Minimally Invasive Treatment of White Spot Lesions – A Systematic Review
Purpose: To evaluate the efficacy of minimally invasive methods for the treatment of white-spot lesions involving fluorides, CPP-ACP (casein phosphopeptide-stabilised amorphous calcium phosphate) and resin infiltration vs a placebo or control.
Materials and Methods: According to predetermined criteria, four databases were searched for eligible studies. References of the selected articles and relevant reviews were searched for any missed publications.
Results: Eight randomised controlled trials were selected as eligible studies, and only qualitative analyses were performed because of the diversity of the interventions and outcome measures. Three studies showed significant effects of three different fluoride preparations and used DIAGNOdent and ICDAS to assess the white spot lesions. Both studies comparing resin infiltration to a placebo showed significant effects in treating white spot lesions. One study using CPP-ACP showed a significant improvement in the lesions post treatment.
Conclusion: Evidence suggests minimally invasive treatment modalities of white spot lesions produced significant improvement in the appearance and regression of white spot lesions following treatment when compared to a control or placebo.
Key words: CPP-ACP, dental caries, fluorides, resin infiltration, white spot lesions.
White spot lesions (WSL) have been defined as a 'subsurface enamel porosity from carious demineralisation' that present themselves as 'a milky white opacity when located on smooth surfaces'. The WSL is the first visible evidence of caries in enamel, characterised by a demineralised lesion underneath an intact surface. WSL develop as a result of a dietary carbohydrate- and salivamodified bacterial infection, resulting in an imbalance between demineralisation and remineralisation of the enamel. The lesion is caused by the accumulation of plaque and bacteria, along with insufficient oral hygiene. High oral plaque accumulation can increase the risk of WSL formulation. In 1966, Dirks was the first to describe the (possible) remineralisation of natural enamel lesions formed in vivo, so-called white spot lesions, as a normal occurrence in the oral environment. In the natural state, natural demineralisation and remineralisation continually takes place. Saliva can remineralise WSL to some degree, but this process is slow and rarely results in complete resolution of the lesions. When left untreated, the acids keep diffusing into the porous subsurface enamel, dissociating and producing hydrogen ions. The hydrogen ions in turn trigger the release of calcium and phosphate into solution, which then diffuse out of the tooth. If left to advance, this eventually leads to loss of the surface integrity of the enamel, which becomes cavitated. You have the opportunity to gather more in-depth information about discolorites treatment on our website.
Overall management of WSL involves methods of preventing demineralisation as well as methods of encouraging remineralisation of existing lesions. The conventional treatment approach is based on restoration, which, in most instances, is quite invasive. The aim of modern dentistry is focused on a prophylactic approach instead of invasive restoration of carious defects. The occurrence and spread of WSL can be minimised by preventive treatment with fluoride toothpaste and rinses, topical fluoride applications and oral hygiene instructions.
Since most patients requiring treatment for white spot lesions are adolescents or young adults, minimally invasive treatment options are needed to prevent excessive sacrifice of dental tissue at an early age. To minimally invasively treat WSL, remineralisation products (fluorides, casein phosphopeptide-stabilised amorphous calcium phosphate [CPP-ACP]) or resin-based products, such as infiltrants, are used.
On white spot lesions, fluoride inhibits demineralisation while also acting cariostatically through enhancement of remineralisation processes, the latter being the stronger effect. CPP-ACP is a relatively new means of remineralising tooth surfaces by keeping high levels of calcium and phosphorus ions in the proximity of the enamel. Casein phosphopeptides bind the calcium and phosphate ions, forming CPP-ACP complexes, which release calcium and phosphorus ions at pH values below 7. The anticariogenicity mechanism is thought to consist in the ACP acting as a buffer on the actions of free calcium and phosphate, thereby promoting remineralisation. Casein itself has also been shown to have an anticariogenic capacity through its ability to incorporate into plaque, thus preventing subsurface demineralisation of the enamel. CPP-ACP can be used both in professionally applied products and in those meant for home use.
Recently, the resin infiltration technique was introduced as a type of minimally invasive treatment. The resin infiltration technique prevents further progression of the lesion using a low-viscosity resin with a high penetration coefficient, filling the enamel intercrystalline spaces. This technique has been reported to remove the whitish opaque colour, thereby changing the colour and translucency of the white lesion. Evidence is abundant regarding the prevention of WSL with these treatment modalities. Literature on the effectiveness of remineralisation and resin products in treating WSL is limited. Therefore, the aim of the present systematic review was to evaluate the efficacy of minimally invasive treatment modalities in treating white spot lesions.
MATERIALS AND METHODS
Structured question: Do minimally invasive treatment modalities such as fluoride, CPP-ACP and resin infiltration treat white spot lesions effectively?
Search strategy
The Medline/PubMed, LILACS, SciELO and Science Direct databases were searched to identify relevant studies published up to June 2014. To locate additional studies, the references of the selected articles and relevant reviews were also checked. The search strategies included a combination of controlled vocabulary and free text terms. We employed the following keywords related to the intervention method, type of lesion and outcome.
• Intervention: fluorides, CPP-ACP or resin infiltration
• Type of lesion: white spot lesions
• Outcome: progression or regression.
Inclusion and exclusion criteria
The selection was limited to published randomised clinical trials in English evaluating minimally invasive approaches to treating WSL, e.g. with fluorides, resin infiltration and CPP-ACP, after orthodontic treatment. Only studies comparing fluorides, CPP-ACP and resin infiltration with a control or placebo after orthodontic treatment were included. Studies were excluded if they: included invasive approaches to treating WSL, involved animal models, were published in languages other than English, were review articles or in vitro studies. Studies evaluating the preventive effect of minimally invasive treatment modalities for white spot lesions during orthodontic treatment and comparing among fluorides, CPP-ACP and resin infiltration were also excluded.
Screening methods and data extraction
According to the predetermined inclusion and exclusion criteria, all titles and abstracts were examined by an independent reviewer (ZA) to find relevant studies; the full texts of the relevant studies were scrutinised by another reviewer (JJ) independently to select eligible studies. Any disagreement was discussed, and a final consensus was reached. In the analysis of these included studies, the following questions were addressed: (1) Does topical fluoride application effectively arrest the progression of or treat the WSL? (2) Does CPP-ACP effectively arrest the progression of or treat the WSL? (3) Does resin infiltration using ICON (DMG; Hamburg, Germany) effectively arrest the progression of or treat the white spot lesions?
For each included study, descriptive and quantitative information was extracted, including citation author, year of publication, experimental treatment (number of subjects), control treatment (number of subjects}, treatment duration, assessment method, results of baseline and follow-up visits, authors' conclusions, and all information needed to fulfill quality evaluation criteria. Each study's methodological quality was assessed by using the domainbased evaluation described in the Cochrane Handbook for Systematic Reviews of Interventions 5.0.2.12. Using the guidelines in the Cochrane Handbook, one reviewer (ZA) independently assessed the quality of the identified studies. The reviewers categorised the following 6 quality items as 'yes' (low risk of bias), 'unclear' (uncertain risk Vol 14, No 3, 2016 of bias), or 'no' (high risk of bias): sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias. The level of risk for each study was then classified as low (all quality items were met), medium (1 or 2 quality items were not met), or high (3 or more quality items were not met).
Statistical analysis
Due to the heterogeneous nature of the various assessment techniques and interventions included in this review, the pooling of data was not possible.
RESULTS
The electronic and hand searches retrieved 488 unique citations, which were entered into a flow chart (Fig 1) to illustrate the path for selecting the final trials. After evaluating titles and abstracts, we obtained 19 relevant studies (one study39 could not be located). After evaluating the full texts, we selected eight studies as eligible. Eleven articles were excluded from the study. After searching the references of the selected articles and relevant reviews, we identified no additional eligible studies. Finally, eight studies, all in English, were used for the systematic review, and a description of each is given in Table 1.
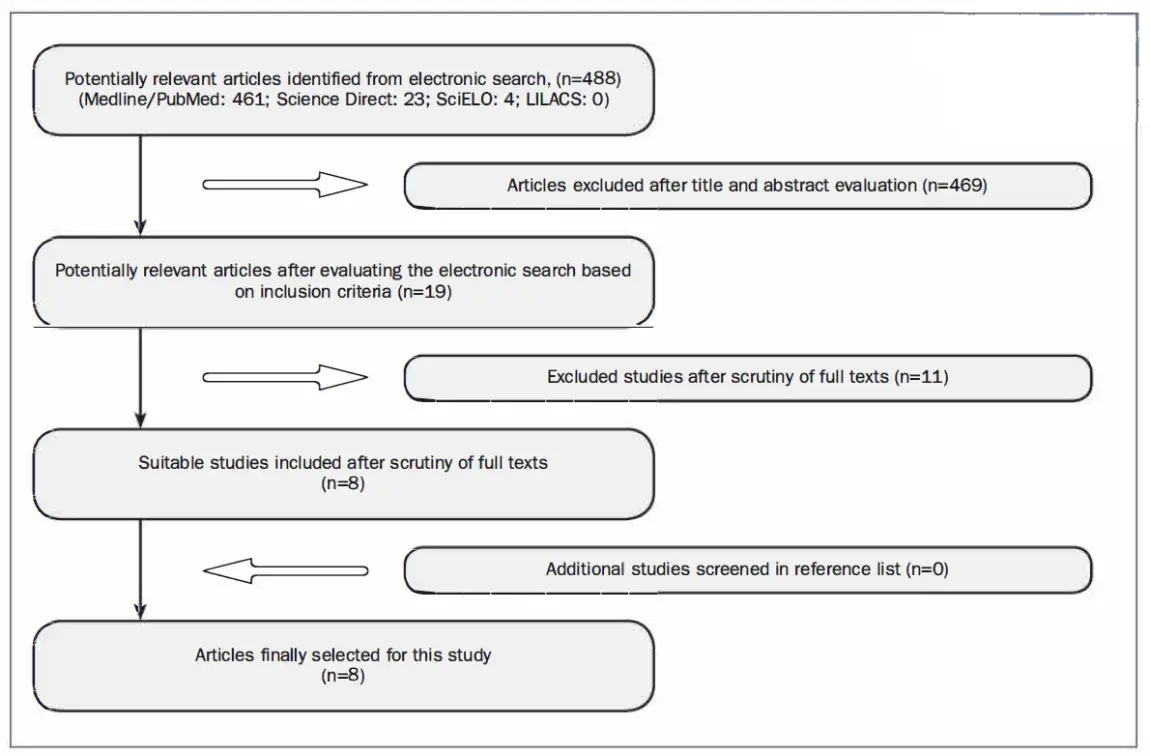 Fig 1. Flowchart of the included studies.
Fig 1. Flowchart of the included studies.
Table 1. Summary of studies included
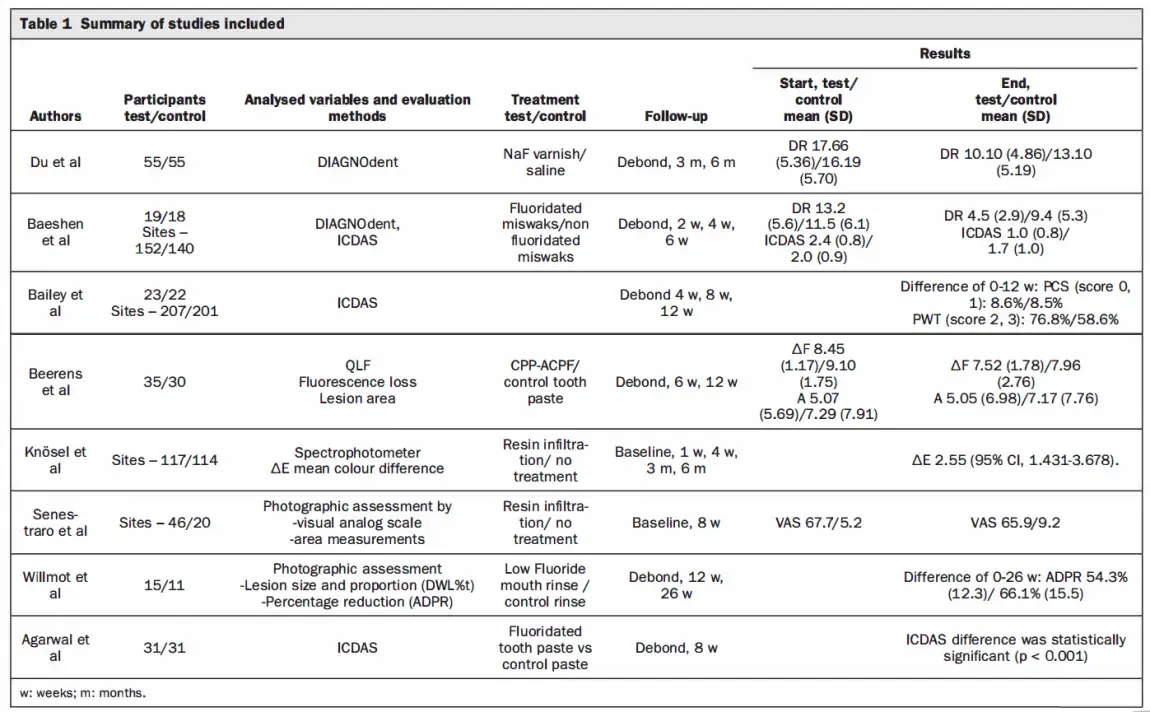 Among the eight included studies, four randomised controlled trials evaluated the effects of fluoride in different vehicles: 50-ppm sodium fluoride mouth rinse, 5% sodium fluoride varnish, 0.5% sodium fluoride chewing sticks3 and a sodium fluoride toothpaste (EP 0.32% w/w, 1450 ppm fluoride). The remaining four studies compared the effects of agents containing CCP-ACP, casein phosphopeptide amorphous calcium fluoride phosphate and resin infiltration. No significant similarities in methodologies could be found in these studies. All the included studies were compared with a placebo, a control group or no intervention.
Among the eight included studies, four randomised controlled trials evaluated the effects of fluoride in different vehicles: 50-ppm sodium fluoride mouth rinse, 5% sodium fluoride varnish, 0.5% sodium fluoride chewing sticks3 and a sodium fluoride toothpaste (EP 0.32% w/w, 1450 ppm fluoride). The remaining four studies compared the effects of agents containing CCP-ACP, casein phosphopeptide amorphous calcium fluoride phosphate and resin infiltration. No significant similarities in methodologies could be found in these studies. All the included studies were compared with a placebo, a control group or no intervention.
Two studies used DIAGNOdent, one of which also used the ICDAS criteria. Two other studies used the ICDAS (International Caries Detection and Assessment System) criteria to determine the effectiveness of CPP-ACP and fluoridated toothpaste. One study used quantitative light-induced fluorescence and one study used a spectrophotometer to evaluate the lesions. Two studies used photographic examination, but were conducted on different products and also did not use the same method to examine the photographs. Due to the given circumstances, it was not feasible to create a pool of data to perform a meta-analysis. Thus, a qualitative analysis was undertaken.
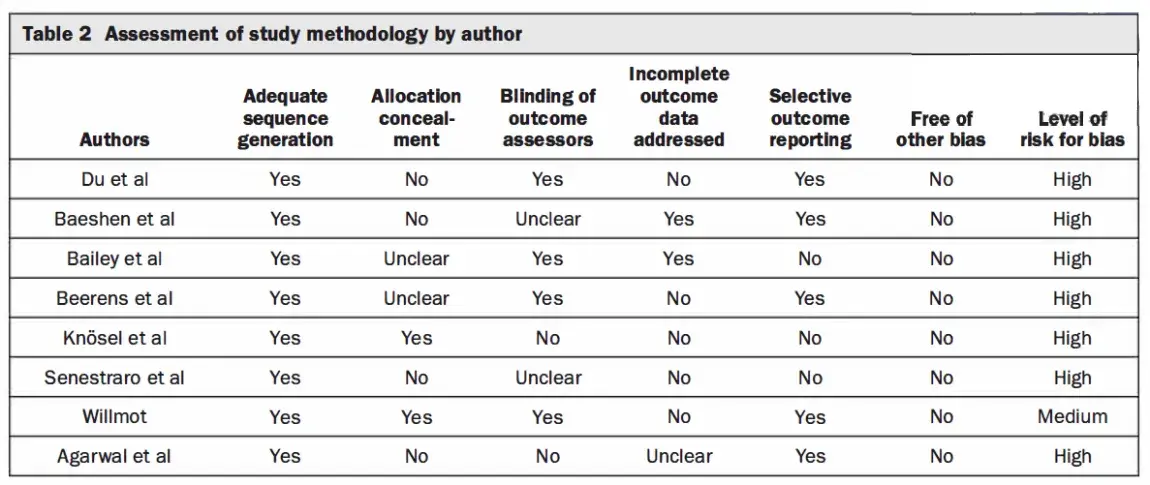
All studies had methodological problems after examination (Table 2). Whether or not the randomisation was blinded was not reported in two studies, and the blinding procedure was unclear in two other studies. Whether the operator and the evaluator were separate persons was unclear in one study. Two studies did not report the data based on patients, and one study did not report a prespecified primary outcome measured by quantitative light-induced fluorescence. Statistical analyses of two studies were based on the number of teeth, and the assessment methods of three studies were only technology based (DIAGNOdent pen, quantitative light-induced fluorescence, or spectrophotometer). One study did not mention the ICDAS scores in the results section, which was a major limitation of the study.
Table 2. Assessment of study methodology by author
 We categorised the study according to the interventions and assessment methods. Four studies tested fluoride in different vehicles and preparations for the treatment of white spot lesions. One study assessed the effect of 50 ppm of fluoride for the treatment of WSL by using computerised image analysis to measure the lesion sizes. In a 26-week follow-up, the value of the average difference in the percent reduction of lesion size did not decrease significantly in the test group compared with the control group (mean difference -0.12, 95% confidence interval [Cl] -0.25-0.01). The second study tested the efficacy of fluoride varnish (5% sodium fluoride) assessed with laser fluorescence (DIAGNOdent), and indicated that the DIAGNOdent readings were significantly different between the fluoride-treated group and the control group (mean difference -4.47, 95% Cl -6.59- -2.35). The third study compared 0.5% sodium fluoride chewing sticks with nonfluoridated chewing sticks by using visual inspection (ICDAS II index criteria) and DIAGN0dent. At the end of treatment, both the DIAGNOdent readings and the ICDAS II index had significantly decreased in the intervention group compared with the control group (mean difference 6.60, 95% Cl 4.68-8.52; mean difference 1.10, 95% Cl 0.7 7-1.43; respectively). The fourth study was conducted to test the effectiveness of fluoridated toothpaste vs a nonfluoridated toothpaste and used the ICDAS II to score the WSL at baseline and 8 weeks. The ICDAS II index of the WSL decreased in the test group in the mandibular dentition but not on the maxillary dentition during the 8-week trial (p < 0.0001).
We categorised the study according to the interventions and assessment methods. Four studies tested fluoride in different vehicles and preparations for the treatment of white spot lesions. One study assessed the effect of 50 ppm of fluoride for the treatment of WSL by using computerised image analysis to measure the lesion sizes. In a 26-week follow-up, the value of the average difference in the percent reduction of lesion size did not decrease significantly in the test group compared with the control group (mean difference -0.12, 95% confidence interval [Cl] -0.25-0.01). The second study tested the efficacy of fluoride varnish (5% sodium fluoride) assessed with laser fluorescence (DIAGNOdent), and indicated that the DIAGNOdent readings were significantly different between the fluoride-treated group and the control group (mean difference -4.47, 95% Cl -6.59- -2.35). The third study compared 0.5% sodium fluoride chewing sticks with nonfluoridated chewing sticks by using visual inspection (ICDAS II index criteria) and DIAGN0dent. At the end of treatment, both the DIAGNOdent readings and the ICDAS II index had significantly decreased in the intervention group compared with the control group (mean difference 6.60, 95% Cl 4.68-8.52; mean difference 1.10, 95% Cl 0.7 7-1.43; respectively). The fourth study was conducted to test the effectiveness of fluoridated toothpaste vs a nonfluoridated toothpaste and used the ICDAS II to score the WSL at baseline and 8 weeks. The ICDAS II index of the WSL decreased in the test group in the mandibular dentition but not on the maxillary dentition during the 8-week trial (p < 0.0001).
Two studies compared CPP-ACP to a control group. One study used the quantitative light-induced fluorescence system (QLF) and measured parameters such as fluorescence loss, integrated fluorescence loss and lesion area. This study showed a significant decrease in fluorescence loss for both groups between baseline and follow-up, but no statistically significant differences between the groups were observed with regard to the sizes of the lesions (mean difference 0.10, 95% Cl -3.72-3.92) or the fluorescence loss (mean difference 0.21, 95% Cl -0.88-1.30). A study assessing the effect of CPP-ACP used ICDAS criteria as an assessment method. In a 12-week follow-up, 31% more lesions had regressed with the remineralising cream than with the placebo (OR = 2.3, p = 0.04) and the difference between the test and control group was statistically significant.
Two studies compared the effects of resin infiltration (a minimally invasive technique) vs no treatment (control) to treat WSL. One study used the visual analog scale to assess the difference in the WSL at baseline and the 8-week follow-up. The mean visual analog scale ratings for the test group improved significantly compared to the control group at follow-up (65.9 vs 9.2, p < 0.001). The other study assessed resin infiltration vs the control group using a spectrophotometer. In a 6-month follow-up, the results of this study showed that the mean colour difference (8E) of WSL after resin infiltration vs sound adjacent enamel (8E baseline vs 6 months) was 2.55 (95% Cl, 1.431-3.678). The untreated control teeth showed no significant changes over 6 months compared with the baseline: mean (8E) 0.29 (95% Cl-0.335-0.928).
DISCUSSION
A limited number of eligible studies were identified in this review. None of them was adjudged to be at low risk of bias, with most having a high risk of bias either due to inadequacies in several quality items or arising from other biases, chiefly problems associated with assessment methods or inadequate designs. Other shortcomings included small sample sizes, unclear selection criteria, no scores in the case of one study, unreliable statistical analyses that failed to account for clustering effects, and use of unproven assessment methods without relating them to more accepted techniques (eg, visual inspection). Future study designs should include appropriate randomisation, blinding of treatment groups, masking of outcome assessments, rigid eligibility criteria and appropriate analyses to reduce bias. As a result of both the diverse interventions and outcome measures, quantitative synthesis was not possible.
While the remineralizing effects of fluorides and CPP-ACP are well established, this review shows that only limited evidence of the effect of resin infiltration on WSL is available in the literature. The results of the studies included in this review demonstrated that fluorides, when tested against a control, showed positive results and induced improvements in the WSL. The most recent technique of infiltrating WSL with a resin infiltrant exhibited the greatest improvement in the appearance of WSL vs the control group.
Out of the eight studies included in this review, two failed to find significant effects of minimally invasive treatment of WSL as opposed to the control group. One study reported that lack of compliance may be a reason for the insignificant results. Insufficient sample size and a high dropout rate may also affect significance, and of course, there may actually not have been a therapeutic effect.
DIAGNOdent assesses WSL by estimating the organic content and bacterial metabolites in the demineralised lesions. Both studies which assessed the lesions with DIAGNOdent demonstrated significant improvement in the WSL following interventions using fluorides (miswak and varnish, respectively). Whether this was clinically significant was not clear in one study.
It was found that ICDAS criteria of scoring WSL correlated well with DIAGNOdent in two studies which used both of these assessment methods. These studies showed a significant decrease in the severity of WSL scores following use of fluoridated miswak and CPP-ACP.
CPP-ACP has been shown to localise and stabilise calcium and phosphate ions at the tooth surface in a bioavailable form that can promote remineralisation of enamel subsurface lesions in situ, restoring the white opaque appearance of the lesions to translucency, even in the presence of fluoride. The potential of CPP-ACP to prevent enamel demineralisation and promote lesion remineralisation has been demonstrated in animal caries models, in vitro models, human in situ models and clinical trials. Two studies included in this review tested the effects of CPP-ACP and CPP-ACPF on WSL. One study reported a significant difference in the regression of lesions between the test and control group. These results were contradictory to the other study included in this review.
Infiltration of WSL has been established as a new way of stopping or reducing their progression. Paris et al suggested that in the case of post-orthodontic WSL, infiltration treatment should be done as soon as possible after bracket removal, fearing that the lesion at that time is active, would tend to progress and eventually lose its surface integrity. Neither study included in this review mentioned the time elapsed after debonding and before treatment. Time should be allowed to elapse before treating WSL after bracket debonding, as this allows saliva to take effect in healing the tooth. Both studies in this review showed highly significant improvements in the lesions from baseline to follow-up after treatment with resin infiltration. In addition to these randomised clinical trials, other clinical trials have also reported drastic improvement in the aesthetic appearance after masking labial WSL with the resin infiltrant.
CONCLUSION
This systematic review indicated a lack of reliable evidence to support the efficacy of minimally invasive treatment modalities of postorthodontic WSL. Additional high-quality studies with strict eligibility criteria, a combination of specific and sensitive detection methods and reliable statistical analyses are required.
More information about minimally invasive treatment are accessible for you to learn on our website.
REFERENCES
1. Agarwal A, Pandey H, Pandey L, Choudhary G. Effect of fluoridated toothpaste on white spot lesions in postorthodontic patients. Int J Clin Pediatr Dent 2013;6:85-88.
2. Andersson A, Skold-Larsson K, Hallgren A, Petersson LG, Twetman S. Effect of a dental cream containing amorphous cream phosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev Dent 2007;5:229-233.
3. Baeshen HA, Lingstrom P, Birkhed D. Effect of fluoridated chewing sticks (miswaks) on white spot lesions in postorthodontic patients. Am J Orthod Dentofacial Orthop 2011;140:291-297.
4. Bailey DL, Adams GG, Tsao CE, Hyslop A, Escobar K, Manton DJ, Reynolds EC, Morgan MV. Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res 2009;88:1148-1153.
5. Beerens MW, Van Der Veen MH, Van Beek H, Ten Cate JM. Effects of casein phosphopeptide amorphous calcium fluoride phosphate paste on white spot lesions and dental plaque after orthodontic treatment: a 3-month follow-up: effects of CPP-ACFP. Eur J Oral Sci 2010;118:610-617.
6. Cai F, Shen P, Morgan MV, Reynolds EC. Remineralization of enamel subsurface lesions in situ by sugar-free lozenges containing casein phosphopeptide-amorphous calcium phosphate. Aust Dent J 2003;48:240-243.
7. Chang HS, Walsh LJ, Freer TJ. Enamel demineralization during orthodontic treatment. Aetiology and prevention. Aust Dent J 1997;42:322-327.
8. Cochrane NJ, Saranathan S, Cai F, Cross KJ, Reynolds EC. Enamel subsurface lesion remineralisation with casein phosphopeptide stabilised solutions of calcium, phosphate and fluoride. Caries Res 2008;42:88-97.
9. Dirks OB. Posteruptive changes in dental namel. J Dent Res 1966;45:503-511.
10. Du M, Cheng N, Tai B, Jiang H, Li J, Bian Z. Randomized controlled trial on fluoride varnish application for treatment of white spot lesion after fixed orthodontic treatment. Clin Oral lnvestig 2012;16:463-468.
11. Featherstone JD. Diffusion phenomena and enamel caries development. In: Guggenheim B (ed). Proceedings of the Cariology Today International Congress, September 1983, Zurich, Switzerland. Basel: Karger, 1984:259-268.
12. Featherstone JD, Rodgers BE. Effect of acetic, lactic and other organic acids on the formation of artificial carious lesions. Caries Res 1981;15:37 7-385.
13. Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod 1982;81:93-98.
14. Hammad SM, Sanna M, El Zayat I, El Mohsen MA. Effect of resin infiltration on white spot lesions after debonding orthodontic brackets. Am J Dent 2012;25:3-8.
15. lijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. Caries Res 2004;38:551-556.
16. Karlinsey RL, Mackey AC, Stookey GK, Pfarrer AM. In vitro assessments of experimental NaF dentifrices containing a prospective calcium phosphate technology. Am J Dent 2009;22:180-184.
17. Knosel M, Eckstein A, Helms H-J. Durability of esthetic improvement following Icon resin infiltration of multibracket-induced white spot lesions compared with no therapy over 6 months: A single-center, split-mouth, randomized clinical trial. Am J Orthod Dentofacial Orthop 2013;144: 86-96.
18. Lee J-H, Kim D-G, Park C-J Cho L-R. Minimally invasive treatment for esthetic enhancement of white spot lesion in adjacent tooth. J Adv Prosthodont 2013;5:359.
19. Loesche WJ. Chemotherapy of dental plaque infections. Oral Sci Rev 1976;9:65-107.
20. Malterud Ml. Minimally invasive restorative dentistry: a biomimetic approach. Pract Proced Aesthetic Dent 2006;18:409-414.
21. Meyer-Lueckel H, Paris S. Improved resin infiltration of natural caries lesions. J Dent Res 2008;87:1112-1116.
22. Morgan MV, Adams GG, Bailey DL, Tsao CE, Fischman SL, Reynolds EC. The anticariogenic effect of sugar-free gum containing CPP-ACP nanocomplexes on approximal caries determined using digital bitewing radiography. Caries Res 2008;42:171-184.
23. Paris S, Meyer-Lueckel H. Masking of labial enamel white spot lesions by resin infiltration-a clinical report. Quintessence Int 2009;40:713-718.
24. Paris S, Meyer-Lueckel H, Colfen H, Kielbassa AM. Resin infiltration of artificial enamel caries lesions with experimental light curing resins. Dent Mater J 2007;26: 582-588.
25. Paris S, Meyer-Lueckel H, Kielbassa AM. Resin infiltration of natural caries lesions. J Dent Res 2007;86:662-666.
26. Reynolds EC. Remineralization of enamel subsurface lesions by casein phosphopeptide-stabilized calcium phosphate solutions. J Dent Res 1997;76:1587-1595.
27. Reynolds EC. The prevention of sub-surface demineralization of bovine enamel and change in plaque composition by casein in an intra-oral model. J Dent Res 1987;66: 1120-1127.
28. Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, Reynolds C. Fluoride and casein phosphopeptideamorphous calcium phosphate. J Dent Res 2008;87: 344-348.
29. Reynolds EC, Cai F, Shen P, Walker GD. Retention in plague and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gum. J Dent Res 2003;82:206-211.
30. Reynolds EC, Cain CJ, Webber FL, Blacson IH, Perich JW. Anticariogenicity of calcium phosphate complexes of tryptic casein phosphopeptides in the rat. J Dent Res 1995;74:1272-1279.
31. Rodrigues JA, Lussi A, Seemann R, Neuhaus KW. Prevention of crown and root caries in adults. Periodontal 2000 2011;55:231-249.
32. Senestraro SV, Crowe JJ, Wang M, Vo A, Huang G, Ferracane J, Covell DA. Minimally invasive resin infiltration of arrested white-spot lesions: a randomized clinical trial. J Am Dent Assoc 2013;144:997-1005.
33. Shen P, Cai F, Nowicki A, Vincent J, Reynolds EC. Remineralization of enamel subsurface lesions by sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. J Dent Res 2001;80:2066-2070.
34. Stahl J, Zandona AF. Rationale and protocol for the treatment of non-cavitated smooth surface carious lesions. Gen Dent 2007;55:105-111.
35. Sudjalim T, Woods M, Manton D. Prevention of white spot lesions in orthodontic practice: a contemporary review. Aust Dent J 2006;51:284-289.
36. Summitt JB. Fundamentals of Operative Dentistry: A Contemporary Approach. Chicago: Quintessence, 2006.
37. Torres CRG, Rosa PCF, Ferreira NS, Borges AB. Effect of caries infiltration technique and fluoride therapy on microhardness of enamel carious lesions. Oper Dent 2012;37: 363-369.
38. Walker G, Cai F, Shen P, Reynolds C, Ward B, Fane C, Honda S, Koganei M, Oda M, Reynolds E. Increased remineralization of tooth enamel by milk containing added casein phosphopeptide-amorphous calcium phosphate. J Dairy Res 2006;73:74-78.
39. Will mot D. White spot lesions after orthodontic treatment. Semin Orthod 2008;14:209-219.
40. Willmot DR. White lesions after orthodontic treatment: does low fluoride make a difference? J Orthod 2004;31: 235-242.

Video
OHI-S
02 April 2024
Video
OHI-S
16 January 2024

Video
OHI-S
21 November 2023


