Micro‐CT assessment of radicular pulp calcifcations in extracted maxillary frst molar teeth
Abstract
Objectives: The present study aimed to evaluate the frequency, position, and length of radicular pulp calcifications in three-rooted maxillary first molars using micro-computed tomography.
Materials and methods: Two hundred three-rooted maxillary first molars were scanned at a pixel size of 10 µm and reconstructed using similar parameters. Three-dimensional models of the mesiobuccal (MB1, MB2, MB3), distobuccal (DB), and palatal (P) canals were qualitatively evaluated for discontinuity in the canal path. Transaxial and sagittal cross-sectional images of the roots were further screened, and the complete obliteration of the canal lumen by pulp calcification was identified when the canal had similar radiodensity to the surrounding dentine. Then, the number, position, and length of the calcifications were recorded for each root. Intra-observer agreement was performed using Cohen’s kappa test, while one-way ANOVA and Duncan tests compared the lengths of calcifications among the canals, with α = 5%.
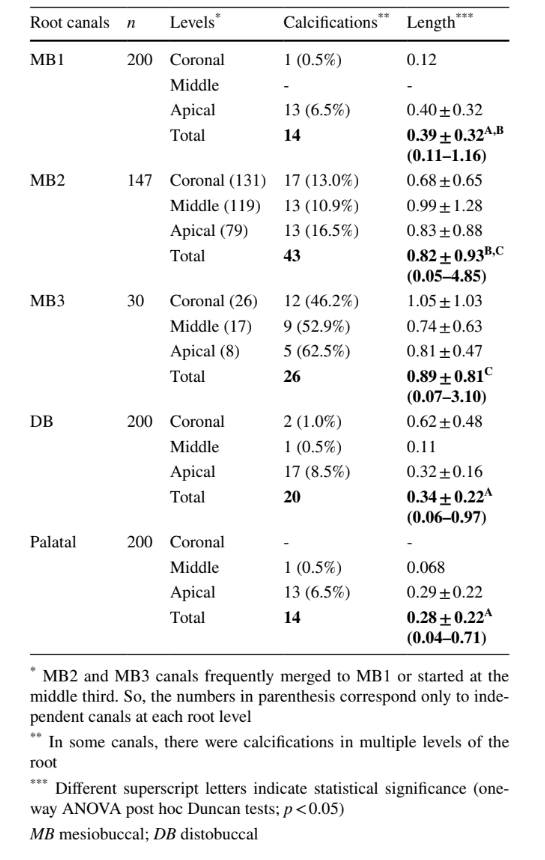
Results: Intra-observer agreement was perfect for identification of pulp calcifications (ĸ = 1.0; p = 0.000). MB2 and MB3 canals accounted for the highest percentage frequency of calcifications distributed throughout the canal path. In the MB1, DB, and P canals, they occurred mainly at the apical third. Lengths of calcifications were greater in the MB3 (0.89 ± 0.81 mm) and MB2 (0.82 ± 0.93 mm) canals than in the MB1 (0.39 ± 0.32 mm), DB (0.34 ± 0.22 mm), and P (0.28 ± 0.22 mm) canals (p < 0.05).
Conclusion: MB2 and MB3 canals accounted for the highest frequency and length of radicular pulp calcifications. In the MB1, DB, and P canals, calcifications occurred mostly at the apical third, while in the MB2 and MB3, most of calcifications were observed at the orifice level and along the canal path.
Clinical relevance: In maxillary first molars, radicular pulp calcifications are mainly located at the apical third of the MB1, DB, and P canals, while in the MB2 and MB3 canals, most of them are at the orifice level or along the canal path.
Introduction
Dental pulp calcifications are hard tissue formations developed within the dental pulp tissue or on the dentine/pulp interface. In the literature, depending on the histomorphology and aetiology, a myriad of terms and expressions have been used to designate this condition including pulp stone, denticle, dystrophic calcification, calcific metamorphosis, pulp canal obliteration, obliteration, pulp cavity calcifying process, reduced pulpal lumen, pulp calcification, calcific pulp obliteration, and pulp canal sclerosis. The prevalence of this phenomenon varies widely (8 to 95%), depending on the population, study design, and the method of analysis, but it has been estimated that one or more calcifications are present in at least 50% of all teeth, mostly in molars. The true prevalence, however, is likely to be higher considering that calcifications less than 200 µm cannot be detected in radiographs, the most used analytical method.
The aetiology of dental pulp calcification has been associated with trauma, aging, orthodontic treatment, caries, periodontal disease, operative procedures, pulp inflammation, and systemic diseases and genetic conditions, such as imperfect dentinogenesis, dentine dysplasia, cardiac and kidney disease, Marfan syndrome, and William syndrome. Some authors believe that pulp calcification represents a form of dystrophic calcification, a type in which calcium is deposited in degenerating tissues. However, it is not possible to assign this term to all calcifications observed within the root canal system considering they were also observed in healthy and even unerupted or impacted teeth, suggesting that functional stress does not need to exist for calcification to occur. Depending on its location, calcified pulp tissue was also classified into pulp chamber or radicular calcifications. The former includes regular or irregular forms of secondary or tertiary dentine that are deposited on the dentinal walls, while the latter is formed primarily within the pulp tissue and comprises true or false denticles that can spread and grow until the complete obstruction of the canal lumen. In a clinical setup, if endodontic treatment becomes necessary, the presence of calcifications narrowing or even completely obliterating the root canal space can turn this procedure into a significant challenging task. For instance, while pulp chamber calcifications may compromise access cavity preparation and orifice location, radicular pulp calcifications may deflect or engage the tip of instruments, preventing their passage along the canal path. Interestingly, although calcifications may potentially be the primary cause of missed canals, perforation, or instrument separation, most studies that investigated outcomes of root canal treatment or reasons for tooth extraction did not focus on this eventually impairing parameter.
In the literature, the evaluation of pulp tissue calcification has been mostly performed by using histology or radiographic exams. While histology is time-consuming, is expensive, is destructive, and allows only a few sections per root to be assessed, drawbacks of conventional radiographs include limited resolution, shadows, anatomical noise, geographical distortion, overlapping, elongation, or depression of root canals. Nowadays, these limitations were overcome using non-destructive high-resolution imaging tools. Although we were unable to find any specific study on dental pulp calcification using cone-beam computed tomography (CBCT) imaging, there are several reports on its successful use as an adjunctive aid to treat calcified canals. But CBCT data on calcified teeth seems variable and dependent on the operator experience, leaving a dubious perspective on the reliability of the available devices for the study of pulp calcifications. In the last decade, micro-computed tomographic technology (micro-CT) has arisen as gold standard for the study of dental hard tissues and root canals because of its higher resolution and accuracy to detect even small morphological details of teeth. In the literature, however, studies using this non-destructive tool reported the presence of calcifications within the root canal system only as a secondary finding. Therefore, the aim of present study was to evaluate the frequency, position, and length of radicular pulp calcifications that completely obliterate the canal lumen in 200 extracted three-rooted maxillary first molars using high-resolution micro-CT imaging.
Materials and methods
After approval of this research project by the University Research Ethics Committee (Protocol 2015/408), two hundred three-rooted maxillary first molar teeth—extracted for reasons not related to this study—presenting no deep caries or restoration, severe abrasion, previous root canal treatment, incomplete root formation, fracture, resorption, or root fusion were collected, cleaned, and radiographed in both mesiodistal and buccolingual directions. Patients’ age and gender were unknown. All specimens were scanned in a micro-CT device (Skyscan 1172; Bruker-microCT, Kontich, Belgium) at 100 kV, 100 µA, pixel size of 10 µm, and 180° rotation around the vertical axis with steps of 0.6°, using an aluminium-copper alloy filter. The acquired projection images were reconstructed with similar parameters for smoothing (3), ring artefact correction (6), contrast limits (0.009–0.018), and beam hardening correction (15%) with NRecon v.1.7.1.1 software (Bruker-microCT).
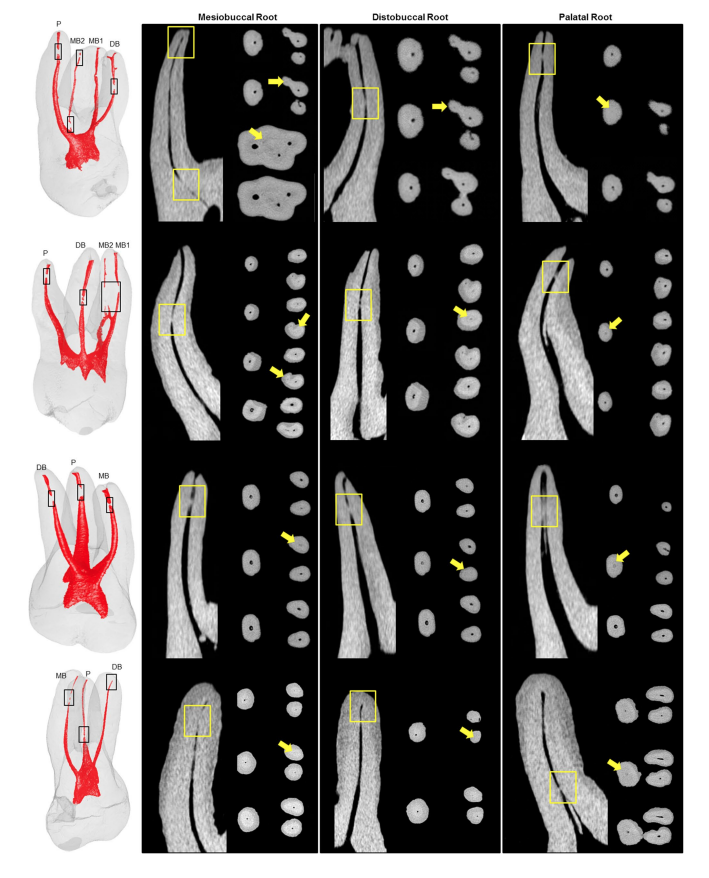
Three-dimensional models of the roots and root canal systems were created using CTAn v.1.17.7.2 (Bruker-microCT) and qualitatively evaluated for canal configuration with CTVol v.2.3.2.0 (Bruker-microCT) and for discontinuity of the root canal space with DataViewer v.1.5.6.2 (Bruker- microCT). Transaxial and sagittal cross-sectional images of these areas were further screened (CTAn v.1.17.7.2 and DataViewer v.1.5.6.2; Bruker-microCT), and radicular pulp calcifications were identified when the canal lumen was completely obliterated, i.e., had similar density to the surrounding dentine tissue in both transaxial and sagittal cross-sections (Fig. 1).
Then, the frequency and position (coronal, middle, or apical thirds) of the calcifications were recorded for the mesiobuccal (MB1), distobuccal (DB), and palatal (P) canals. If present, the second (MB2) and third (MB3) root canals of the mesiobuccal root were also evaluated. The lengths of calcifications (in millimetres) were measured using CTAn v.1.17.7.2 (Bruker-microCT) using the formula (Sf – Si)/PS, where Sf and Si are the final and initial transaxial slices (in the z-axis) in which it is possible to observe the calcification, and PS is the scanning pixel size (0.010 mm). The lengths of the calcifications were compared among the root canals using the one-way analysis of variance post hoc Duncan test at a significance level of 5%. All evaluations were performed by a single operator with 10 years of experience in the analysis of micro-CT scans. Intra-examiner reliability for the assessment of the complete obliteration of the root canal lumen was verified using the Cohen’s kappa test with a 5% level of significance. In this analysis, one hundred twenty-five micro-CT cross-sections containing 150 root canals (with and without calcifications) were selected and appraised by the same observer after a 5-month interval.
Results
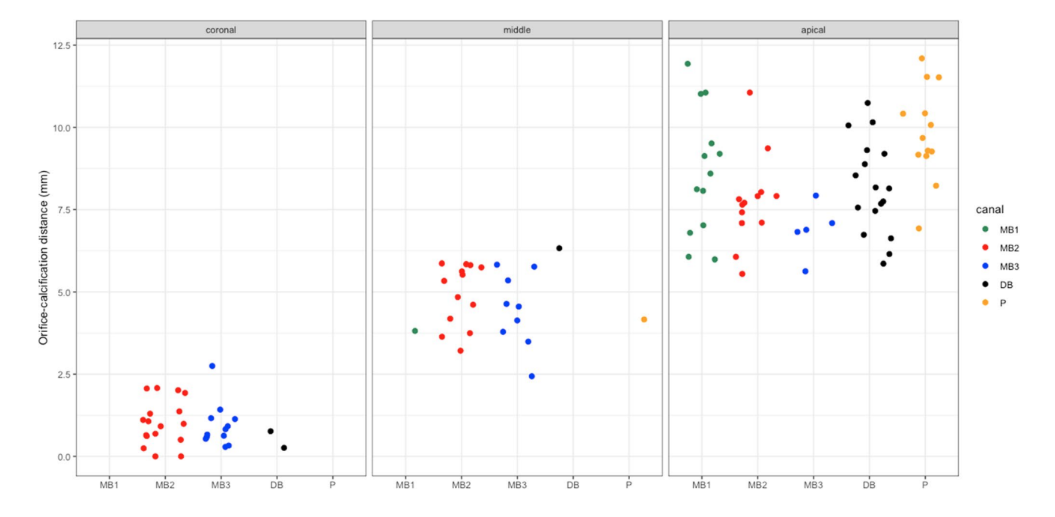
A total of 174,476 transaxial slices (mean of 872 per tooth) acquired by scanning 200 three-rooted maxillary first molars were screened in this study. Percentage frequency, location, and length of radicular pulp calcifications observed in each root canal are presented in Table 1. Because of their heterogeneous levels of crystallinity and chemical composition, pulp calcifications sometimes appeared slightly different from dentine in terms of radiographic density in some cross-sectional images. Despite of it, intra-examiner reliability was perfect for identification of pulp calcifications (ĸ = 1.0, Cohen’s kappa; p = 0.000). MB2 and MB3 canals accounted for the highest percentage frequency of calcifications, similarly distributed throughout the canal path, while in the MB1, DB, and P canals, they were observed mostly at the apical third (Figs. 1 and 2). The mean lengths of calcifications in the MB3 (0.89 ± 0.81 mm) and MB2 (0.82 ± 0.93 mm) canals were similar (p > 0.05), but greater than in the MB1 (0.39 ± 0.32 mm), DB (0.34 ± 0.22 mm), and P (0.28 ± 0.22 mm) canals (p < 0.05).
cal third
Discussion
In the literature, most studies reported the prevalence of pulp calcifications in different groups of teeth and populations. Overall, a high prevalence of pulp calcification was reported in maxillary posterior teeth, especially in first molars, the type of tooth evaluated in the present study. Although the reason for this high prevalence is still unclear, it has been explained by their early eruption, which would expose them to more degenerative changes over time, and their high blood perfusion, also considered as a contributing factor to form calcifications. Pulp calcifications have been also described as true (resembling dentine), false (composed of localized masses of calcified material), or diffuse (often found near blood vessels), but no attempt was made herein to classify them, as it would demand a destructive method of analysis. On the other hand, the present study overcome the main limitations of other analytical methods—such as image overlapping and distortion—by using the non-destructive gold standard micro-CT technology to evaluate 200 maxillary first molars at a pixel size of 10 µm. This method was successfully employed to analyse reduced pulp cavities by mineralized pulp tissues and to identify radicular calcifications in non-instrumented canals of mandibular molars. After image acquisition, 174,476 transaxial slices were screened to calculate the frequency, location, and length of radicular pulp calcifications that completely obliterate the canal lumen. This is an innovative and original approach once, so far, no research using radiograph, micro-CT, or CBCT imaging methods was designed specifically to address this morphological condition within the radicular pulp tissue of maxillary molars.
In the present study, different patterns regarding length and location of calcifications were observed. In the MB1, DB, and P canals, calcifications were smaller and located mostly at the apical third, while MB2 and MB3 canals accounted for their highest number, distributed throughout the canal length (Table 1, Fig. 2). Notwithstanding the impossibility to compare these findings with previous publications, they are in accordance with 2 previous studies that reported sporadic accumulations of mineral deposits in the radicular pulp tissue of maxillary molars distributed through the coronal, middle, and apical thirds, using micro-CT technology. Unfortunately, the aetiological factors and the biological mechanisms involved in the formation of calcifications are still not fully understood, but some authors have correlated it with longstanding local irritants, aging, and progressive periodontal disease. Although care was taken to include teeth with an overall preserved structure, it is likely that some of the present findings were related to these factors. It would be logical to assume that teeth fulfilling the inclusion criteria would have been extracted due to orthodontic, prosthodontic, or periodontal reasons. Regarding the latter, while some histopathological studies has linked moderate and severe periodontal problems with pulpal changes, such as inflammation and dystrophic calcification, others showed no significant changes within the pulp tissue, even in the presence of advanced periodontal disease. These dissimilarities are possibly related to the unfeasibility to obtain a proper control group (periodontally healthy teeth) using the available destructive methods. In the future, however, it is likely that results from well-controlled in vivo studies using high-resolution nondestructive imaging methods clarify this contradictory issue. In this study, no data were available on the origin of teeth and, therefore, it was not possible to provide a proper explanation for the different distribution patterns of calcifications observed among the root canals.
In clinics, reduction or obliteration of the canal lumen by calcifications can compromise the accessibility of the endodontic instruments to the canal terminus and, consequently, influence treatment outcome. In the literature, there are limited data regarding the prognosis of treatment performed in calcified teeth in response to other factors than trauma. Wu et al. demonstrated that only 49.3% of canals with calcifications at the apical third could be successfully negotiated even with the aid of an operating microscope. Another study designed to evaluate the treatment outcome of 114 calcified root canals reported that working length was achieved in 90% of the cases with a success rate of 80% after a follow-up period of 3 years. But, in elderly patients, endodontic treatment of calcified canals resulted in an overall success rate of 89% after 2 to 12 years, decreasing to 62.5% when considering teeth with apical periodontitis. Taken together, the results of these studies suggest that pulp calcification is an important factor that may affect treatment outcome. Therefore, it would be important to address some clinical implications of radicular pulp calcifications on the light of the present results.
At the orifice level, calcifications can render locating the root canals more difficult, and their length, an aspect poorly explored in previous studies, can be considered of high relevance in practice. In this study, the highest prevalence of calcifications at the coronal and middle thirds were observed in the MB2 (13.0% and 10.9%, respectively) and MB3 (46.2% and 52.9%, respectively) canals, while their lengths reached up to 4.85 mm and 3.10 mm, respectively (Table 1). Previous anatomical studies showed that MB2 and MB3 orifices are often hidden under the shelf of the dentine wall or under calcified tissues in a small groove. Consequently, they can be missed in routine clinical practice, a condition considered the major cause of treatment failure in maxillary molars. At the apical canal, depending on the length of the calcification, reach the working length or establish patency can be tricky, time-consuming, and, sometimes, unfeasible. Besides, the inaccessibility of the apical anatomy may significantly impair the outcome of canal treatment, especially in the presence of pulp necrosis. In the present study, most of the calcifications were observed at the apical third of MB1, DB, and P canals (Table 1, Fig. 2), while MB2 and MB3 canals accounted for their highest percentage frequencies (16.5% and 62.5%, respectively), supporting the findings of a previous publication that reported difficulty to achieve patency in these root canals.
From a clinical perspective, complications may arise during location and negotiation of calcified canals including perforation, instrument separation, excessive weakening of tooth structure, inability to reach working length, and deviation from the original canal path. In this way, several strategies have been proposed to reduce the risk of an iatrogenic event by using endodontic explorers, special burs, thin ultrasonic tips, and visual inspection of root canals with high illumination and magnification. Additional approaches include the use of dyes, such as methylene blue, or placing sodium hypochlorite into the pulp chamber to observe a stream of bubbles emerging from the oxygenation of the pulp tissue remnants. In very deep access preparations, it would be also helpful to take radiographs from multiple angles to maintain the alignment and direction of the files when scouting calcified canals. A preoperative CBCT scan is extremely important in most cases, but nowadays, intraoperative CBCT examination was also recommended for complex cases. This approach aimed to set boundaries and to evaluate the benefit/risk ratio for the best interest of the patient’s care, mostly when apical pathosis is not present and the risks of attempting to expose a completely calcified canal are unjustifiable. Another innovative purpose was the use of intra-oral CBCT scans to produce templates to help locating the canal path in calcified teeth. More recently, it was also demonstrated the feasibility of a new multisonic device to remove embedded calcifications from distal canals of mandibular molars by combining the effects of washing (loose calcifications), energy (cavitation), and dissolving action of irrigants.
Limitations of the current study include the lack of knowledge regarding age, gender, use of medication, and systemic diseases of teeth donors, as well as the reasons for extraction and the pulp and periapical status of teeth. On the other hand, the use of a non-destructive and accurate analytical tool that allowed the identification and measurement of pulp calcifications throughout hundreds of cross-sectional slices obtained from a large number of maxillary first molars (n = 200) with well-preserved hard tissue structures constitute the strengths of this study. Future investigations are warranted to examine the association of pulp calcifications with local and systemic factors, to evaluate the effect of this anatomical condition on treatment outcome, and also to propose technical strategies to overcome this condition in a clinical setup.
Conclusion
In maxillary first molars, MB2 and MB3 canals accounted for the highest frequency and length of radicular pulp calcifications. In the MB1, DB, and P canals, calcifications occurred mainly at the apical third, while in the MB2 and MB3 canals, most of calcifications were observed at the orifice level and along the canal path.
Authors: Ali Keleş, Cangül Keskin, Marco Aurélio Versiani
References:
- Carvalho TS, Lussi A (2017) Age-related morphological, histological and functional changes in teeth. J Oral Rehabil 44:291–298. https://doi.org/10.1111/joor.12474
- McCabe P, Dummer PMH (2012) Pulp canal obliteration: an endodontic diagnosis and treatment challenge. Int Endod J 45:177–197. https://doi.org/10.1111/j.1365-591.2011.01963.x
- Bastos JV, Côrtes MIS (2018) Pulp canal obliteration after traumatic injuries in permanent teeth - scientific fact or fiction? Braz Oral Res 32:e75. https://doi.org/10.1590/1807-3107bor-2018. vol32.0075
- Chen B, Szabo D, Shen Y, Zhang D, Li X, Ma J, Haapasalo M (2020) Removal of calcifications from distal canals of mandibular molars by a non-instrumentational cleaning system: a micro-CT study. Aust Endod J 46:11–16. https://doi.org/10.1111/aej.12376
- Tamse A, Kaffe I, Littner M, Shani R (1982) Statistical evaluation of radiologic survey of pulp stones. J Endod 8:455–458. https:// doi.org/10.1016/S0099-2399(82)80150-7
- Moss-Salentijn L, Klyvert MH (1983) Epithelially induced denticles in the pulps of recently erupted, noncarious human premolars. J Endod 9:554–560. https://doi.org/10.1016/S0099-2399(83) 80060-0
- Baghdady VS, Ghose LJ, Nahoom HY (1988) Prevalence of pulp stones in a teenage Iraqi group. J Endod 14:309–311. https://doi. org/10.1016/S0099-2399(88)80032-3
- Şener S, Cobankara FK, Akgünlü F (2009) Calcifications of the pulp chamber: prevalence and implicated factors. Clin Oral Invest 13:209–215. https://doi.org/10.1007/s00784-008-0212-x
- Goga R, Chandler NP, Oginni AO (2008) Pulp stones: a review. Int Endod J 41:457–468. https://doi.org/10.1111/j.1365-2591. 2008.01374.x
- Luukko K, Kettunen P, Fristad I, Berggreen E (2011) Structure and functions of the dentin-pulp complex. In: Hargreaves KM, Cohen S (eds) Cohen’s Pathways of the Pulp, 10th edn. Mosby, St. Louis, pp 283–348
- da Silva EJNL, Prado MC, Queiroz PM, Nejaim Y, Brasil DM, Groppo FC, Haiter-Neto F (2017) Assessing pulp stones by cone-beam computed tomography. Clin Oral Investig 21:2327–2333. https://doi.org/10.1007/s00784-016-2027-5
- Taşsöker M, Magat G, Şener S (2018) A comparative study of cone-beam computed tomography and digital panoramic radiography for detecting pulp stones. Imaging Sci Dent 48:201–212. https://doi.org/10.5624/isd.2018.48.3.201
- Milcent CPF, da Silva TG, Baika LM, Grassi MT, Carneiro E, Franco A, de Lima AAS (2019) Morphologic, structural, and chemical properties of pulp stones in extracted human teeth. J Endod 45:1504–1512. https://doi.org/10.1016/j.joen.2019.09.009
- Langeland K, Rodrigues H, Dowden W (1974) Periodontal disease, bacteria, and pulpal histopathology. Oral Surg Oral Med Oral Pathol 37:257–270. https://doi.org/10.1034/j.1600-051x. 2002.290801.x
- Li L, Zhu YQ, Jiang L, Peng W, Ritchie HH (2011) Hypoxia promotes mineralization of human dental pulp cells. J Endod 37:799–802. https://doi.org/10.1016/j.joen.2011.02.028
- Fleig S, Attin T, Jungbluth H (2017) Narrowing of the radicular pulp space in coronally restored teeth. Clin Oral Invest 21:1251– 1257. https://doi.org/10.1007/s00784-016-1899-8
- Bernick S, Nedelman C (1975) Effect of aging on the human pulp. J Endod 1:88–94. https://doi.org/10.1016/S0099-2399(75) 80024-0
- Kannan S, Kannepady SK, Muthu K, Jeevan MB, Thapasum A (2015) Radiographic assessment of the prevalence of pulp stones in Malaysians. J Endod 41:333–337. https://doi.org/10.1016/j. joen.2014.10.015
- Çolak H, Çelebi AA, Hamidi MM, Bayraktar Y, Çolak T, Uzgur R (2012) Assessment of the prevalence of pulp stones in a sample of Turkish central anatolian population. Sci World J 804278:1–7. https://doi.org/10.1100/2012/804278
- De-Deus G, Belladonna FG, Cavalcante DM, Simoes-Carvalho M, Silva E, Carvalhal JCA, Zamolyi RQ, Lopes RT, Versiani MA, Dummer PMH, Zehnder M (2021) Contrast-enhanced micro-CT to assess dental pulp tissue debridement in root canals of extracted teeth: a series of cascading experiments towards method validation. Int Endod J 54:279–293. https://doi.org/10.1111/iej.13408
- Yang YM, Guo B, Guo LY, Yang Y, Hong X, Pan HY, Zou WL, Hu T (2016) CBCT-aided microscopic and ultrasonic treatment for upper or middle thirds calcified root canals. Biomed Res Int 2016:1–9. https://doi.org/10.1155/2016/4793146
- Ball RL, Barbizam JV, Cohenca N (2013) Intraoperative endodontic applications of cone-beam computed tomography. J Endod 39:548–557. https://doi.org/10.1016/j.joen.2012.11.038
- Hsieh CY, Wu YC, Su CC, Chung MP, Huang RY, Ting PY, Lai CK, Chang KS, Tsai YC, Shieh YS (2018) The prevalence and distribution of radiopaque, calcified pulp stones: A cone-beam computed tomography study in a northern Taiwanese population. J Dent Sci 13:138–144. https://doi.org/10.1016/j.jds.2017.06.005
- Zhang D, Chen J, Lan G, Li M, An J, Wen X, Liu L, Deng M (2017) The root canal morphology in mandibular first premolars: a comparative evaluation of cone-beam computed tomography and micro-computed tomography. Clin Oral Investig 21:1007–1012. https://doi.org/10.1007/s00784-016-1852-x
- Borges CC, Estrela C, Decurcio DA, Pécora JD, Sousa-Neto MD, Rossi-Fedele G (2020) Cone-beam and micro-computed tomography for the assessment of root canal morphology: a systematic review. Braz Oral Res 34:e056. https://doi.org/10.1590/1807- 3107bor-2020.vol34.0056
- Ordinola-Zapata R, Bramante CM, Versiani MA, Moldauer BI, Topham G, Gutmann JL, Nuñez A, Duarte MA, Abella F (2017) Comparative accuracy of the clearing technique, CBCT and Micro-CT methods in studying the mesial root canal configuration of mandibular first molars. Int Endod J 50:90–96. https://doi. org/10.1111/iej.12593
- Markvart M, Bjørndal L, Darvann TA, Larsen P, Dalstra M, Kreiborg S (2012) Three-dimensional analysis of the pulp cavity on surface models of molar teeth, using X-ray micro-computed tomography. Acta Odontol Scand 70:133–139. https://doi.org/10. 3109/00016357.2011.600707
- Park JW, Lee JK, Ha BH, Choi JH, Perinpanayagam H (2009) Three-dimensional analysis of maxillary first molar mesiobuccal root canal configuration and curvature using micro–computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:437–442
- Berès F, Isaac J, Mouton L, Rouzière S, Berdal A, Simon S, Dessombz A (2016) Comparative physicochemical analysis of pulp stone and dentin. J Endod 42:432–438. https://doi.org/10. 1016/j.joen.2015.11.007
- Jannati R, Afshari M, Moosazadeh M, Allahgholipour SZ, Eidy M, Hajihoseini M (2019) Prevalence of pulp stones: a systematic review and meta-analysis. J Evid Based Med 12:133–139. https:// doi.org/10.1111/jebm.12331
- Shahbazian M, Vandewoude C, Wyatt J, Jacobs R (2014) Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin Oral Invest 18:293–300. https://doi.org/10.1007/s00784-013-0963-x
- Burke FM, Samarawickrama DY (1995) Progressive changes in the pulpo-dentinal complex and their clinical consequences. Gerodontology 12:57–66. https://doi.org/10.1111/j.1741-2358.1995. tb00132.x
- Gautam S, Galgali SR, Sheethal HS, Priya NS (2017) Pulpal changes associated with advanced periodontal disease: a histo-pathological study. J Oral Maxillofac Pathol 21:58–63. https:// doi.org/10.4103/0973-029X.203795
- Fatemi K, Disfani R, Zare R, Moeintaghavi A, Ali SA, Boostani HR (2012) Influence of moderate to severe chronic periodontitis on dental pulp. J Indian Soc of Periodontol 16:558–561. https:// doi.org/10.4103/0972-124X.106911
- Czarnecki RT, Schilder H (1979) A histological evaluation of the human pulp in teeth with varying degrees of periodontal disease. J Endod 5:242–253. https://doi.org/10.1016/S0099-2399(79) 80018-7
- Torabinejad M, Kiger RD (1985) A histologic evaluation of dental pulp tissue of a patient with periodontal disease. Oral Surg Oral Med Oral Pathol 59:198–200. https://doi.org/10.1016/0030- 4220(85)90018-0
- Tang L, Sun TQ, Gao XJ, Zhou XD, Huang DM (2011) Tooth anatomy risk factors influencing root canal working length accessibility. Int J Oral Sci 3:135–140. https://doi.org/10.4248/IJOS1 1050
- Wu D, Shi W, Wu J, Wu Y, Liu W, Zhu Q (2011) The clinical treatment of complicated root canal therapy with the aid of a dental operating microscope. Int Dent J 61:261–266. https://doi.org/ 10.1111/j.1875-595X.2011.00070.x
- Akerblom A, Hasselgren G (1988) The prognosis for endodontic treatment of obliterated root canals. J Endod 14:565–567. https:// doi.org/10.1016/s0099-2399(88)80092-x
- Kiefner P, Connert T, ElAyouti A, Weiger R (2017) Treatment of calcified root canals in elderly people: a clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology 34:164–170. https://doi.org/10.1111/ ger.12238
- Ordinola-Zapata R, Martins JNR, Plascencia H, Versiani MA, Bramante CM (2020) The MB3 canal in maxillary molars: a micro-CT study. Clin Oral Invest 24:4109–4121. https://doi.org/ 10.1007/s00784-020-03284-7
- Yoshioka T, Kikuchi I, Fukumoto Y, Kobayashi C (2005) Suda H (2005) Detection of the second mesiobuccal canal in mesiobuccal roots of maxillary molar teeth ex vivo. Int Endod J 38:124–128. https://doi.org/10.1111/j.1365-2591.2004.00918.x
- Costa FFNP, Pacheco-Yanes J, Siqueira JF Jr, Oliveira ACS, Gazzaneo I, Amorim CA, Santos PHB, Alves FR (2019) Association between missed canals and apical periodontitis. Int Endod J 52:400–406. https://doi.org/10.1111/iej.13022
- do Carmo WD, Verner FS, Aguiar LM, Visconti MA, Ferreira MD, Lacerda MFLS, Junqueira RB (2021) Missed canals in endo- dontically treated maxillary molars of a Brazilian subpopulation: prevalence and association with periapical lesion using cone-beam computed tomography. Clin Oral Investig 25:2317–2323. https:// doi.org/10.1007/s00784-020-03554-4
- Karabucak B, Bunes A, Chehoud C, Kohli MR, Setzer F (2016) Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. J Endod 42:538–541. https://doi.org/10.1016/j. joen.2015.12.026
- Coutinho-Filho TS, Gurgel-Filho ED, Souza-Filho FJ, Silva EJNL (2012) Preliminary investigation to achieve patency of MB2 canal in maxillary molars. Braz J Oral Sci 11:373–376
- Shi X, Zhao S, Wang W, Jiang Q, Yang X (2018) Novel navigation technique for the endodontic treatment of a molar with pulp canal calcification and apical pathology. Aust Endod J 44:66–70. https:// doi.org/10.1111/aej.12207
- Jain SD, Carrico CK, Bermanis I (2020) 3-Dimensional accuracy of dynamic navigation technology in locating calcified canals. J Endod 46:839–845. https://doi.org/10.1016/j.joen.2020.03.014
