Separation Membranes in the Practice of Surgical Periodontology
Machine translation
Original article is written in RU language (link to read it) .
In the arsenal of specialists engaged in surgical periodontology today, there are several dozen different surgical techniques, most of which have only minor differences from each other. To achieve effective treatment results, it is sufficient to master at least a few of them, which have proven themselves well in clinical use, and the long-term results are quite guaranteed, which is most valuable for periodontal surgeons just starting their practice.
About the advantages of using membranes for guided tissue regeneration in the webinar on Regenerative Surgery of Periodontal Tissues in Intrabony Defects and Furcation Defects.
The effectiveness of surgical interventions is determined by the indications for their use, which depends on the form of the disease, the depth of the lesion, the condition of the gingival margin, disturbances in the furcation area, resorption of the alveolar ridge, the degree of root exposure, and the overall somatic health of the patient.
Directed regeneration using a barrier membrane
This manipulation is performed in the area of several teeth as more extensive intervention provokes a deterioration in blood supply.
Surgical technique
Anesthetizing the surgical area.
Next, the interdental papilla is incised and small vertical incisions are made, after which the detachment of the mucoperiosteal flap begins.
The next stage involves cleaning the tooth surfaces from subgingival deposits, which can be done in various ways: chemically and mechanically. The chemical method involves applying an 18% solution of citric acid for one minute or 0.1% sodium hypochlorite.
The effect of such an application on the root surfaces is sufficient for the complete removal of microbial toxins and protein conglomerates, which accumulate there during the formation of periodontal pockets or against the background of gum recession. Regarding gum recession, if it has occurred relatively long ago, the dentinal tubules in this area will be densely sealed with protein and salt deposits, and the root surface appears smooth, polished. If the root surface is left smooth, one cannot count on a reliable connection with the mucoperiosteal flap surface, and some time after the operation, gum recession will begin.

Figure 1. Gum recession.
Under the influence of citric acid, the openings of the dentinal tubules are exposed. In the future, regeneration processes will be initiated in them thanks to the formation of cement "nails", as well as the exposure of collagen fibers. A similar, but less pronounced effect is observed with the influence of tetracycline hydrochloride, which is released in the form of a moistened powder, applied to the affected area for several minutes. Absorbing into the structures of collagen and tooth tissue, the drug has a local antimicrobial effect.
For the treatment of the root surface, fibronectin is also used, which improves adhesion and fixation of the flap, stimulates the proliferation and growth of fibrocytes, ensuring the preservation of the formed flap. This solution is applied in the form of applications, but only after the preliminary influence of citric acid or tetracycline. It is important to consider the weak demineralizing ability of this drug. Subsequently, an analysis of the defect, its configuration, and size is carried out, based on these parameters a membrane is selected. The latter must ensure the coverage of the defect area by several millimeters around the entire perimeter.
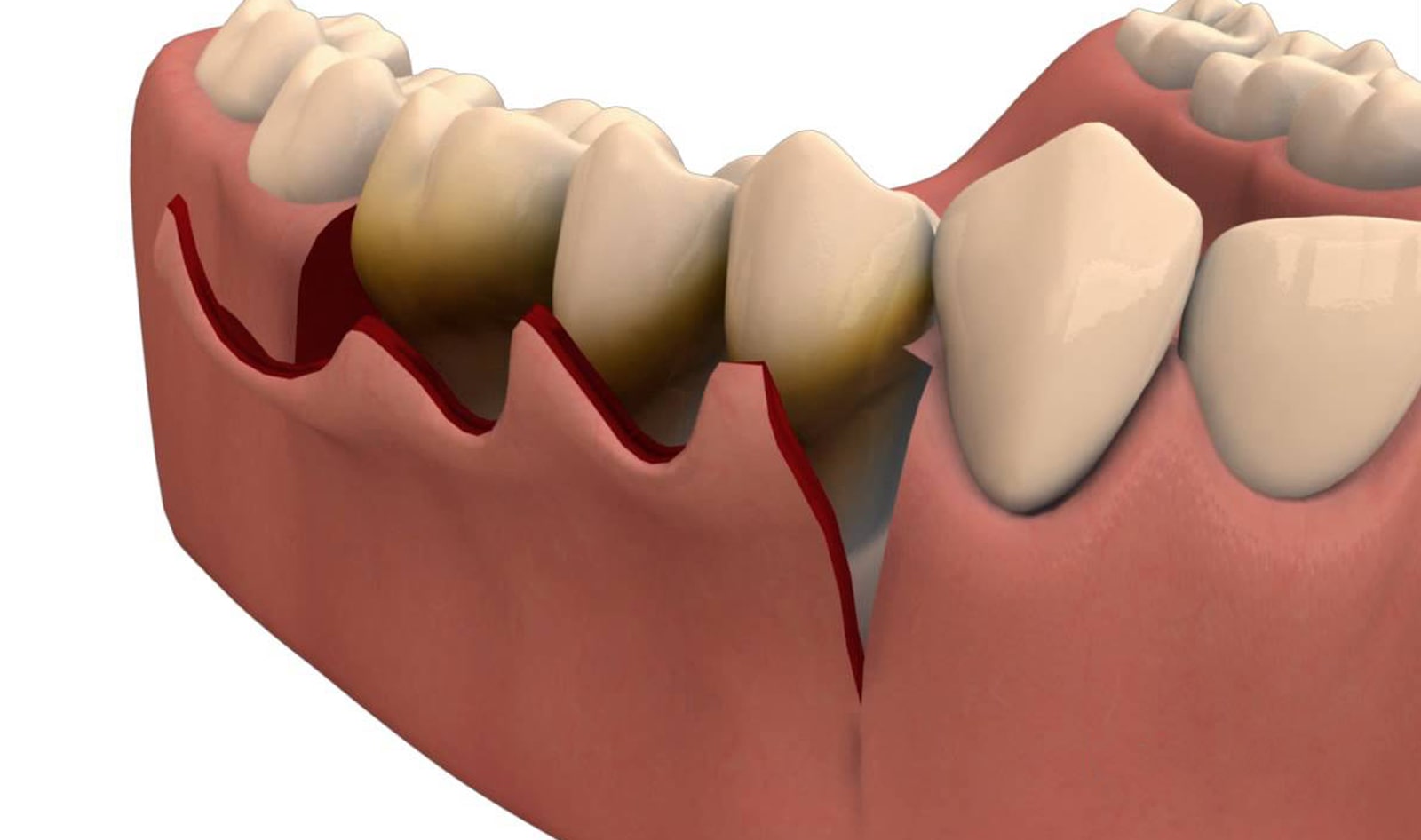
Figure 2. Detachment of the mucoperiosteal flap.
There is also a technique of osteotomy of the cortical plate in the area directly beneath the membrane. In this case, the fixation of the membrane is achieved using a special material in the area of the tooth neck, not reaching the level of the anticipated new periodontal attachment (two millimeters above the enamel-cementum border).
Next, the flap is placed back and secured in the interdental spaces with sutures. Two months after the application of the non-resorbable membrane, anesthesia is reapplied, and the gum is incised in the interdental spaces at the sites of the previous cuts. The mucoperiosteal flap is slightly shifted, the sutures securing the membrane are cut. The membrane is removed with a sharp movement, then the flap is moved and placed back, secured with catgut sutures.
Membranes made of nickel-titanium alloy have the ability to integrate with surrounding tissues, eliminating the need for repeated surgical procedures to remove the membrane. The technique of using a tissue implant made of nickel-titanium does not require the use of special devices and tools, which is a fundamental factor for recommending this protocol to optimize the mechanisms of reparative bone tissue regeneration in periodontal surgery in various clinical cases.
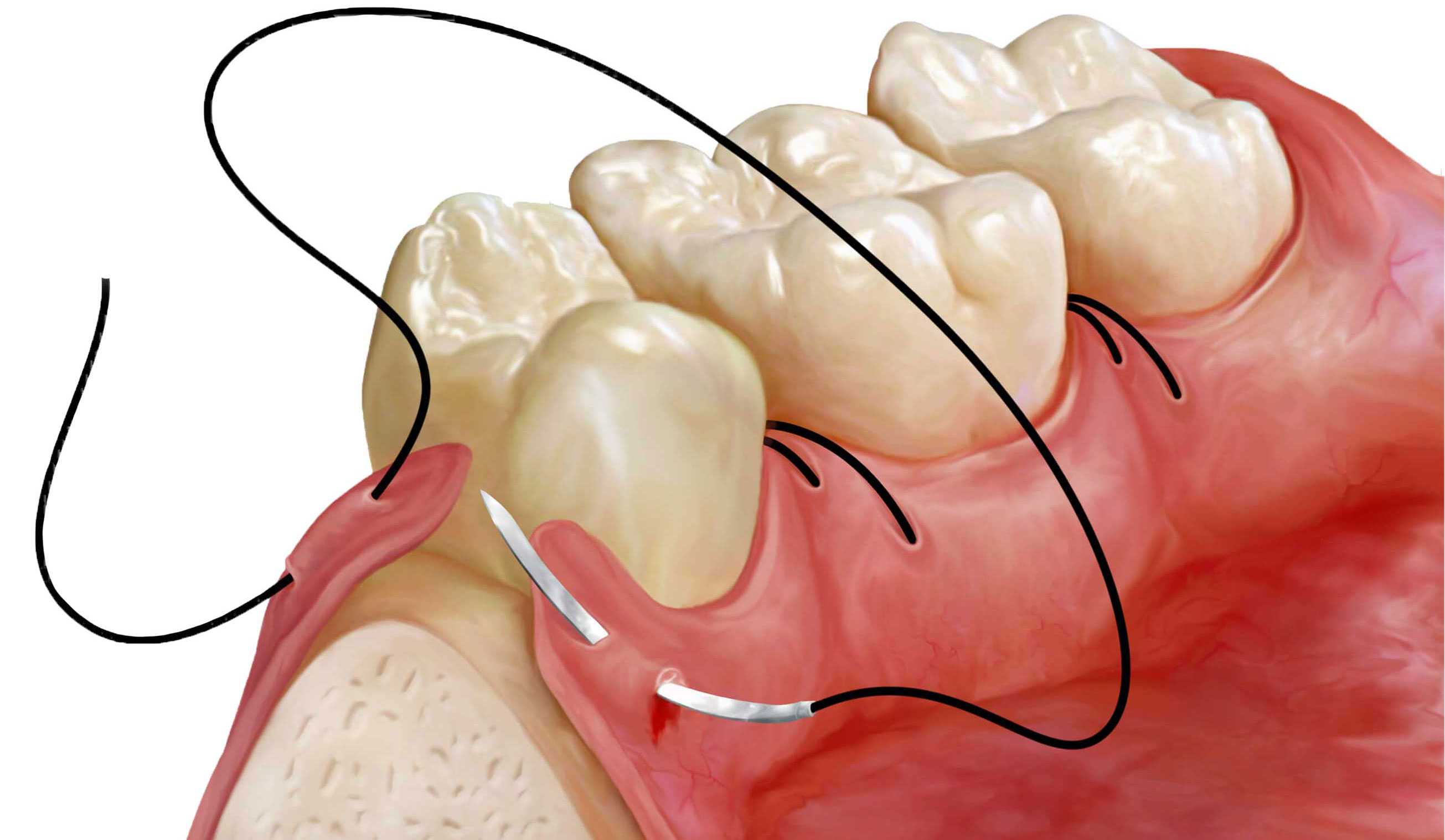
Figure 3. Suturing.
The combined use of bone grafts and collagen membranes in more than 90% of clinical situations leads to the formation of connective tissue structures, as well as promotes the filling of bone defects by more than half.
Bone Grafts
According to the classification by Bernard, bone grafts are divided into the following classes:
- osteoconductive;
- osteoinductive.
Osteoconductive grafts provide the creation of a framework resembling a matrix in which new bone elements are formed. Among the representatives of this class are dried or frozen:
- hydroxyapatite ceramic compositions;
- bone allografts.
Osteoinductive grafts promote the release of factors that stimulate regeneration processes, without forming any kind of framework. Representatives of this group include decalcified and demineralized bone allografts.
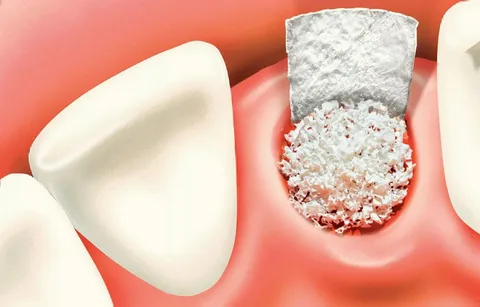
Figure 4. Application of bone graft.
Fibrine Riche Plaguettes
Today, the most promising direction is to increase the long-term effectiveness of regeneration through the use of agents that activate the regeneration of the periodontal ligament and bone. Among these drugs, the platelet growth factor FRP is of greatest interest, which is a platelet mass containing a large amount of fibrin.
Growth factors are natural peptides, similar to hormones, but their action is exclusively local; they are not found in free form in the blood. Growth factors regulate cell growth, control the performance of their functions, have the ability to evolve and transform into cells of connective tissue, ligaments, bones, epithelium.
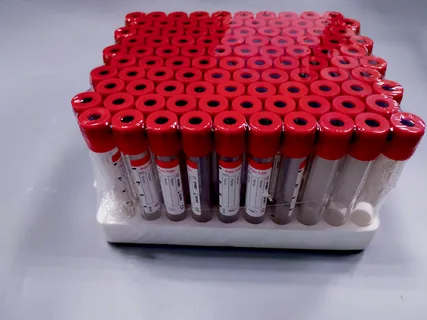
Figure 5. Obtaining platelets with high fibrin content.
To obtain a platelet mass with high fibrin content, an FRP centrifuge is used, and a set of special tubes is also required. Just before the surgical intervention, blood is drawn into the tubes, then the blood undergoes a centrifugation cycle for 12 minutes at a speed of 2600 revolutions per minute. As a result of centrifugation, the following fractions are formed in the tubes:
- red blood cells settle in the lowest layer;
- the upper layer remains plasma, which contains a minimal amount of platelets;
- in the middle, there is a clot, which contains the main mass of platelets, it is carefully extracted with tweezers and transferred to a sterile surface.
The advantage of this technique is that the blood is not exposed to anticoagulants or strong vibrations, which are crucial conditions for obtaining platelets with a maximally high fibrin content at the output. The blood does not undergo any other manipulations, and therefore, there are no obstacles for its use. The introduction of these factors into a membrane-limited area along with bone grafts significantly stimulates regeneration.
After the surgical intervention, patients are put on clinical follow-up, which includes general observation and control of the local status:
- condition of the mucosa in the area of the gingival margin;
- periodontal index control;
- preservation or elimination of periodontal pockets;
- presence of tooth mobility;
- performance of control radiography;
- assessment of capillary resistance;
- conducting reoparodontography and osteometry;
- assessment of general and local nonspecific protection.
All these activities allow us to make a forecast and determine the dynamics of the process. The most important criterion is the condition of the periodontal tissues.
About the biological principles of guided bone regeneration in the webinar Resorbable membranes in guided bone regeneration.
