Cervical margin relocation
Machine translation
Original article is written in RU language (link to read it) .
The offset of the cervical margin (OCM) was proposed more than 15 years ago, and recently it has become increasingly popular among practicing dentists.
Learn more about the stages of working with interdental defects of molar teeth in the online course Contact Point: Effective Techniques for Restoration of the Molar Group of Teeth.
OCM is indicated when the gingival margin of a Class II cavity cannot be isolated with a rubber dam alone, as an alternative to surgical crown lengthening. The OCM technique involves creating a base from composite using a direct method with a metal matrix to raise the proximal level of the indirect adhesive restoration. Consequently, the margins can be predictably sealed using a conventional impression and/or intraoral optical scanning (IOS). Various studies describe the OCM protocol and evaluate this technique in the laboratory.
Probing Pocket Depth
The location of the subgingival margin can affect the condition of the periodontium and initially healthy tissues, determined by probing pocket depth (PPD) of 4mm or less without bleeding on probing (BOP).
Unfortunately, no clinical studies have been conducted so far to evaluate the response of periodontal tissues to indirect adhesive restorations on molars using CAD/CAM.
The literature also reports on the influence of the level of the edge of the approximal restoration on the development of secondary caries: restoration edges ending below the enamel-cement border show a significantly higher risk of failure.
The primary goal of this clinical study is to evaluate the periodontal tissue response (PTR) in single indirect adhesive restorations on molars with one interproximal edge shifted cervically; the secondary goal is to analyze the correlation between the depth of the interproximal edge and PTR. The null hypothesis adopted is that there is no statistically significant difference between edges with or without CAD/CAM regarding periodontal tissue inflammation (PTR).
Materials and Methods
As a sample, 35 restorations in 35 patients needing a single inlay on molars, installed from January to April 2016, were taken. The restorations were made in a sample of patients at the Department of Prosthodontics and Dental Materials of the University of Siena, Italy. All of them had an old composite restoration needing replacement, and carious lesions beneath it.
After a detailed explanation of the research objectives, written consents from patients were collected. Ethical approval was granted by the University of Siena, Italy.
The cleaning of the caries-affected area was performed after the installation of the first matrix strip for retraction and protection of the soft tissues, the bend of the metal matrix was carefully adapted to the curvature of the tooth to achieve the maximum possible cervical fit. In one case, the SCP procedure was conducted using G-Premio Bond for hybridization of all exposed dentin and a universal flowable composite, applied in two or three thin layers depending on the depth and size of the cavity (GC Co. Tokyo, Japan). After the final preparation, an impression was taken (Ex’lance, GC Co., Tokyo, Japan) and sent to the laboratory for the fabrication of a restoration made of pressed lithium disilicate (LS2) (LiSi Press, GC Co. Tokyo, Japan).
Temporary Restoration
A temporary restoration was made from hot polymerized plastic (PMMA). Patients were instructed to use a 0.2% chlorhexidine gluconate solution for 7 days until the ability to perform normal oral hygiene was restored and a follow-up visit was scheduled in 2 weeks for a new impression, allowing sufficient time for the soft tissues to adapt and mature after the preparation. Restorations were made in the laboratory, then tried in, edges were examined, fit and filling were checked. A rubber dam is always placed to isolate the abutment. Restorations were cemented according to the manufacturer's instructions with cement (Link Force, GC Co., Tokyo, Japan) after sandblasting, etching with phosphoric acid for 60 seconds, and covering with a primer, left for 1 minute to evaporate.
Excess cement has been carefully removed and occlusal contacts corrected if necessary. The subgingival placement of the restoration edge has been assessed, and the patient has been given oral hygiene instructions.
Restorations were placed between January 2016 and April 2016 and examined for marginal fit immediately after cementation and 12 months later.
After cementation, the position of the restoration margin relative to the gingival margin was assessed in millimeters by probing, and the linear distance to the alveolar ridge edge was measured in millimeters using intraoral radiography. Additional intraoral images were taken after 12 months.
All clinical procedures were performed using magnification ~ 3.5/4.5.
Results
SPC is accompanied by a statistically significant increase in marginal fit indicators. The gingival index GI and the plaque index PI do not statistically differ between groups. At the end of the experimental period, 53% and 31.5% of cases (group 1 and 2 respectively) showed positive marginal fit: the difference between the groups is statistically significant (p=0.10). According to radiographic analysis, the distance from the bone crest to the restoration edge is 2 mm in 13 out of 19 cases in group 1 and in 6 out of 11 cases in group 2.

Figure 1. Old indirect metal-ceramic restoration needs replacement due to secondary caries.

Figure 2. Removal of old restoration.
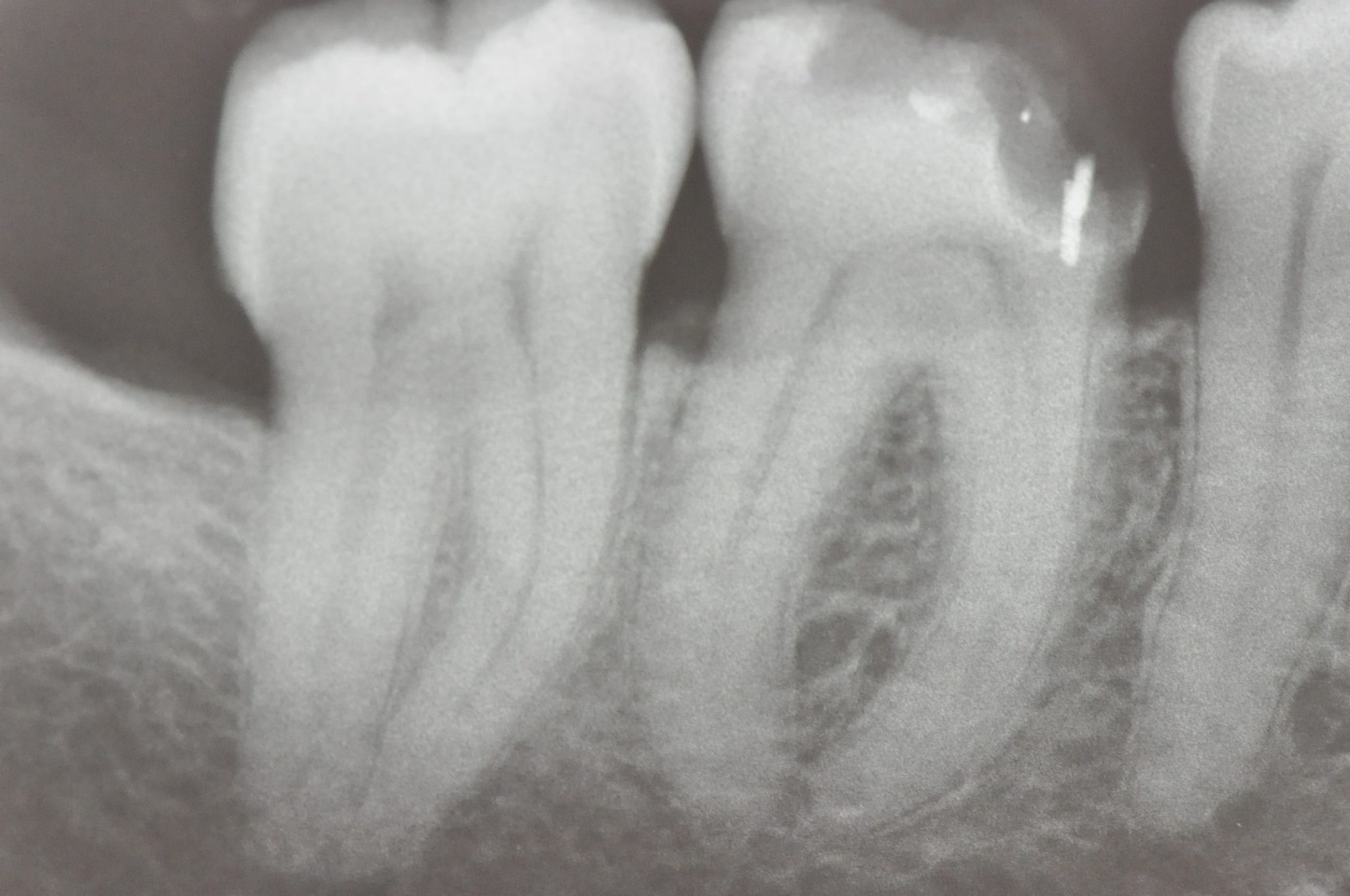
Figure 3. X-ray of the cavity.

Figure 4. Cavity after caries removal.

Figure 5. Cavity after caries removal, side view.

Figure 6. Installation of the matrix for protecting soft tissues, despite the fact that after the removal of the matrix the tissues will slightly bleed. After the placement of the rubber dam and adaptation of the metal matrix and wedge to the tooth profile, dentin sealing and displacement of the cervical edge were performed: the first layer of flowable composite has already been light-cured.

Figure 7. Completed build-up of the cavity.

Figure 8. Immediately after the build-up, the final preparation was carried out without removing the rubber dam.

Figure 9. Final preparation.
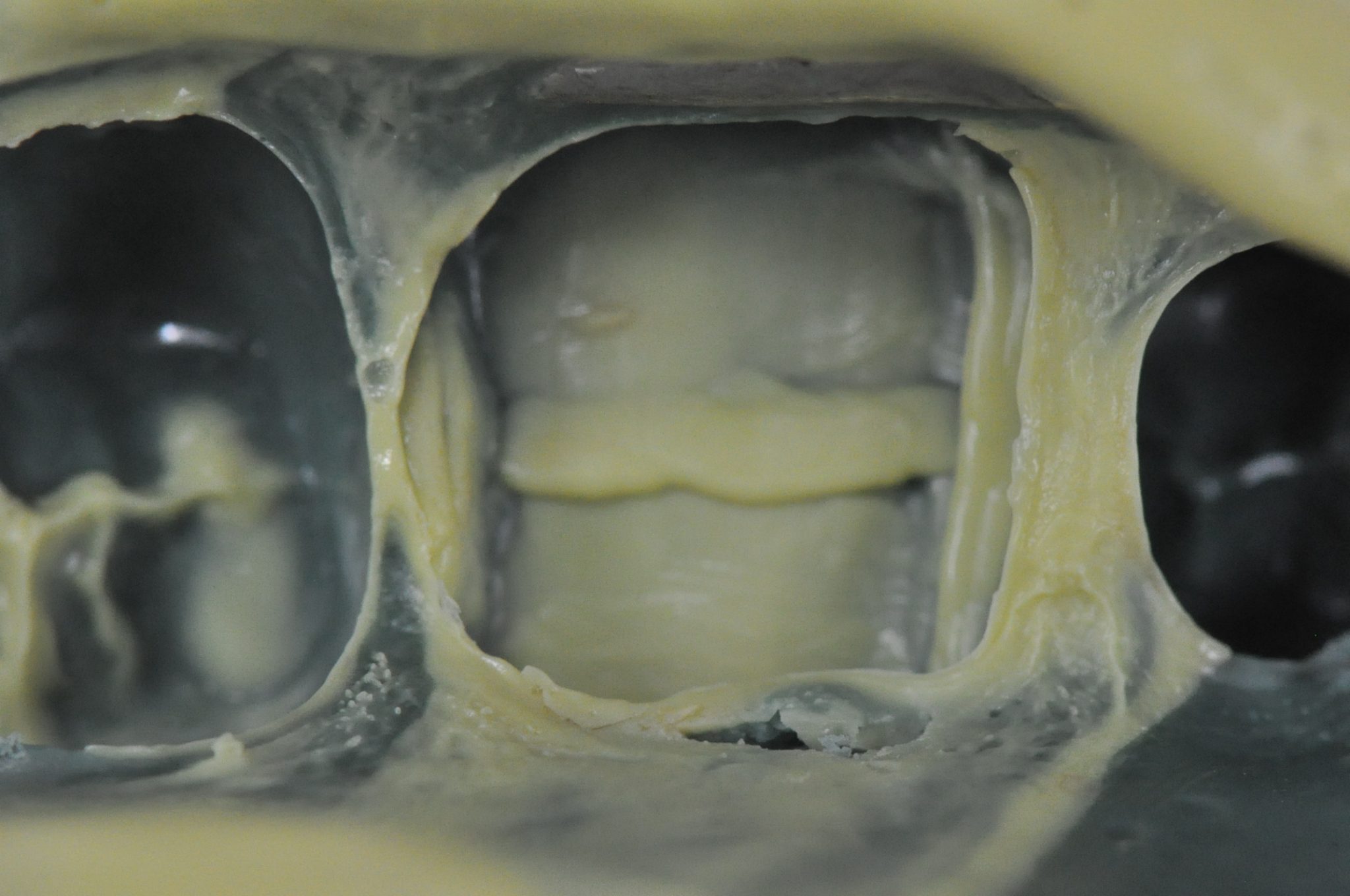
Figure 10. Taking an impression.

Figure 11. Final partial LiSi Press crown.

Figure 12. Crown after cementation using a rubber dam.

Figure 13. Check-up after 12 months: view inside the mouth.
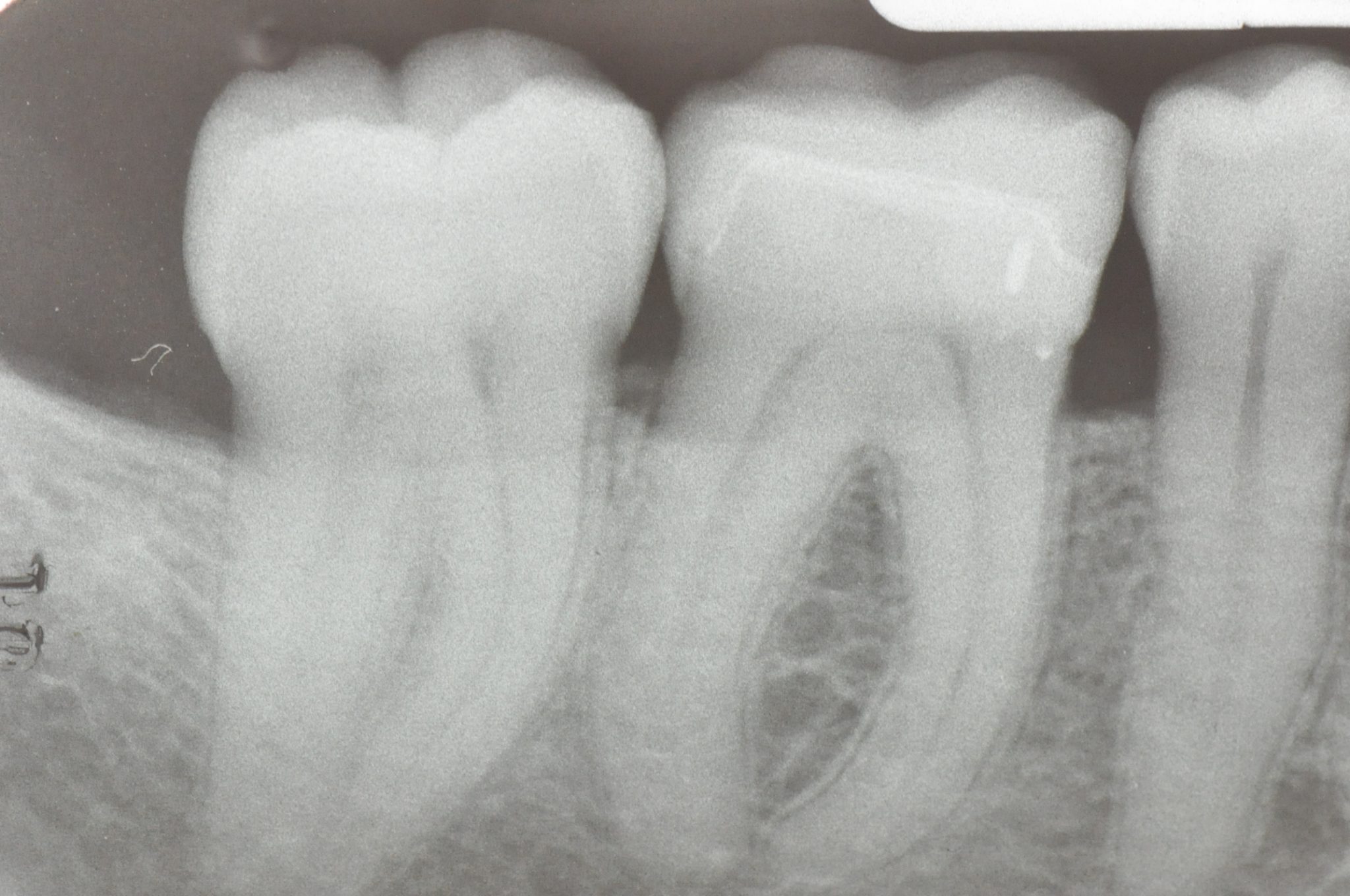
Figure 14. Check after 12 months: X-ray image.
Restoration of the Subgingival Wall
In the context of this study, a higher likelihood of manifestation of Cervical Margin Relocation (CMR) can be expected when using the CMR technique compared to conventional restoration of the subgingival wall. CMR is sensitive to the execution technique, especially in the case of a deep subgingival margin and conducting adhesive preparation below the enamel-cement boundary.
Description of methods and recommendations on the technique of raising the deep subgingival margin in the webinar Rationale for the technique of raising the deep subgingival margin.
Bibliography
Dietschi D, Spreafico R. Adhesive metal-free restorations: current concepts for the esthetic treatment of posterior teeth. Quintessence 2 (1997) 60-77.
Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of toothcolored posterior restorations. Pract Periodontics Aesthet Dent 10 (1998) 47-54.
Magne P, Spreafico R. Deep Margin Elevation: A Paradigm Shift. Am J Esthet Dent 2(2012) 86-96.
Rocca GT, Kreiji I. Bonded indirect restorations for posterior teeth: from cavity preparation to provisionalization. Quintessence Int 38 (2007) 371-379.
Rocca GT, Rizcalla N, Krejci I, Dietschi D. Concepts and evidence-based procedures for bonded inlays and onlays. Part II. Guidelines from cavity preparation to final restoration. Int J Esthet Dent 3 (2015) 370-392.
Spreafico RC, Krejci I, Dietschi D. Clinical performance and marginal adaptation of class II direct and semidirect composite restorations over 3.5 years in vivo. J Dent 33 (2005) 499-507.
Veneziani M. Adhesive restorations in the posterior area with subgingival cervical margins: new classification and differentiated treatment approach. Eur J Esthet Dent 5 (2010) 50-76.
http://styleitaliano.org/
