What is orofacial pain
Machine translation
Original article is written in RU language (link to read it).
Orofacial pain is a type of pain localized exclusively to the face and mouth. Due to the rich innervation of this anatomical area, there is a huge variety of factors and causes that cause facial pain. Just like any other pain, orofacial pain that is not cured within three months becomes chronic, which further complicates its treatment. Clinical studies have shown that the incidence of facial pain reaches 26% of cases. Moreover, as a result of a re-examination of study participants several years later, the presence of pain was confirmed by half of the patients, which proves the high level of chronicity of the process.
About the importance and relevance of this topic in the online course Module 2: Understanding orofacial pain .
Patients with complaints of pain in the facial area turn to specialists in various fields of medicine, which significantly complicates diagnosis. According to the International Classification, facial pain is associated primarily with a neurological nature; its main causes are considered to be neuropathies and neuralgia.
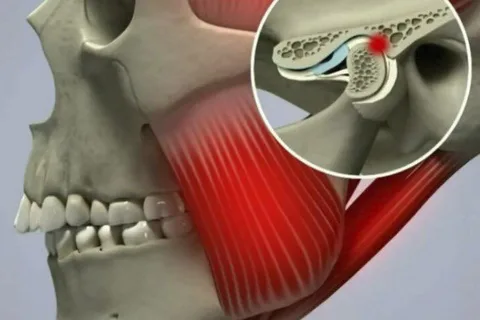
Rice. 1. Orofacial pain due to damage to the TMJ.
Classification
In 2019, the International Classification of Orofacial Pain ICOP was developed, which includes six groups of causes of facial pain. According to this classification, orofacial pain can be associated with diseases:
Dentoalveolar structures.
Muscle dysfunction.
Pathology of the temporomandibular joint, TMJ.
Damage to regional and cranial nerves, including trigeminal (trigeminal neuralgia) and glossopharyngeal.
Primary headache, cephalalgia, migraine.
Idiopathic orofacial pain.
The prevalence of dentoalveolar causes among all factors causing orofacial pain is more than 50%.
Diseases with 4–6 classification points are sometimes encountered in neurological practice. The most common mistake with facial pain is diagnosing trigeminal neuralgia, which entails the prescription of unnecessary long-term pharmacological treatment.
Among the causes of orofacial pain from 2-6 classification points, dysfunction of the temporomandibular joint (TMD) is most common, in approximately a quarter of patients. It is worth noting that according to the ICOP classification, there are two subtypes of TMD pain:
associated with muscle dysfunction, the source of pain is the muscles themselves;
caused by pathological disorders of the TMJ structures themselves.
General characteristics of orofacial pain in TMD
The pain can spread to the area of both jaws, radiate to the neck, shoulders, and can be localized in the ear and surrounding tissues. It can be permanent or provoked by opening the mouth during conversation, chewing, when muscle stretching occurs, activating myofascial trigger points.
May be accompanied by swelling and fatigue in the face.
Rarely, ear congestion, ringing, noise, and dizziness may occur.
Diagnosis of pain due to TMD involves taking a medical history, external examination and palpation. In practice, confirmation of the myofascial nature of orofacial pain is the reproduction of the patient’s usual pain during palpation, which torments him daily.
To confirm arthralgia, provocative tests are performed: palpation of the condylar processes while moving the jaw forward, lateral movements, alternately opening and closing the mouth.
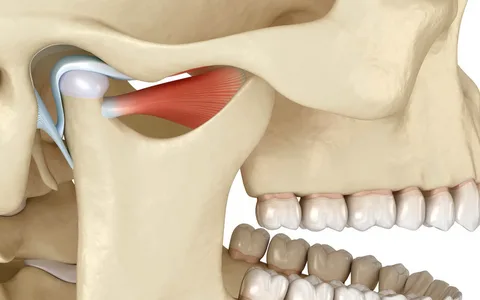
Rice. 2. Temporomandibular joint.
The main etiological factor in the occurrence of TMD was previously considered to be occlusion disorders. However, orthodontic treatment and normalization of the bite did not bring relief to patients. Today, occlusal disorders are considered as a predisposing factor for TMD, among them:
distal bite,
straight and open bite,
crossbite,
absence of five or more chewing teeth,
poor-quality old fillings, incorrectly performed prosthetics.
Predisposing factors also include the following:
traumatic injuries,
inadequate chewing load,
anxiety states,
depression,
excessive clenching of teeth over a long period of time.
Some scientists have suggested that the causes of facial pain in TMD are the result of disturbances in higher pain control systems. Therefore, pain syndrome with TMD can be considered the result of central sensitization.
Principles of treatment of orofacial pain in TMD
Use of non-steroidal drugs (NSAIDs).
Therapeutic exercise and relaxation techniques.
Manual therapy.
Cognitive behavioral therapy.
Treatment with mouth guards.
Orofacial pain due to damage to regional nerves
This cause of facial pain is much less common, but is the most common cause of overdiagnosis, and therefore should be studied in detail. Most often, orofacial pain is associated with damage to the glossopharyngeal and trigeminal nerves.
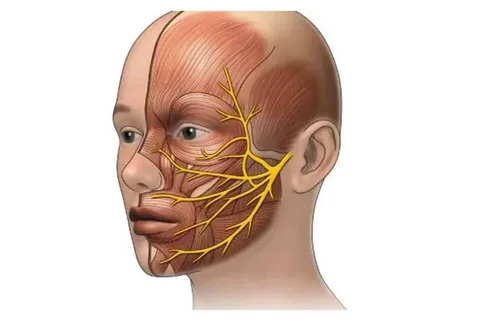
Rice. 3. Location of the branches of the trigeminal nerve.
Trigeminal neuralgia
Trigeminal neuralgia is a neuropathic, paroxysmal, often unilateral pain that occurs in the area and along the branches of the trigeminal nerve, characterized by an abrupt onset and the same ending. Patients describe the attack of pain as stabbing, cutting, compare it to an electric current; the pain occurs either spontaneously or is provoked by touch or chewing food.
Classification of trigeminal neuralgia
Classic, against the background of vascular-radicular conflict.
Secondary, associated with structural disorders, including multiple sclerosis, neoplasms.
Idiopathic, in the absence of compression of the nerve by any anatomical or other formations.
Diagnosis is made on the basis of a clinical interview; there are no special examination methods for making a diagnosis. It is important to conduct a differential diagnosis to exclude dentoalveolar causes of pain and magnetic resonance imaging to identify the source of compression characteristic of secondary TN.
If the neurological causes of orofacial pain are confirmed, therapy is carried out by a neurologist. At the first stage, preference is given to pharmacological treatment; if it is ineffective, a consultation with a neurosurgeon is recommended to consider the need for surgical intervention. Trigeminal nerve decompression provides long-term relief to the patient and ensures the functioning of the nerve.
Idiopathic orofacial pain, burning mouth syndrome
This pathology is characterized by a burning sensation that appears every day for several hours for several months, while during clinical diagnosis it is not possible to establish possible objective causes of the burning sensation.

Rice. 4. Burning mouth syndrome, burning sensation without external manifestations.
With SPR, pain is usually bilateral, of varying intensity, often localized at the tip of the tongue, and may be accompanied by dry mouth and disturbances in taste. More often, the syndrome appears in women, mainly during menopause.
Similar symptoms may be manifestations of candidiasis, lichen planus, iron deficiency anemia, hypovitaminosis of folic acid and B12, diabetes mellitus. According to the ICOP classification, these manifestations fall into point 1 of dentoalveolar pain, since the diagnosis of SPR can only be made in the absence of local and general causes of burning and pain. Therefore, a very important step is to carry out differential diagnosis with the above pathological conditions.
Atypical odontalgia
Atypical odontalgia (AO) is characterized by constant aching pain in the dental area, often in the area of an extracted tooth, in the absence of radiological and neurological disorders. Dental treatment does not help the pain disappear; the pain can spread to neighboring teeth. Establishing a correct diagnosis is very important in the early stages, as it will exclude unnecessary dental procedures, including surgical procedures.
conclusions
Pain in the face and mouth—orofacial pain—can have many causes. Dentoalveolar pain and myofascial pain are most common with TMJ dysfunction. Lesions of the trigeminal nerve can also provoke facial pain, but these diseases are rare, and their overdiagnosis is common, which provokes unnecessary and ineffective pharmacological treatment and surgical interventions.
The pathogenesis of orofacial pain is multifaceted; it is important to take into account neuropathies of regional nerves, central sensitization, pathology of descending pain control, as well as psychological and social factors. It is important to remember that chronic pain greatly affects a person's quality of life, and early diagnosis has a significant impact on the effectiveness of treatment.

Rice. 5. Life without pain.
The development of the ICOP classification of orofacial pain has stimulated new research into facial pain and the introduction of effective treatment methods.
A comprehensive understanding of TMJ dysfunctions and orofacial pain can be obtained in the online course Occlusion, TMJ Dysfunctions and Orofacial Pain A to Z.

/social-network-service/media/default/100980/ec233bde.png)
