Minimum intervention oral care: defining the future of caries management
Abstract
It is not uncommon that oral healthcare professionals and researchers interchange the use of the terms minimum/minimal intervention and minimally invasive dentistry. However, these terms apply to two different, but related, concepts. Minimum intervention dentistry, to be more appropriately addressed in this paper as minimum intervention oral care (MIOC), is an oral healthcare delivery framework that encompasses four interlinked clinical domains. These domains are: identifying disease - detection, longitudinal risk/susceptibility assessment, investigation, diagnosis and the development of a personalized care plan; prevention of lesions/control of disease – patient behaviour management, non-invasive remineralisation of the enamel and dentine, biofilm and diet control, micro-invasive sealants and infiltration techniques to arrest and reverse incipient lesions; minimally invasive operative procedures including selective carious dentine removal, the “5Rs” management of the tooth-restoration complex (review, refurbish, re-seal, repair and replace) amongst other restorative interventions; and tailored recall/review/re-assessment consultations. This framework includes that minimally invasive operative dentistry (MID), that although a critical operative clinical domain, should be viewed as one of the pillars of minimum intervention oral healthcare (MIOC), applied across all disciplines of restorative dentistry, not just caries management. The aim of this review is to clarify these differences and emphasize the importance of minimally invasive operative dentistry (MID) within the context of minimum intervention oral care (MIOC). MIOC is applicable to all disciplines within restorative dentistry, including clinical caries management.
Introduction
The term minimum/minimal intervention dentistry was introduced during the 1980s. Developed from its origins in general medicine, the philosophy of minimum intervention in dentistry is based on maintaining long-life oral health, focused on patient-focused oral and dental care to prevent and manage oral diseases. This concept developed from the changes of understanding of disease processesover time. The knowledge of risk/susceptibility factors involved in dental caries development and its diagnosis enable interventions at the earlier stages of the disease in individual patients to reverse/arrest the process. Further details about caries management in primary teeth are accessible for you to learn in our Pediatric dentistry school.
Considered as one of the most prevalent noncommunicable oral diseases by the World Health Organization, dental caries has been the target of treatment to keep teeth functional and aesthetic throughout life. The therapeutic model of ‘‘extension for prevention’’ established originally by GV Black, in which removing all dental tissue affected by the carious lesion would eliminate the disease, is no longer advocated. With adjunctive preventive fluoridated public water supplies and the widespread use of fluoride-containing dentifrices, the concept of minimally invasive selective carious dentine removal concentrating on the infected, contaminated superficial layer of tissue and the introduction of new operative technologies and techniques using bio-interactive adhesives materials have all contributed to achieving the minimum intervention goals. This follows the principles of “recognition, reduction, regeneration and repair”.
Since minimum intervention concepts became more understood, the term “minimally invasive dentistry” also became more widely used, but little attempt to distinguish between them has been observed in the literature. Indeed, due to their same abbreviation, it is common to see both terms being used synonymously, interchangeably and incorrectly, making the establishment of a clear definition and separation of minimum intervention and minimally invasive dentistry, essential.
Minimum intervention was defined by FDI World Dental Federation as a “preventive philosophy, individualised risk assessments, accurate, early detection of lesions and efforts to remineralise non-cavitated lesions with the prompt provision of preventive care in order to minimize operative intervention”. More recently, in a consensus reported by ORCA (European Organization for Caries Research) and IADR (International Association of Dental Research) Cariology Research Group, 81% of participants agreed that minimum intervention describes a “philosophy that integrates caries lesion control and minimal operative intervention”.
On this basis, minimally invasive operative dentistry is included as one of the clinical domains of the minimum intervention philosophy, and should not be considered a synonym of that. In brief, minimally invasive dentistry (MID) could be defined as “interventions that respect biologically the natural tissue”. The concept of minimum intervention care does not apply only to dental caries management however. It can be applied to all disciplines of restorative care and oral health preservation (Figure 1). Therefore, the dated terminology of minimum intervention dentistry must be re-evaluated and re-aligned as maintenance of oral health is also intimately linked to general health. Thus, the use of the term “minimum intervention oral (health) care” (MIOC) as an all-encompassing descriptor has been introduced. Within the discipline of cariology, MIOC aims to delay or prevent the placement of restorations and when required, any intervention should be as least invasive as possible with the removal of a minimal amount of healthy tissue only where necessary to support the final restoration. One example is atraumatic restorative treatment (ART) that is a minimally invasive clinical approach for the management of cavitated carious lesions without the use of specialist surgical equipment/materials.
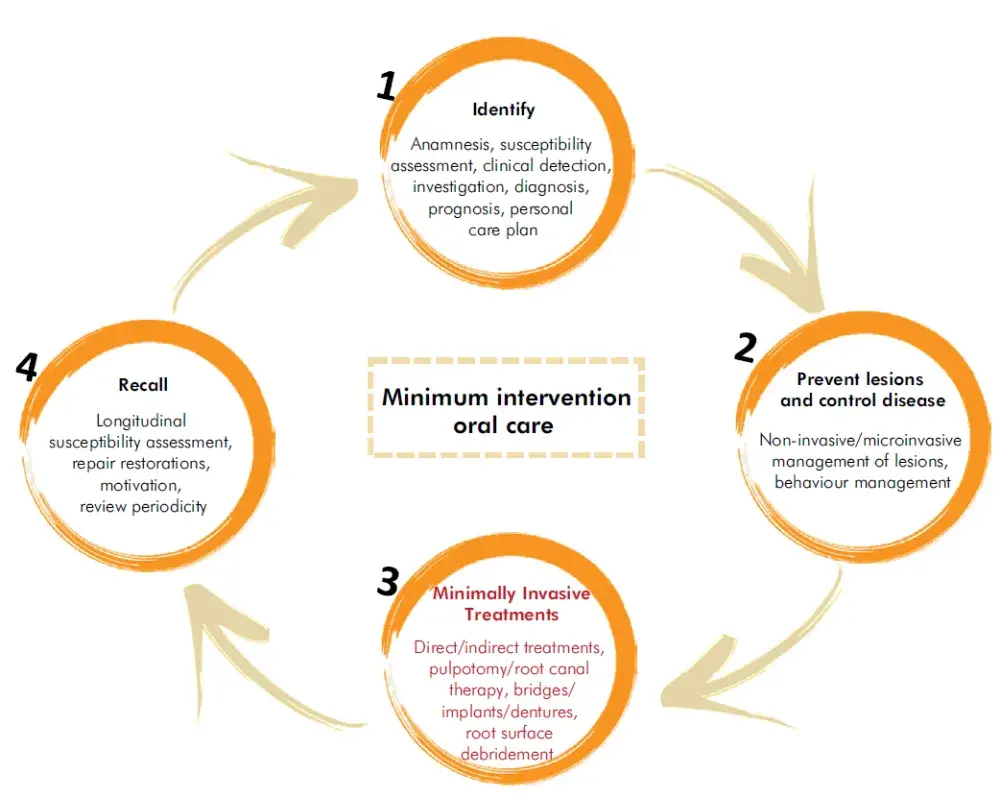 Figure 1. The MIOC framework. Adapted from Banerjee
Figure 1. The MIOC framework. Adapted from Banerjee
Despite the term ‘minimally invasive’ being mostly related to cariology, it can also be used in other operative disciplines in restorative dentistry. For instance, minimally invasive endodontics includes the use of new technologies to reduce hard tissue removal during access cavity and root canal space preparation, irrigants for disinfecting the root canal system and equipment to increase magnification for visualizing the pulp/canal space. This aims to preserve teeth in function, so the use of round burs and Gates-Glidden burs is now discouraged to avoid unnecessary removal and weakening of tooth structure during and after endodontic treatment. In periodontology, minimally invasive periodontal therapies consist of non-surgical techniques used to treat deep pockets with ultrasonic devices with delicate tips and mini-curettes for professional mechanical plaque removal.
The minimum intervention oral care (MIOC) delivery framework is comprised of four interlinked domains as shown in Figure 1. The “identify domain” includes the detection of early lesions and the identification of risk factors, while the “prevent/control domain” encompasses tailored, patientfocused non-invasive strategies, such as diet, biofilm control and the use of fluoride. In this domain, the oral healthcare team assumes the role of educator and health promoter. The “MI restore domain” corresponds to minimally invasive operative interventions for tertiary disease prevention. The fourth last domain of MIOC represents “recall/review/re-assessment” and aims to maintain the patient’s oral health by establishing following-up visits according to his/her specific needs.
The aim of this review is to clarify the role of minimally invasive operative dentistry (MID) within the context of the minimum intervention oral care (MIOC) delivery framework. Important aspects that are leading the profession to shift from an almost exclusively surgical management approach to a prevention-based one with less invasive, tissuepreserving procedures to manage dental caries are discussed. To illustrates implementation, a clinical case is described to exemplify a personalised care plan based on the MIOC framework.
Conventional operative intervention
Traditionally, once a carious lesion was detected clinically, a single operative intervention was the primary treatment choice in order to decontaminate and eliminate “odontopathogens” residing within the lesion. The excision of the entire carious tissue was desirable, extending the cavity margins to sound tissues, before placing a durable dental restorative material. Otherwise, it was thought that lesion progression would be inevitable. As such, these invasive restorative treatments were considered sufficient to arrest/cure the caries process that was thought to be driven histopathologically from within the lesion itself.
However, over time, the profession has seen a transformation in caries management, prompted by a change in the understanding of its etiology and pathogenesis. The decision-making process for caries management is no longer influenced by the assumption that caries is an infectious disease. Those “former odontopathogens” are now recognized as part of the commensal microbiota, comprising a core microbiome that enriches within a dysbiotic situation within the biofilm to ultimately cause tissue damage,a carious lesion. The increased consumption of dietary carbohydrates impacts the oral microbiota composition, richness and diversity. The carbohydrate metabolism of bacteria within the plaque biofilm changes the pH to a more acid environment. Therefore, there is an increased growth of certain aciduric/acidophilic multi-kingdom species, while others may become depleted. This dynamic state can cause imbalances in the demineralizationremineralization process, leading to the development of carious lesions. Building on this, it is now clear that traditional surgical treatments for carious lesions cannot be considered as a cure for the disease process. The minimum intervention oral care (MIOC) philosophy is based upon these updates in understanding.
The minimum intervention oral care (MIOC) framework
The MIOC delivery framework (Figure 1) includes early carious lesion detection as part of the “identify” clinical domain, not based merely on the presence of lesions in an advanced cavitated stage. It is accepted that a carious lesion can be arrested if the overlying biofilm can be disrupted regularly by the patient, at any stage of development, to prevent dysbiosis. Active lesions, cavitated or not, can be managed regardless of the presence of bacteria within the lesion itself, by the re-establishment of homeostasis in the biofilm on the tooth/lesion surface. Isolated restorative operative interventions can help control the caries process occurring in the overlying biofilm assuming the tooth-restoration complex surface is easily cleansable for the patient. Therefore, non-operative prevention and control regimes (the second MIOC domain - cariogenic diet control, biofilm control and rational use of fluoride/remineralisation agents) must go hand-in-hand with operative minimally invasive interventions.
Considering the clinical domain of minimally invasive operative interventions as part of the MIOC framework, direct or indirect restorations, as well as endodontics, should be planned based not only on the size of the cavity preparation, but also on a) the new concepts of caries etiology and pathogenesis; b) the preservation/aesthetics of tooth structure; c) the maintenance of the dental pulp vitality/sensibility d) the strength of the remaining tooth structure; and e) the functional longevity of the tooth-restoration complex (TRC).
Minimally invasive operative treatments, when required, usually alongside/after non-invasive and micro-invasive preventive intervention has been started, represent more advanced therapeutic tertiary prevention, intending to repair areas where tissue damage has caused loss of function, compromised aesthetics and particularly, compromised cleansability of the tooth surface by the patient. Minimally invasive methods should be used in conjunction with efforts to elicit patient behavioural changes affecting the cariogenic habits of the patient. The management of the aetiology of lesion formation/caries process by using non-invasive prevention and control regimes (cariogenic diet control, biofilm control and rational use of fluoride/remineralisation agents) is incorporated in the second clinical domain of MIOC.
The minimally invasive management of caries has also been termed ‘ultraconservative dentistry’ or ‘micro-dentistry’ in the literature. These inconsistencies in terminology and invasive thresholds were explored in the International Caries Consensus Collaboration (ICCC). A standardized terminology was proposed by the consensus delegates, aiming to avoid miscommunication within the research, teaching and clinical practice arenas. Experts also grounded evidence for clinical recommendations of carious tissue removal and cavitated carious lesion management based on the texture of demineralized dentine and lesion depth. The literature available offers robust findings for safely maintaining a mainly demineralised dentine layer (also termed caries-affected dentine) and even some necrotic and disorganized dentine (also termed caries-infected dentine) beneath deep sealed restorations close to the vital pulp. It is better to retain a residual microbiota beneath a deep restoration, that would be depleted due to nutrient starvation stresses, than to risk loss of pulp vitality by direct exposure and further bacterial contamination, during an indiscriminate, non-selective excavation process. The appropriate removal of soft, necrotic tissues is part of an effort to increase the longevity of the tooth-restoration complex, together with controlling the caries process at the patient level to reduce the risk of carious lesion development adjacent to restorations and elsewhere in the mouth. In the past five years or so, there have been several international expert consensus guideline documents published to assimilate this information to enable best practice for clinicians and patient groups.
Contemporary restorations
Dental biomaterials evolution has also reflected the development of MIOC. Adhesive materials, including bonding systems, resin composites and glass polyalkenoate cements (glass-ionomer cements – GICs) are replacing amalgam as the restorative materials of choice, allowing the preparation of smaller cavities. These materials evolve with always improving physico-chemical and biological properties. Likewise, modern resin composites are blurring the boundaries between the choice of direct or indirect restorative treatments in many clinical situations, due to their continuous enhancement of mechanical and biological properties, aesthetic and anatomic mimicry, monomer-polymer conversion, physical properties closer to dentine and improved bond strengths.
When questioning the need for invasive procedures, it is necessary to bear in mind the importance of delaying the first restoration as much as possible, as described above. No restorative procedure is definitive, and thus, whenever a tooth is restored, a repetitive restorative cycle begins, since further re-interventions are inevitable. Restorative re-treatments of the tooth-restoration complex (TRC) involve additional preparation of dental tissues and, as a result, cavity preparations become progressively larger. Successive re-treatments negatively affect the rate of TRC survival by making the TRC weaker, the so-called “tooth death spiral”. This understanding of the finite life of all restorative procedures is essential to guide current MI restorative procedures. In addition, there is no single objective criterium that defines an unsatisfactory restoration and, therefore, the decision to repair, replace or perform maintenance (sealing, refurbishing) is still challenging in clinical practice. The decision to replace a restoration, often based on subjective criteria and unnecessarily, still seems to be the first option of dentists. In view of the need for reintervention, repairs, re-sealing, refurbishing or simple review (the “5Rs”) should be preferable to the complete replacement of the restoration, avoiding cavity enlargement and, consequently, decelerating the loss of natural tissue.
Personalised care planning based on MIOC
MIOC is based, as previously mentioned, on the four interlinked, patient-focused, oral healthcare team-delivered clinical domains: identify – including anamnesis, caries detection and risk/susceptibility assessment, investigations, personalised care planning; prevention of lesions/control of disease –non-operative behavioral preventive measures, remineralisation, biofilm/diet control, sealants/infiltration; minimally invasive operative procedures – including selective caries removal, “5Rs” management of TRCs; and tailored recall consultations (Figure 1). The professional oral healthcare team members must incorporate the MIOC delivery framework from the moment that the patient contacts the practice, either physically or online.
It is unquestionable that dental caries is, to a large extent, modulated by the individual patient’s lifestyle (diet, oral hygiene habits, etc.), which in turn is influenced by socioeconomic factors including education level, occupation and income. Additionally, general health issues and the use of certain medications may also play an important role in caries development. Therefore, within the MIOC framework, these aspects should be assessed as part of the “identify” clinical domain. They will not only facilitate the professional team to understand the patient’s current oral health situation, but will assist the team in identifying caries risk/susceptibility factors that should be addressed as part of his/her individualized oral health promotion program. Although the absolute validity of caries risk/susceptibility assessment tools is limited, their importance as pedagogical value for patients’ oral health education is incontestable. The second step in the identify domain, refers to the implementation of a well-conducted clinical oral examination of clean and and dry tooth surfaces, using a validated caries detection system.
With the information gathered in the identify phase, the professional(s) is now able to establish a personalised plan care plan that includes the prevention and/or control of initial carious lesions in which different non- and micro- invasive primary and secondary preventive strategies are available. For more complex cases, minimally invasive tertiary preventive procedures can be selected. Patient behavior change using the capability, opportunity and motivation behavior model (COM-B) needs to be implemented by the team members to help facilitate and engage with the patient in order to modify their behaviors that increase their personal caries risk/susceptibility.
Last but not least, it is important to establish a suitable recall/review/re-assessment program according to the patient’s profile and behavior. For example, a young child who has been referred for dental treatment due to early childhood caries, presenting with many active cavitated and noncavitated lesions, should not have the same follow-up regimen as a child of similar age who is caries-free. In other words, different people require different tailored approaches. To exemplify a personalised care plan based on the MIOC framework domains, a case of a 15 yr-old adolescent who sought treatment for dental caries is presented.
Identifying the problem
Initially, it is crucial to understand that proper caries diagnosis extends well beyond merely counting lesions/cavities. For that reason, an extensive and careful anamnesis is conducted, in which information about the patient’s socio-demographic profile, diet and oral hygiene habits is collected. Medical and dental histories are also recorded.
The next step in the MIOC identification domain is to perform the clinical oral examination. The presence of visible plaque and gingival bleeding should be registered, as they might assist the oral healthcare team professional in assessing the patients’ caries risk/susceptibility. Moreover, the literature points to an association between active carious lesions and visible dental plaque.
Immediately after, considering that caries detection should be carried out on clean and dry tooth surfaces, a professional prophylaxis is performed. In the clinical case presented, dental caries is recorded using the CAST (Caries Assessment Spectrum and Treatment) instrument, but other caries detection systems including the International Caries Detection Assessment System and the Nyvad criteria do exist. In this regard, it is worth mentioning that there is evidence showing that the use of validated and wellestablished visual scoring systems improves the accuracy of visual caries detection. Additionally, the implementation of a systematic method of registering dental caries allows more precise monitoring of the patient’s condition over time. It is also important to use a caries detection system that includes initial carious lesions. According to the MIOC framework, interrupting the repeat restoration cycle by postponing or even avoiding the first invasive procedure, is essential for keeping teeth functional for life. Therefore, the assessment of incipient carious lesions and consequently, an early secondary preventive intervention in such reversible lesions, non- or micro-invasively, both play a significant role in achieving the MIOC goals.
The dental examination of this patient identifies some inactive enamel carious lesions and a cavitated dentine lesion on tooth 16 (Figure 2a). The long cone peri-apical radiograph shows a deep carious lesion into the inner third of dentine, but without periapical alterations (Figure 2b).
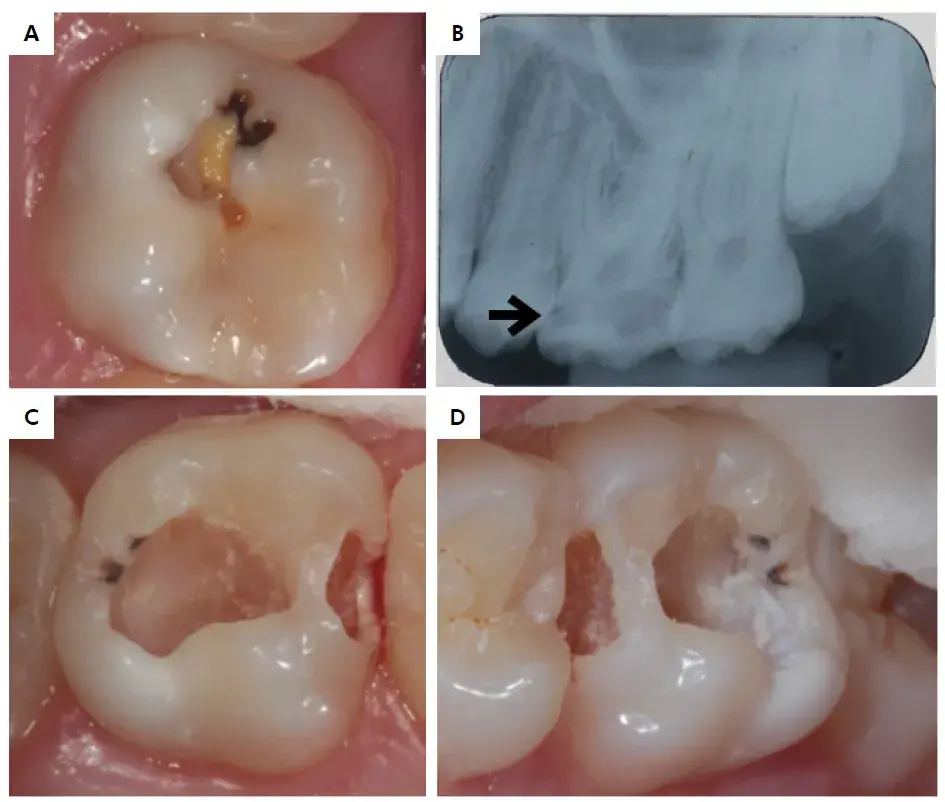 Figure 2. The clinical (a) and radiographic (b) representation of tooth 16. Observe that the radiograph shows a carious lesion at the mesial surface (arrow) of the tooth which was not detected clinically (c) and of the occluso-mesial (d) cavities immediately after carious tissue.
Figure 2. The clinical (a) and radiographic (b) representation of tooth 16. Observe that the radiograph shows a carious lesion at the mesial surface (arrow) of the tooth which was not detected clinically (c) and of the occluso-mesial (d) cavities immediately after carious tissue.
Prevention of lesions/control of disease
Taking into account the anamnesis - the patientpresents with good general health, living in an area with fluoridated water (0.07ppm) - and the clinical findings - excluding the carious lesion observed on the 16, no other lesion is either cavitated or active, the patient is considered at medium caries risk/susceptibility. In such cases, prevention/control measures such as positive behavior reinforcement regarding oral hygiene and diet control should always be incorporated in the personalised oral healthcare plan. This will enable and facilitate the patient to achieve behavior change goals that are set between them and the oral healthcare team.
Minimally invasive operative procedures
With respect to the cavitated tooth 16, since it does not present with a history of spontaneous pain, fistula or abscess, the decision for a minimally invasive approach is made, to improve tooth surface cleansability for the patient as well as restoring aesthetics and long term function. Carious tissue is removed selectively, up to leathery caries-affected dentine at the pulp aspect in order to avoid pulpal exposure ( Figure 2 c). M oreover, f ollowing t he minimally invasive principles, two separate cavities were created, preserving as much sound enamel structure as possible (Figure 2d). A high viscosity glass-ionomer restoration was placed and the patient’s recall visit was scheduled in within 90 days (tailored recall). The patient was instructed to contact the team in case of pain, discomfort or abscess.
Recall consultation
During the recall consultation, scheduled 3 months later, the patient reports neither dental pain nor clinical (Figure 3a) symptoms being present. Considering the depth of the lesion, a follow-up radiograph is taken showing no further signs of pulp necrosis (Figure 3b). Although a radiolucency adjacent to the base of the restoration was noticed on the radiograph, this should not be considered a concern, since the literature indicates that the caries-affected dentine in this area is demineralised but tends to remineralise slowly over time, as well as there being a reduction in the number of microorganisms is this retained tissue. Taking all these factors into consideration, a re-intervention (stepwise excavation) is judged unnecessary, as this step increases the risk of pulp exposure, besides adding additional cost, time and discomfort for the patient.
In conclusion, the decision to follow еhe MIOC framework to manage this case not only allows a more patient-friendly approach, but also the preservation of sound tooth structure with improved long term outcomes.
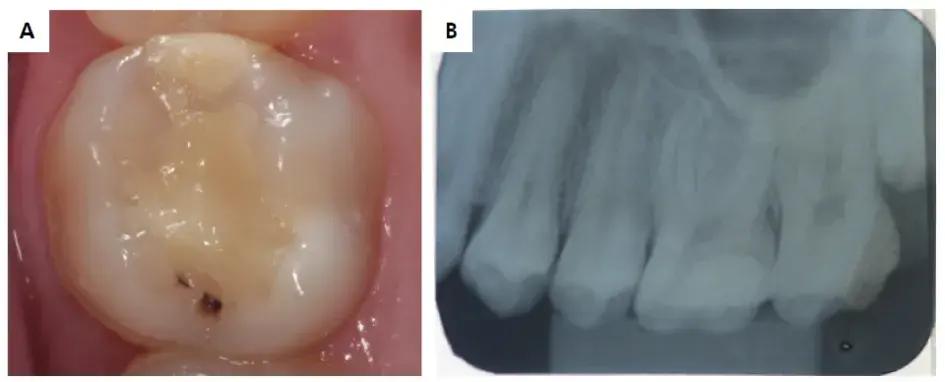 Figure 3. Clinical (a) and radiograph (b) aspect of the restoration 90 days after being placed.
Figure 3. Clinical (a) and radiograph (b) aspect of the restoration 90 days after being placed.
Conclusions
Having clarified the important differences and links between minimum intervention oral care (MIOC) and minimally invasive dentistry (MID), the challenge now is to translate the concepts presented above for clinical practitioners to implement in primary care. For instance, the recommendation of selective caries removal, retaining caries-affected dentine below the restorative material, or performing ART, are still considered “temporary treatments” by some outdated professionals. Depending on the region or country, professionals are more or less prone to perform minimally invasive procedures. Although this paper addressed the application of the MIOC framework to manage dental caries, it is important to highlight that the concept can and should be applied in all restorative disciplines. For that reason, all members of the oral healthcare team need to be trained to appreciate and practice MIOC delivery.
The challenge to incorporate the MIOC framework into daily practice involves changes in attitude by the multiple stakeholders affecting oral healthcare delivery. These include all oral healthcare clinical professionals, academics, researchers, industry partners, policy makers, regulators, indemnity providers and even the media. For that to happen, evidence-based best practice guidelines are needed and are being developed considering both the public and private sectors, taking also into consideration the particularities of the oral health systems of individual countries. The diffusion of the MIOC concept should be based on low-bias evidence and be effectively incorporated into the daily practice. One of the most important steps in that direction was the inclusion of the MIOC approach in a modern cariology curriculum to prepare future dentists to implement the current evidence. Finally, it is important to highlight that about 532 million children and 2.3 billion adults are living with untreated cavitated carious lesions worldwide and prevention-based MIOC/MID might be the most useful and cost-effective strategy to control the disease benefiting, especially, those vulnerable, high-need populations who often lack access to adequate oral healthcare.
If you enjoyed reading this article and would like to explore primary teeth treatment protocols further, we encourage you to enroll our website.
List of authors
Soraya Coelho LEAL
Naile DAME-TEIXEIRA
Cecília de Brito BARBOSA
Paula Akemi Albuquerque KOMINAMI
Fernanda RAPOSO
Eliana Mitsue Takeshita NAKAGAWA
Avijit BANERJEE
References
1. Banerjee, A. ‘Minimum intervention’: MI inspiring future oral healthcare? Br Dent J. 2017 Aug;233:133-5.
2. Banerjee A. Minimum intervention oral healthcare delivery: is there consensus? Br Dent J. 2020 Oct;229(7):393-5.
3. Banerjee A. Minimal intervention dentistry: Part 7. Minimally invasive operative caries management: rationale and techniques. Br Dent J. 2013 Feb;214(3):107-11.
4. Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ. Minimal intervention dentistry: a review. FDI Commission Project 1-97. Int Dent J. 2000 Feb;50(1):1-12.
5. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Disease and global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018 Nov;392(10159):1789-858. 32279-7
6. Frencken JE, Leal SC, Navarro MF. Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig. 2012 Oct;16(5):1337-46.
7. Banerjee A, Frencken JE, Schwendicke F, Innes NP. Contemporary operative caries management: consensus recommendations on minimally invasive caries removal. Br Dent J. 2017 Aug;223(3):215-22.
8. Leal SC. Minimal intervention dentistry in the management of the paediatric patient. Br Dent J. 2014 Jun;216(11):623-7.
9. Frencken JE, Peters MC, Manton DJ, Leal SC, Gordan VV, Eden E. Minimal intervention dentistry for managing dental caries: a review: report of a FDI task group. Int Dent J. 2012 Oct;62(5):223-43.
10. Walsh LJ, Brostek AM. Minimum intervention dentistry principles and objectives. Aust Dent J. 2013 Jun;58 Suppl 1:3-16.
11. Longbottom CL, Huysmans MC, Pitts NB, Fontana M. Glossary of key terms. Monogr Oral Sci. 2009;21:209-16.
12. Machiulskiene V, Campus G, Carvalho JC, Dige I, Ekstrand KR, Jablonski-Momeni A, et al. Terminology of dental caries and dental caries management: consensus report of a workshop organized by ORCA and Cariology Research Group of IADR. Caries Res. 2020;54(1):7-14.
13. Banerjee A. W. T. Pickard’s Guide to minimally invasive operative dentistry. 10th ed. Oxford: Oxford University Press; 2015.
14. Peters MC, McLean ME. Minimally invasive operative care. I. Minimal intervention and concepts for minimally invasive cavity preparations. J Adhes Dent. 2001;3(1):7-16.
15. Dalli M, Çolak H, Mustafa Hamidi M. Minimal intervention concept: a new paradigm for operative dentistry. J Investig Clin Dent. 2012 Aug;3(3):167-75.
16. Gluskin AH, Peters CI, Peters OA. Minimally invasive endodontics: challenging prevailing paradigms. Br Dent J. 2014 Mar;216(6):347-53.
17. Rethman MP, Harrel SK. Minimally invasive periodontal therapy: will periodontal therapy remain a technologic laggard? J Periodontol. 2010 Oct;81(10):1390-5.
18. Ribeiro FV, Casarin RC, Palma MA, Júnior FH, Sallum EA, Casati MZ. Clinical and microbiological changes after minimally invasive therapeutic approaches in intrabony defects: a 12-month follow-up. Clin Oral Investig. 2013 Sep;17(7):1635-44.
19. Marsh PD. Microbial ecology of dental plaque and its significance in health and disease. Adv Dent Res. 1994 Jul;8(2):263-71.
20. Aas JA, Griffen AL, Dardis SR, Lee AM, Olsen I, Dewhirst FE, et al. Bacteria of dental caries in primary and permanent teeth in children and young adults. J Clin Microbiol. 2008 Apr;46(4):1407-17.
21. Parolo CC, Maltz M. Microbial contamination of noncavitated caries lesions: a scanning electron microscopic study. Caries Res. 2006;40(6):536-41.
22. Mackenzie L, Banerjee A. Minimally invasive direct restorations: a practical guide. Br Dent J. 2017 Aug;223(3):163-71.
23. Schwendicke F, Splieth C, Breschi L, Banerjee A, Fontana M, Paris S, et al. When to intervene in the caries process? An expert Delphi consensus statement. Clin Oral Investig. 2019 Oct;23(10):3691-703.
24. Frencken JE, Innes NP, Schwendicke F. Managing Carious lesions: why do we need consensus on terminology and clinical recommendations on carious tissue removal? Adv Dent Res. 2016 May;28(2):46-8.
25. Innes NP, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res. 2016 May;28(2):49-57.
26. Schwendicke F, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res. 2016 May;28(2):58-67.
27. Franzon R, Casagrande L, Pinto AS, García-Godoy F, Maltz M, Araujo FB. Clinical and radiographic evaluation of indirect pulp treatment in primary molars: 36 months follow-up. Am J Dent. 2007 Jun;20(3):189-92.
28. Alves LS, Fontanella V, Damo AC, Oliveira EF, Maltz M. Qualitative and quantitative radiographic assessment of sealed carious dentin: a 10-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010 Jan;109(1):135-41.
29. Maltz M, Alves LS, Jardim JJ, Moura MS, Oliveira EF. Incomplete caries removal in deep lesions: a 10-year prospective study. Am J Dent. 2011 Aug;24(4):211-4. PMID:22016914
30. Maltz M, Henz SL, Oliveira EF, Jardim JJ. Conventional caries removal and sealed caries in permanent teeth: a microbiological evaluation. J Dent. 2012 Sep;40(9):776-82.
31. Bitello-Firmino L, Soares VK, Damé-Teixeira N, Parolo CC, Maltz M. Microbial load after selective and complete caries removal in permanent molars: a randomized clinical trial. Braz Dent J. 2018 May-Jun;29(3):290-5.
32. Splieth CH, Banerjee A, Bottenberg P, Breschi L, Campus G, Ekstrand KR, et al. How to Intervene in the caries process in children: a joint ORCA and EFCD Expert Delphi Consensus statement. Caries Res. 2020;54(4):297-305.
33. Paris S, Banerjee A, Bottenberg P, Breschi L, Campus G, Doméjean S, et al. How to intervene in the caries process in older adults: a joint ORCA and EFCD Expert Delphi Consensus statement. Caries Res. 2020 Dec;54(5-6):1-7.
34. Schwendicke F, Lamont T, Innes N. Removing or controlling? how caries management impacts on the lifetime of teeth. Monogr Oral Sci. 2018;27:32-41.
35. Martins BM, Silva EJ, Ferreira DM, Reis KR, Fidalgo TK. Longevity of defective direct restorations treated by minimally invasive techniques or complete replacement in permanent teeth: a systematic review. J Dent. 2018 Nov;78:22-30.
36. Green D, Mackenzie L, Banerjee A. Minimally Invasive long-term management of direct restorations: the ‘5 Rs’. Dent Update. 2015 Jun;42(5):413-6.
37. Young S, Dawett B, Gallie A, Banerjee AD. Minimum intervention oral care delivery for children: developing the oral healthcare team. Dent Updat. 2021;49(5).
38. Leal SC, Takeshita EM, Guaré RO, Diniz DD. Caries diagnosis: a comprehensive exercise. In: Leal SC, Takeshita EM, eds. Pediatric restorative dentistry. Cham: Springer; 2019. p. 1-12.
39. Newton JT, Asimakopoulou K. Minimally invasive dentistry: enhancing oral healthrelated behaviour through behaviour change techniques. Br Dent J. 2017 Aug;223(3):147-50.
40. Ferreira MA, Souza DL, Almeida GC, Aguiar HS. Active white enamel lesion: a case-control study. Oral Health Prev Dent. 2007;5(3):209-14.
41. Pretty IA, Ekstrand KR. Detection and monitoring of early caries lesions: a review. Eur Arch Paediatr Dent. 2016 Feb;17(1):13-25.
42. Frencken JE, Souza AL, Sanden WJ, Bronkhorst EM, Leal SC. The Caries Assessment and Treatment (CAST) instrument. Community Dent Oral Epidemiol. 2013 Feb;41(1):e71-7.
43. Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007 Jun;35(3):170-8.
44. Nyvad B, Machiulskiene V, Baelum V. Reliability of a new caries diagnostic system differentiating between active and inactive caries lesions. Caries Res. 1999 Jul-Aug;33(4):252-60.
45. Gimenez T, Piovesan C, Braga MM, Raggio DP, Deery C, Ricketts DN, et al. Visual inspection for caries detection: a systematic review and meta-analysis. J Dent Res. 2015 Jul;94(7):895-904.
46. Laske M, Opdam NJ, Bronkhorst EM, Braspenning JC, Sanden WJ, Huysmans MC, et al. Minimally invasive intervention for primary caries lesions: are dentists implementing this concept? Caries Res. 2019;53(2):204-16.
47. Mickenautsch S. Adopting minimum intervention in dentistry: diffusion, bias and the role of scientific evidence. J Minim Interv Dent. 2009;11:16-26.
48. Innes NP, Chu CH, Fontana M, Lo EC, Thomson WM, Uribe S, et al. A Century of change towards prevention and minimal intervention in cariology. J Dent Res. 2019 Jun;98(6):611-7.
49. Pitts N. Preventive and minimal intervention dentistry in the undergraduate curriculum. J Dent. 2011 Dec;39 Suppl 2:S41-8.
50. Bernabé E, Marcenes W. Can minimal intervention dentistry help in tackling the global burden of untreated dental caries? Br Dent J. 2020 Oct;229(7):487-91.
