Examination of a patient with pathology of the maxillofacial area
Machine translation
Original article is written in RU language (link to read it) .
A clinical examination of a patient with surgical pathology of the maxillofacial area is a set of techniques necessary to establish the individual characteristics of the patient, which is important for making the correct diagnosis, choosing the appropriate treatment tactics, monitoring the dynamics of the disease, and predicting the final result.
A detailed algorithm for clinical examination for pathology in the maxillofacial area at the webinar Temporomandibular disorders: clinical examination and differential diagnosis .
Clinical examination consists of a combination of the following stages:
identification of complaints, medical history;
visual examination, palpation and percussion examination;
instrumental examination;
laboratory diagnostics,
radiography;
morphological studies.

Figure 1. Patient examination.
Patient interview
At this stage, it is important to establish the patient’s neuropsychic state and level of intellectual development; based on this, one should begin to analyze complaints and the history of the disease.
Patient complaints are varied:
painful sensations,
edema and swelling,
the appearance of deformations and defects.
When a patient complains of pain, it is necessary to find out the following characteristics:
the cause of its appearance (permanent or provoked by certain stimuli);
nature of the pain (aching, sharp, burning, etc.);
intensity;
duration (attacks of pain or is it constant);
localization;
biorhythmicity.
If a patient has swelling, the following factors should be determined:
when it arose
whether it is increasing in size or stable,
Is there any pain in the area of swelling? If so, then evaluate all the characteristics of the pain.

Figure 2. Radiograph evaluation.
An assessment of all these indicators will help to make a differential diagnosis of various diseases, traumatic lesions, and tumor processes.
If a patient is diagnosed with a violation of the integrity or deformation of soft or hard tissues in the dental system, which are the cause of functional and cosmetic disorders, the doctor needs to establish their origin:
they are congenital or appeared after birth,
what pathological process provoked their occurrence (trauma, inflammation, neoplasm, previous operations).
History of the disease
At this stage, the duration of the disease, initial symptoms, the patient’s opinion regarding the cause of its appearance, the dynamics of the pathological process, and therapeutic measures are established.
If there is documentation regarding previous treatment or examination (medical history, laboratory diagnostic results, radiography), it is necessary to take them into account.
If you have suffered an injury, you should establish:
circumstances when and where the injury occurred,
was there a loss of consciousness, for what period of time,
whether there was vomiting and nausea,
did you have any dizziness?
Has there been any bleeding from the nose, ears,
was first aid provided, its volume,
whether the patient visited a medical institution,
what kind of help he received there.

Figure 3. Palpation of lymph nodes.
In case of neurogenic pain, the patient’s neurological status is clarified; if bleeding occurs, information is collected on the duration of bleeding after previous injuries, operations, or tooth extraction.
When clarifying the life history, it is necessary to determine the presence of bad habits, chronic and infectious diseases and surgical interventions, and the presence of allergies in the patient.
Patient examination
If the patient's condition is assessed as satisfactory, he is examined in a dental chair. If the patient is in serious condition, then the examination can be carried out on the operating table, on the couch, or with the dental chair laid out horizontally.
Tools required for clinical examination of a patient:
A spatula is used to remove overhanging soft tissue so that it does not interfere with examination.
Dental tweezers help assess tooth mobility and can be used to perform percussion.
A dental mirror allows you to examine the teeth and difficult-to-examine parts of the patient’s oral cavity: the back third of the tongue, the palate, the sublingual space.
A dental probe (bayonet-shaped or angular) is used to measure the depth of pathological pockets and the presence of defects in teeth.
Bauman probe, thin injection needles with a blunt tip, salivary catheters made of polyethylene - all this is used to examine fistula tracts and salivary ducts.
The button probe can be used to examine fistulas, oroantral communications, assess wound depth, and assess palate and bone injuries.
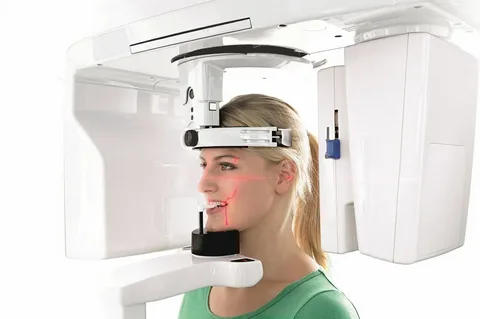
Figure 4. X-ray diagnostics.
Examining the outer integument, the doctor pays attention to the symmetry of the face; when establishing asymmetry, its nature is studied, and the reasons that caused it are established (swelling, inflammation, deformation, neoplasm). There is a change in the condition of the skin (coloring, turgor), the appearance of fistulous tracts on the skin, the presence and characteristics of the discharge.
During the examination, scars, the condition of the lips, the coloring of the red border, the symmetry of the corners of the mouth, and the amount of mouth opening are noted.
Palpation
Palpation is a diagnostic examination technique that, through palpation, allows one to evaluate parts of the patient’s body. In the process of palpating the soft tissues, the consistency of the swelling area, the presence of pain, mobility, area of localization, cohesion with the underlying sections (is it possible to fold the skin in the area of swelling), areas of softening and fluctuations are established.
True fluctuation is diagnosed in several mutually perpendicular directions; if fluctuation is detected in a single direction, it is most likely to be false.
All irregularities and areas of bone thickening are palpated, their soreness and symmetry are revealed, and sizes are calculated.
Palpation of lymph nodes
The lymph nodes are palpated separately, and the following indicators are assessed during the process:
consistency,
soreness,
sizes.
Acute inflammation of the lymph nodes is characterized by:
rapid increase in size,
acute pain,
mobility is limited,
sometimes fluctuation occurs.
With chronic inflammation, the lymph nodes:
their mobility is preserved,
mild pain,
increase in size slowly.
Techniques for palpation of different groups of lymph nodes
Cervical, posterior ear, submandibular - with one hand the surgeon tilts the patient’s head downwards, with the other he consistently palpates the lymph nodes with three fingers.
Submental - palpated in the same position only with the index finger.
Submandibular, buccal, nasolabial - palpated bimanually. During this manipulation, the fingers of one hand are placed on the side of the oral cavity, the other on the side of the skin.
Parotid - palpated with several fingers in the area of the branch of the lower jaw, or bimanually - in the projection of the parotid glands.
Supraclavicular - the doctor stands behind the patient, palpating with three fingers located on the collarbone.
Bite assessment
The bite is classified as physiological or pathological. Physiological occlusion is a position of the teeth on both jaws when there is maximum contact between the teeth, which guarantees an aesthetic appearance and the performance of chewing function.
Physiological occlusions are orthogenic and orthognathic. A direct or orthogenic bite is characterized by contact of the cutting edges of the lower incisors and canines with the cutting edges of the corresponding upper teeth.
With an orthognathic bite, all teeth, with the exception of the lower first incisors and upper third molars, are in contact with the teeth of the same name and adjacent teeth, while the teeth of the upper jaw overlap the lower teeth with the buccal cusps of the lateral teeth and the cutting edges of the anterior ones.
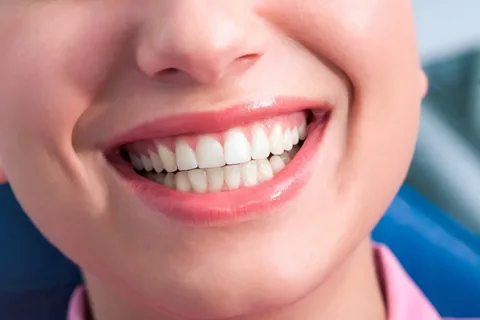
Figure 5. Occlusion assessment.
In the case of a pathological bite, the appearance changes and the functioning of the dentition is disrupted. The following types of pathological bite are distinguished:
biprognathic - the anterior teeth and alveolar processes of both jaws have anterior deviation;
deep – the incisors on opposite jaws deeply overlap each other, there is no proper contact between the occlusal and cutting surfaces of the teeth;
distal - the upper canines and incisors are located anterior to the lower teeth of the same name;
mesial - the lower incisors and canines are located anterior to the upper teeth of the same name.
This completes the clinical examination and begins additional examinations.
An example of a questionnaire for examining cranial nerves at the webinar Neurological examination .

