. Dent Mater. 2004;20(6):579-585.
28.BicalhoAA,PereiraRD,ZanattaRF,etal.Incremental filling technique and composite material- part 1: cuspal deformation, bond strength and physical properties. Oper Dent. 2014;39(2):E71-E72.
29. Belli S, Inokoshi S, Ozer F, eta!. The effect ofadditional enamel etching andaflowable composite to the interfacial integrity of class II adhesive composite restorations. Oper Dent. 2001;26(1):70-75.
30. Belli S, Donmez N, Eskitascioglu G. The effect of c-factor and flowable resin or fiber use at the interface of microtensile bond strength to dentin. J Adhes Dent. 2006;8( 4):24 7-253.
31. Belli S, Orugoglu H, Yildirim C, Eskitascioglu G. The effect of fiber placement of flowable resin lining on microleakage in class II adhesive restorations. J Adhes Dent. 2007;9(2):175-181.
32.El-MowafyO,El-BadrawyW,Eltanty A, etal. Gingival microleakage of class II resin composite restoration with fiber inserts. Oper Dent. 2007;32(3):298-305.
33. Ozel E, Soyman M. Effects of fiber nets, application techniques and flowable composites on microleakage and the effect of fiber nets on polymerization shrinkage in class II MOD cavities. Oper Dent. 2009;34(2):l,74-180.
34. Erkut S, Gulsahi K, CTaglar A, et al. Microle"akage in overflare<l root canals restored with different fiber reinforced dowels. Oper Dent. 2008;33(1):92-101.
35. Sadr A, Behnoush-B, Hayashi J, et al. Effect ofliber reinforcement on adaptation and bond strength of a bulk-filled composite in deep preparations. Dent Mater. 2020;36(4):527-534.
36. Magne P. Composite resins and bonded porcelain: the post amalgam era? J CalifDentAssoc. 2006;34(2):135-14 7. 37. Urabe I, Nakajima M, Sano H, Tagami J. Physical properties of the dentin-enamel junction region. Am J Dent. 2000;13(3):129-135.
38. Versluis A, Tantbirojn D, Pintado M, et al. Residual shrinkage stress distributions in molars after composite restoration.Dent Mater. 2004;20(6):554-564.
39. UnterbrinkGL, LlebenbergWH. Flowable resin composites as "filled adhesives": literature review and clinical recommendations. Quintessenceint.1999;30( 4):249-257.
40. Davidson C, de Gee A, Feilzer A The competition between the composite-dentin bond strength and the polymerization contraction stress. J Dent Res. 1984;63(12):1396-1399.
41.Krejci I,Stavridakis M. New perspectives on dentin adhesion - differing methods of bonding. PractPeriodontics AesthetDent. 2000;12(8):727-732.
42. Alleman D, Magne P.A systematic approach to deep caries removal end points: the peripheral seal concept in adhesive dentistry. Quintessence Int. 2012;43(3):197-208.
43. Deliperi S, Alleman D. Stress-reducing protocol for direct composite restorations in minimally invasive cavity preparations. PracProcedAesthetDent. 2009;21(2):el-e6.
44. Deliperi S, Bardwell D, Alleman D. Clinical evaluation of stress-reducing direct composite restorations of structurally compromised molars: a 2-year report. Oper Dent. 2012;37(2):109-116.
45. Fennis W, TezvergilA, Kuijs R, et al. In vitro fracture resistance of fiber reinforced cusp-replacing composite restorations. Dent Mater. 2005;21( 6):565-572.
46. Deliperi S,Alleman D, Rudo D. Stress-reduced direct composites for the restoration of structurally compromised teeth: fiber design according to the "wallpapering" technique. Oper Dent. 2017;42(3):233-243.
47. Soares LM, Razaghy M, Magne P. Optimization oflarge MOD restorations: composite resin inlays vs. short fiber-reinforced direct restorations. Dent Mater. 2018;34( 4):587-597.
48. Sary T, Garoushi S, Braunitzer G, et al. Fracture behavior of MOD restorations reinforced by various fibre-reinforced techniques- an in vitro study. J Mech Behav BiomedMater. 2019;98:348-356.
49. Davidson C, de Gee A Relaxation of polymerization contraction stress by flow in dental composites. J Dent Res.1984;63(2):146-148.
50. Feilzer AJ, de Gee AJ, Davidson CL. Setting stress in composite resin in relation to configuration of the restoration. J Dent Res.1987;66(11):1636-1639.
51. Rueggeberg FA, Margeson DH. The effect of oxygen inhibition on unfille<l/fille<l composite ,y,,tem.JDentRes. 1990;69(10):1652-1658.
52. Sano H, Shono T, Takatsu T, HosodaH. Microporous dentin zone beneath resin-impregnated layer. Oper Dent. 1994;19(2):59-64.
53. Fusayama T. New Concepts in Operative Dentistry: Differentiating Two Layers of Carious Dentin and Using anAdhesiveResin. Chicago, Illinois: Quintessence; 1980.
54. Fusayama T.ASimplePain-FreeAIIhesiveRestorative System by Minimal Reduction and Total Etching. Tokyo, Japan: Ishiyaku EuroAmerica; 1993.
55. Diets chi D, Spreafico R Adhesive Metal Free Restoration. Chicago, IL: Quintessence; 1997
56. Dietschi D, Monasevic M, Krejci I, Davidson C. Marginal and internal adaptation of class II restorations after immediate ordelayedcompositeplacementJDent. 2002;30(5-6):259-269.
57. Dietschi D, Olsburg S, Krecji I, Davidson C. In vitro evaluation of marginal and internal adaptation of indirect class II composite restorations with different resinous bases.Eur JOral Sci. 2003;lll(l):73-80.
58. Aaka Y, Miyazaki M, Takamizawa T, et al. Influence of delayed placement of composites over cured adhesives on dentin bond strength of single-application self-etch systems. Oper Dent. 2006;31(1):18-24.
59. Fukegawa D, Hayakawa S, Yoshida Y, et al. Chemical interactionofphosphoric acidesterwithhydroxyapatite. J Dent Res. 2006;85(10):941-944.

Video
OHI-S
02 April 2024
Video
OHI-S
16 January 2024

Video
OHI-S
21 November 2023




