Vital pulp treatment for traumatized permanent teeth: A systematic review
ABSTRACT
Background: Traumatic dental injuries involving the pulp are quite common and there is a need to evaluate the quality of evidence on the success of vital pulp treatment (VPT) interventions in traumatised permanent teeth.
Objectives: The aim of this systematic review was to assess the success of VPT in the management of traumatised human vital permanent teeth diagnosed with complicated crown or crown-root fractures.
Methods: An electronic search of the following databases: Web of Science, Scopus, PubMed, MEDLINE, EMBASE, LILACS, Clinical Trial Registries and the grey literature was performed until 25th/8/2021. Controlled clinical trials, cohort studies, case-control studies, case series with at least five cases and a minimum of 12-months follow-up were included. Non-English language literature was excluded. Two independent assessors performed study selection, data extraction and quality assessment using the National Institutes of Health’s quality assessment tool. Disagreements were resolved through consensus/with a third assessor.
Results: A total of 14-studies (2-controlled clinical trials, 1-case-control, and 11-case series)publishedbetween1978–2020,witha totalof 1081permanentteethandanage range between 6–42 years-old were included. Bias analysis ranged considerably from ‘good’ to ‘poor’. Meta-analysis was not performed due to data heterogeneity, unclear reporting, and limited number of controlled clinical studies. Partial pulpotomy was the main reported clinical procedure with an overallsuccessrate between 82.9–100%.Complete pulpotomy and direct pulp capping were associated with lower success rates of 79.4–85.7% and 19.5%, respectively. Calcium hydroxide was the main pulp capping material with favourable clinical and radiographic success (79.4–100%). Biodentine®, mineral trioxide aggregate and IRoot® BP were also associated with a high clinical and radiographic success, 80–91%, 80–100%, and 90–100%, respectively, albeit in fewer studies.
Discussion: Although a high success rate has been reported when using VPT in managing pulpally involved traumatised teeth, the results of this systematic review clearly highlighted a paucity and low quality of the available evidence.
Conclusions: Overall high success of VPT in the management of traumatised vital permanent teeth were reported, although based on limited evidence of well- conducted clinical studies.
INTRODUCTION
Traumatic dental injuries (TDIs) account for approximately 5% of all injuries, with high prevalence in children and young adults (Andersson, 2013). In the permanent dentition, crown fractures are more prevalent than luxation injuries, of which, complicated crown and crown- root fractures are commonly seen (DiAngelis et al., 2016).
Several complicationssuch as tooth discolouration, mobility, malocclusion, pulp necrosis and eventually tooth loss might occur following TDIs. Hence, prompt and accurate management of TDIs improves the overall prognosis and reduces the risk of future complications (Krastl, Weiger, Ebeleseder, et al., 2021).
Loss of pulpal vitality, especially in immature teeth, can significantly reduce the long-term prognosis of injured teeth (Nazzal & Duggal, 2017). Furthermore, shortcomingsin the initial management of TDIs can potentially lead to a lifelong treatment cycle with an inherent increase in treatment costs (Andersson, 2013). Therefore, preservation of pulp vitality through the use of available vital pulp treatment (VPT) interventions is a key component in the management of traumatized teeth (Cohenca et al., 2013; da Rosa, Piva, et al., 2018). There are additional details about several damaged tooth treatment that you can obtain in our course "Saving hopeless teeth: surgical and conservative protocols".
Clinically, various VPT interventions are well documented and aim to maintain the vitality of pulp tissue that has been previously compromised (Kodonas et al., 2021).
Direct pulp capping involves the placement of a protective pulp capping material directly over the exposure site and is mainly indicated in a recent and pinpoint-sized exposed vital pulp (Duncan et al., 2019). Partial (Cvek) pulpotomy, involves partial removal of the coronal pulp, achieving haemostasis followed by placement of a pulp capping material. Furthermore, full (complete) pulpotomy involves removal of the entire coronal pulp to the level of pulp stumps, achieving haemostasisfollowed by placement of a pulp capping material (Duncan et al., 2019; Krastl, Weiger, Ebeleseder, et al., 2021).
Currently, available systematic reviews and meta-analyses assessing the success of VPT in permanent teeth have mainly focussed on carious exposed pulp tissue (Aguilar & Linsuwanont, 2011; Cushley et al., 2021; Munir et al., 2020). More recently, a systematic review assessing VPT in permanent teeth due to multifactorial pulpal diagnosis (carious and traumatic exposures) has been performed (Sabeti et al., 2021). However, to the authors’ knowledge, no previous systematic reviews assessing VPT in relation to traumatized exposed pulp tissue have been reported. In contrast to microbial-driven dental caries exposures, which subjects the pulp to a low-grade chronic injury, pulp exposure as a result of TDIs generally involves a considerably lower microbial contamination and shorter exposure time. Consequently, pulpal exposures, as a result of dental trauma, are likely to have a better chance of healing (Bjørndal et al., 2010; Cohenca et al., 2013; da Rosa, Piva, et al., 2018). Therefore, the aim of this systematic review was to assess the success of VPT interventions in the management of traumatized human vital permanent teeth diagnosed with complicated crown or crown-root fractures.
MATERIALS AND METHODS
Protocol registration and review question
This systematic review was registered with the international prospective register of systematic reviews (PROSPERO; CRD42020205213) and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009). The research question was formulated using the PICOS framework: In traumatized human vital permanent (immature/mature) teeth diagnosed with complicated crown fracture or crown-root fracture (P), with or without concomitant injuries, do VPT interventions or medicaments (I & C) lead to clinical and radiographic success (O) as reported in randomized, non-randomized and quasirandomized clinical trials, cohort studies, case-control studies, case series of at least 5 cases and a minimum of 12-months follow-up period (S)? Detailed inclusion and exclusion criteria are listed in Table 1.
TABLE 1 Inclusion and exclusion criteria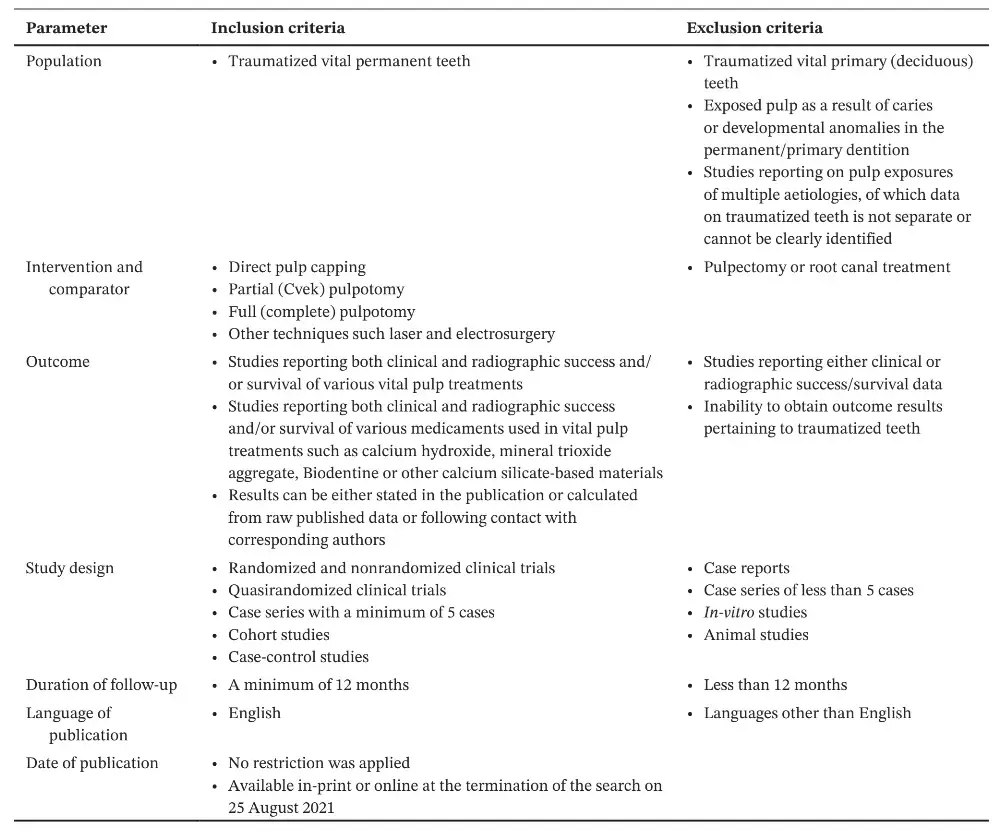
Information sources and search strategy
To identify all studies related to our research question, several databases were searched systematically. Clarivate Analytics’ Web of Science [1980–2021], Scopus [1960–2021], PubMed [1964–2021], MEDLINE [1946–2021], EMBASE [1947–2021] and Latin American and Caribbean Health Sciences Library [LILACS; 1982–2021]. Clinical Trial Registries [Cochrane Central Register for Controlled Trials (CENTRAL) ‘https://www.cochranelibrary.com/central’ and ClinicalTrials.gov ‘https://clinicaltrials.gov’) were electronically searched and only published data were included. Furthermore, to identify unpublished manuscripts, conference papers, research reports and other grey literature through available digitalrepositories; OpenGrey (Europe), ProQuest Dissertations and Theses and Google Scholar (first 50 returns) were searched. All database searches were performed by one author (A.S.) with the assistance of a librarian. Controlled indexing vocabulary (e.g. Medical Subject Headings – MeSH) and free-text or synonymous terms, were used in all search engines while following the syntax rules in each database.
All combinations using (OR, AND, NOT) were used (if applicable) for refinement of the search results. The detailed electronic search strategy is presented in Table S1. Furthermore, five endodontic and dental trauma specialized key journals namely: Australian Endodontic Journal, Dental Traumatology, International Endodontic Journal, Journal of Endodontics, and Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontology, were individually searched through their respective journal's website. The reference lists of all identified eligible studies and other published systematic reviews were hand-searched in order to identify further eligible studies. No time (i.e. year of publication) restrictions were applied and only English language literature was included. The initial search was conducted on 5th October 2020 and an updated search up to 25th August 2021 was performed.
Study selection process
Following duplicates removal, the titles and abstracts of all identified manuscripts were screened independently in this stage by four trained and calibrated assessors (M.M, A.S, H.N, & H.J.T.) against a stipulated inclusion criterion using Rayyan application (https://rayyan.qcri.org/welcome) (Ouzzani et al., 2016). Full-text assessment of potential studies was independently performed by two of the assessors (M.M. and A.S.). Discrepancies and disagreements on study selection were resolved through consensus or discussion with two other assessors (H.N. and H.J.T.).
Data extraction
Data were entered into a standardized pretested electronic data collection form (modified checklist form provided in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0.). Data extraction of all the included studies was performed independently by two calibrated assessors (M.M. and A.S.) who were not blinded to the identity of the authors of the studies, their institutions or the results of their research. All extracted data were stored in a predeveloped Excel spreadsheet created using Microsoft Office software (Microsoft Inc.). If stated, the sources of funding, trial registration and publishing of the trial's protocol were also recorded.
This information was used to aid the assessment of heterogeneity and the external validity of included studies. In case of missing data, attempts were made to contact the corresponding author. Disagreements were resolved through consensus or by discussing with two other asses- sors (H.N. and H.J.T.).
Quality assessment of included studies
The risk of bias in the included studies was performed by two independent and calibrated assessors (A.S. and M.M.) using the National Institutes of Health's (NIH) quality assessment tool. Developed in 2013 by National Heart, Lung, and Blood Institute, the NIH quality assessment tools enable the evaluation of various study designs via a set of tailored criteria that aim to assist the reviewer on key concepts focussing on a study’s internal validity (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). The comprehensive evaluation criteria cover various aspects of study design and reporting, such as sample selection, comparability of the groups, dropout rates and outcome assessment. The overall quality rating of each study is classified as either ‘good’, ‘fair’ or ‘poor’ depending on the overall score percentage of 100–80%, 79–60 and <60%, respectively (George et al., 2019). The Scottish Intercollegiate Guidelines Network (SIGN) Grading System (SIGN 50, 2019) was also applied to grade the level of evidence (LOE). Disagreements were resolved by discussing with two other assessors (H.N. and H.J.T.). In case of clarification, the corresponding author was contacted by e-mail. A record of all decisions on study identification was kept.
RESULTS
Literature search and characteristics of the included studies
The literature search retrieved a total of 5255 records, of which 1298 duplicate records were removed and 3904 were excluded following initial title and abstract screening. A total of 53 studies underwent full-text assessment, of which 39 studies were excluded (Table S2). Consequently, a total of 14 studies were found to be eligible for inclusion in this systematic review (Figure 1). Upon further assessment, two studies were found to belong to the same study cohort in which the authors reported their results at different time points. However, as the sample size reduced from 63 to 40 participants in the second report, both studies are presented individually (Fuks et al., 1987, 1993).
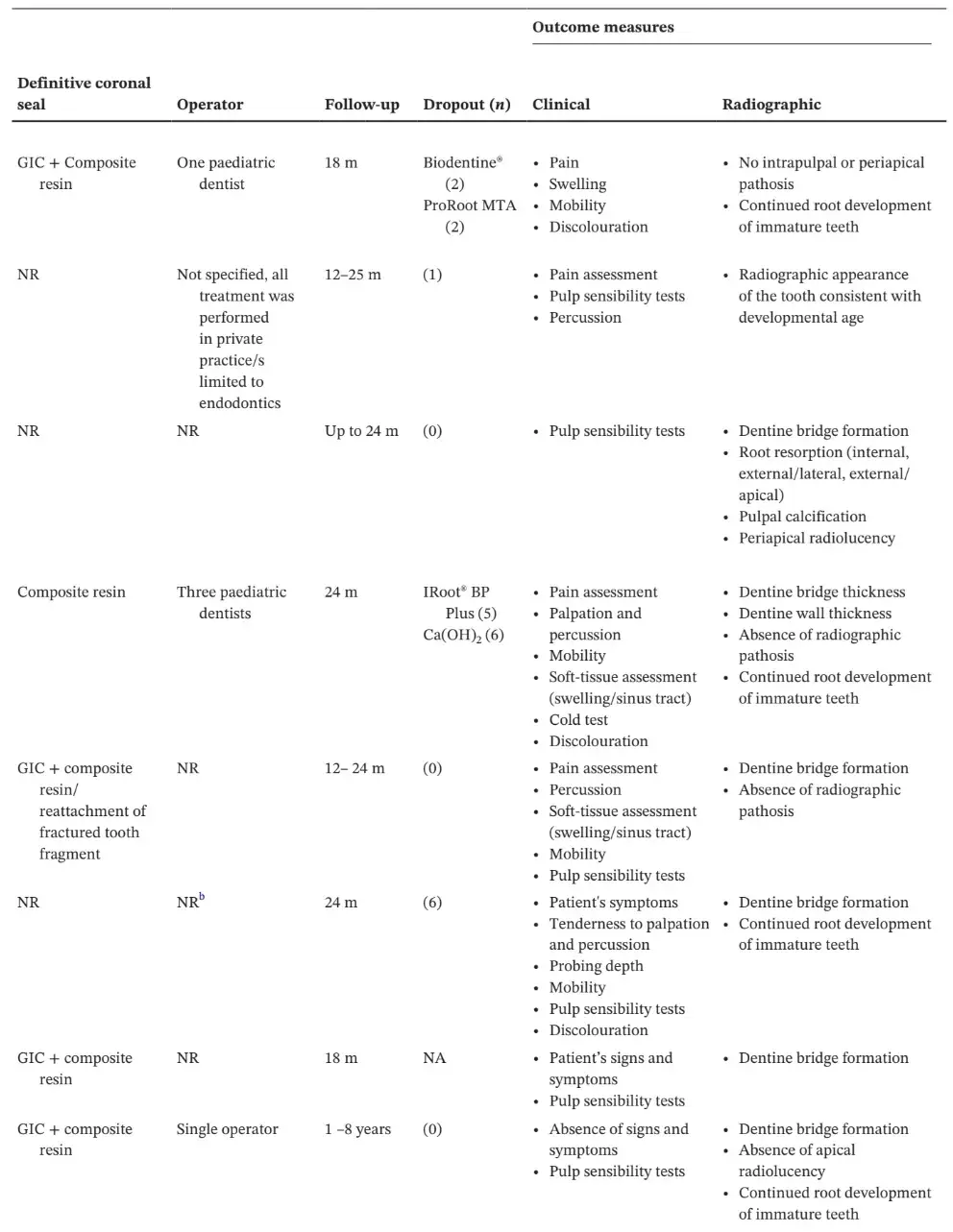
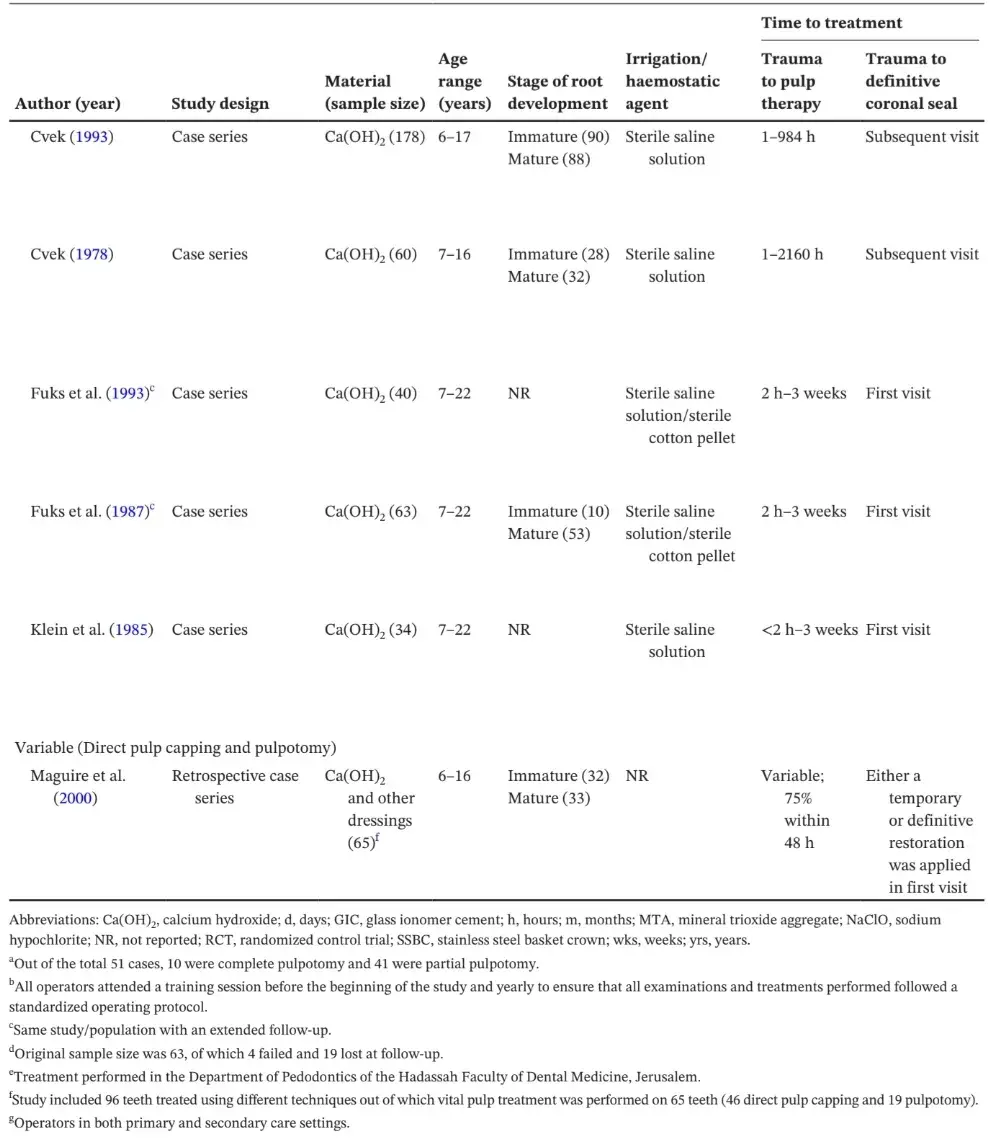
The characteristics of the included studies are described in Table 2, where the following parameters have been summarized: Study design, pulp capping material, participants’ age, stage of root development, irrigation/ haemostatic agent, time to treatment; including trauma to pulp therapy and trauma to definitive coronal seal, definitive coronal seal, operator, follow-up period, dropout rates and both clinical and radiographic outcomes. The majority of studies were conducted in a university hospital setting, with the exception of two studies; one conducted in a governmental setting (de Blanco, 1996) and one in a private practice setting (Witherspoon et al., 2006).
The age range of the participants within the included studies varied from 6 to 42-years-old and involved a total of 1081 permanent teeth. The majority of the included studies specified the type of injured tooth/teeth, of which maxillary central incisors were the most common. Teeth with concomitant trauma were included in five studies (Fuks et al., 1987, 1993; Haikal et al., 2020; Klein et al., 1985; Maguire et al., 2000), whereas excluded in one study (Rao et al., 2020). The remaining seven studies did not report on the presence or absence of concomitant injury (Abuelniel et al., 2020; de Blanco, 1996; Cvek, 1978, 1993; Gelbier & Winter, 1988; Koyuncuoglu et al., 2013; Witherspoon et al., 2006; Yang et al., 2020).
Radiographic outcomes in the majority of studies were assessed with periapical radiographs, with only two studies performing additional root quantification measurements utilizing ImageJ software (Abuelniel et al., 2020; Yang et al., 2020). With regard to the definitive coronal seal, glass ionomer cement and/or composite resin were the most commonly reported material used either placed at the first visit or subsequent visits. Stainless steel crowns were also utilized in cases of deep fractures; however, these were restricted mainly to studies performed in late 80s and early 90s (Fuks et al., 1987, 1993; Klein et al., 1985).
Only two studies declared sources of funding: A retrospective case-control conducted in China received grant support from the National Natural Science Foundation of China (Rao et al., 2020), while a prospective case series conducted in Canada acknowledged a pharmaceutical and medical device company (Septodont) for donating Biodentine® for their research (Haikal et al., 2020).
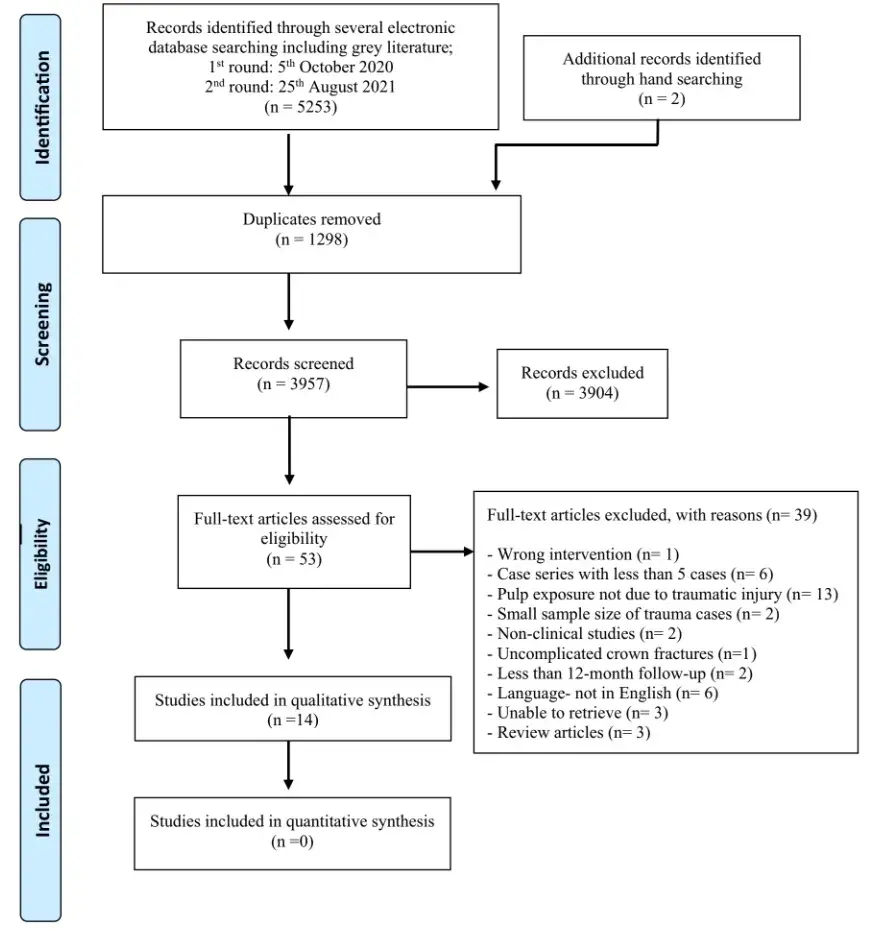 FIGURE 1 PRISMA flow diagram of the study search strategy and identification of relevant studies
FIGURE 1 PRISMA flow diagram of the study search strategy and identification of relevant studies
TABLE 2 Study characteristics and outcome measures of complicated crown fracture studies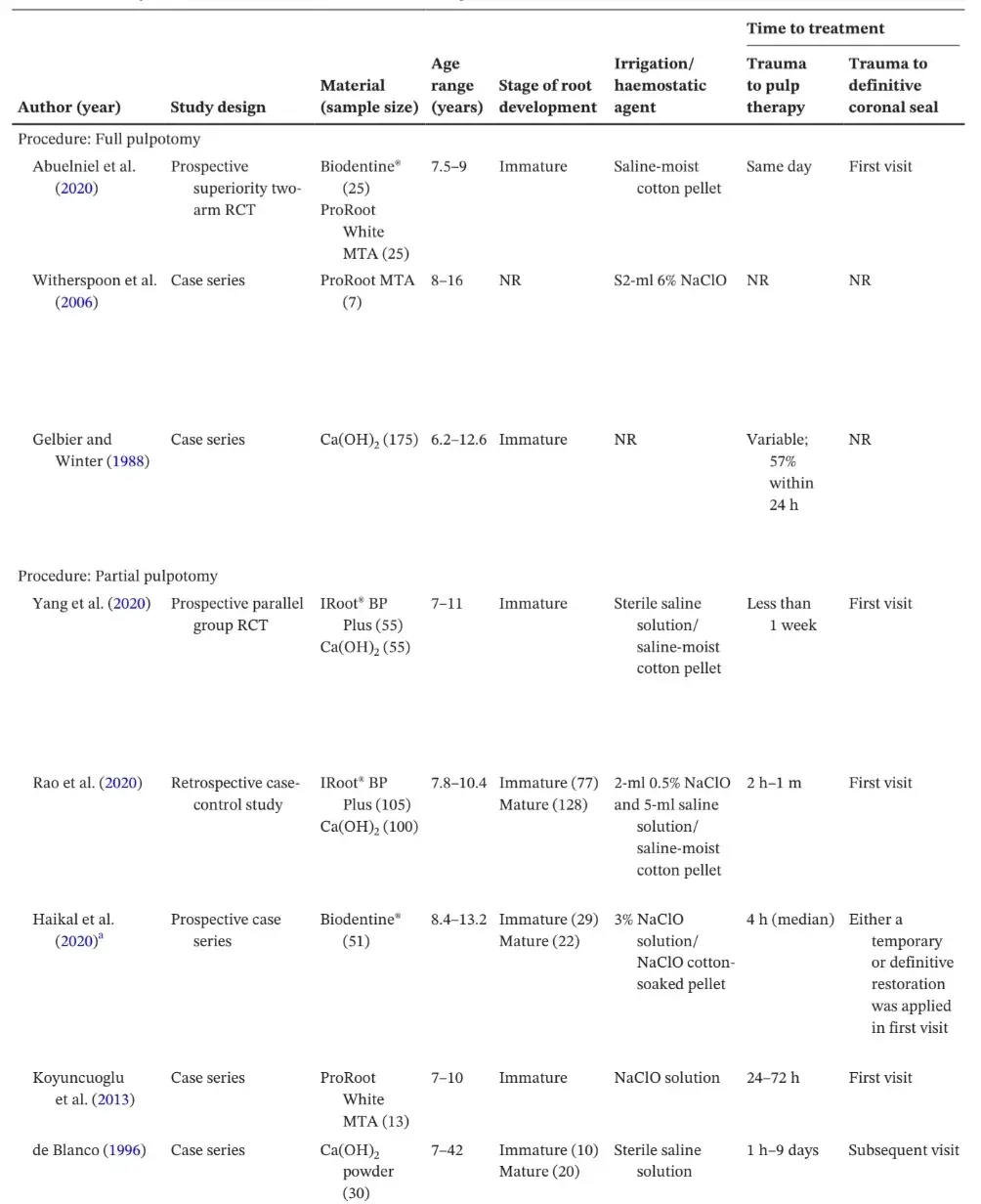
Clinical and radiographic success
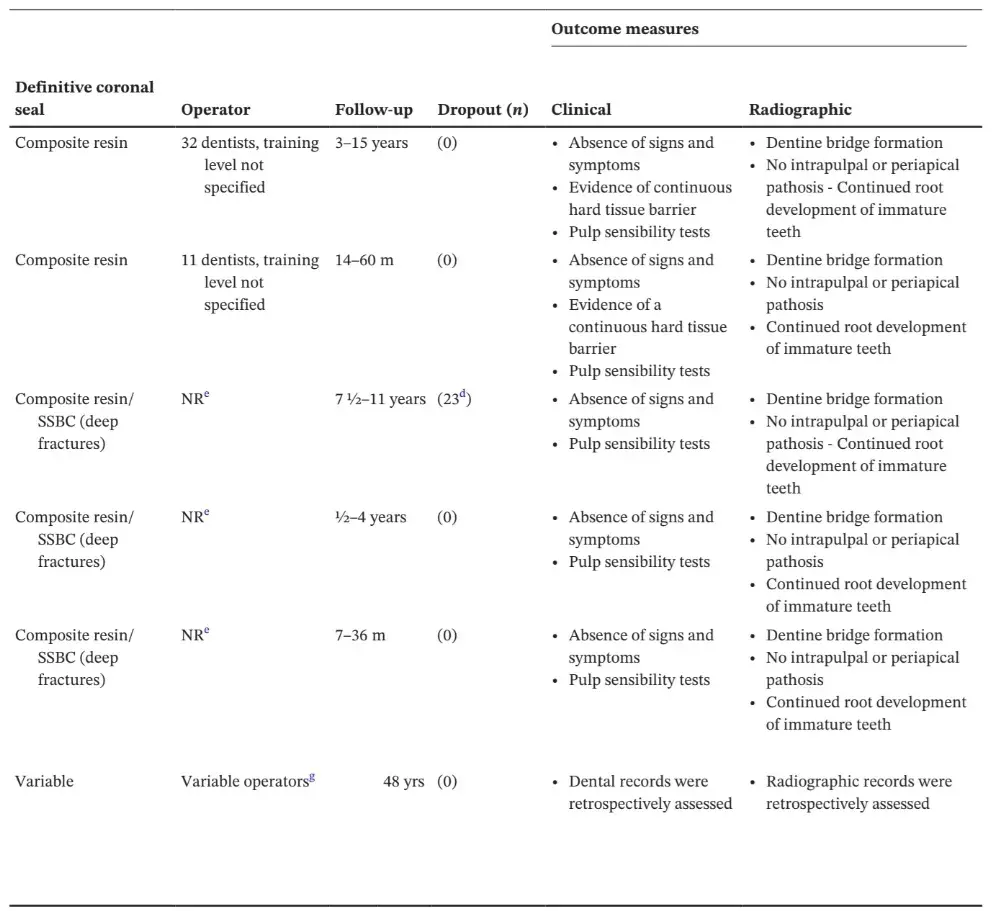
The criteria for clinical and radiographic outcomes defining success are listed in Table 2. Clinical parameters such as pain assessment, pulp sensibility tests, soft tissue assessment, mobility, discolouration and radiographic parameters, e.g. dentine bridge formation, absence of radiographic pathosis, continuation of root development in immature teeth, are reported in the majority of included studies. However, detailed quantification measurement of the continuation in root development of immature teeth was only assessed in 14.3% (n = 2) of included studies (Abuelniel et al., 2020; Yang et al., 2020). In terms of coronal discolouration, only two studies assessed this outcome.
In a randomized controlled trial (RCT), Abuelniel and colleagues reported a significantly higher discolouration following full pulpotomy in the MTA group (88%) compared with the Biodentine® group (0%) (Abuelniel et al., 2020). On the contrary, in a case series design of 51 teeth, discolouration was observed in 17% of cases following Biodentine® partial pulpotomy (Haikal et al., 2020).
Detailed outcomes of all included studies are listed in Table 3. Overall, a high success rate of VPT interventions in the treatment of traumatized vital permanent teeth across the included studies was shown. Partial pulpotomy was the main reported clinical procedure accounting for approximately 71.4% (n = 10) of the studies, with an overall success rate between 82.9–100%. On the otherhand, three studies reported full pulpotomy, and only one study reported direct pulp capping, with lower success rates of 79.4–85.7% and 19.5%, respectively. Calcium hydroxide was the most commonly used pulp capping material, with favourable clinical and radiographic success rates of between 79.4–100%. Other pulp capping materials such as Biodentine®, MTA and IRoot® BP were also associated with high clinical and radiographic success, 80–91%, 80–100% and 90–100%, respectively, albeit in fewer studies.
TABLE 3 Reported outcomes of included studies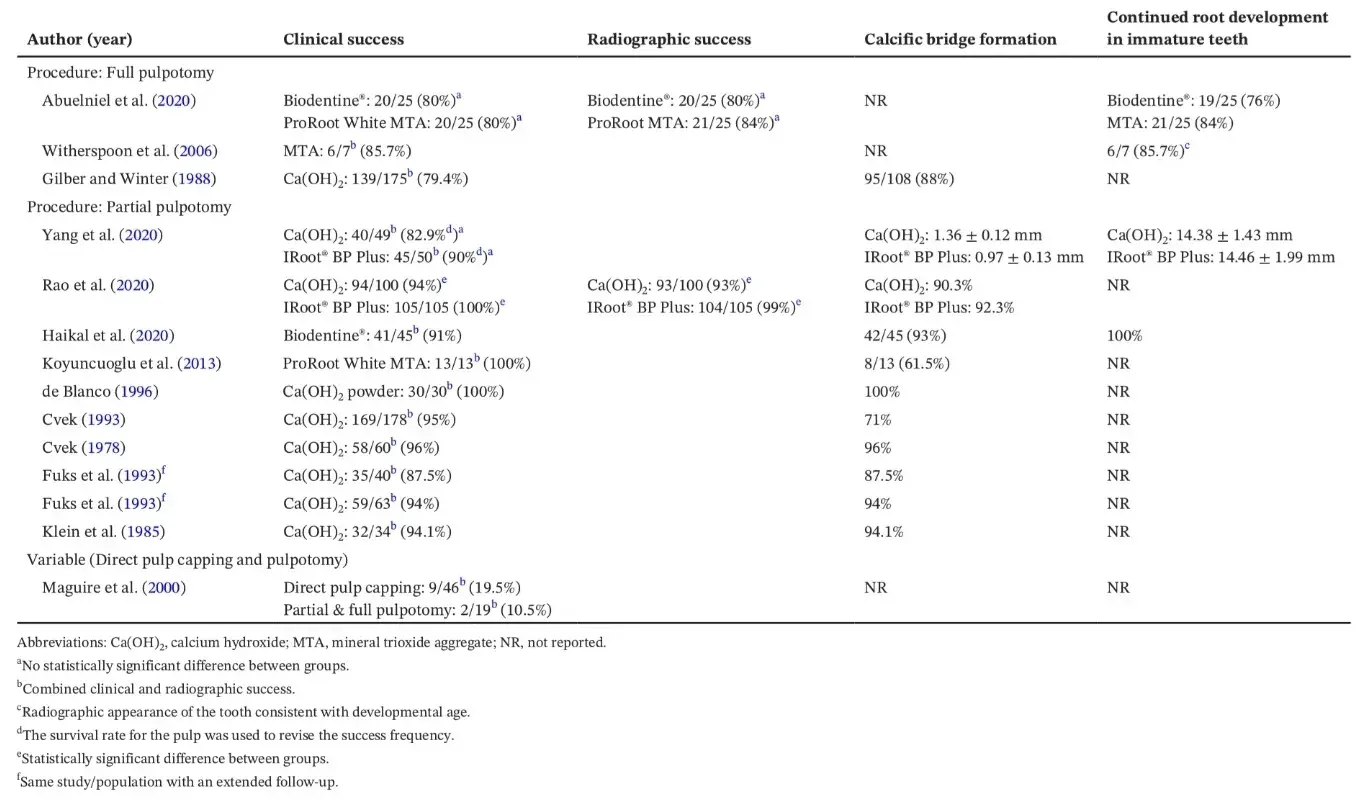
Quality of included studies
Detailed assessment of the risk of bias utilizing the NIH quality assessment tool was performed (Table S3). The quality of the evidence of the included RCTs was scored as ‘good’ (Abuelniel et al., 2020) and ‘fair’ (Yang et al., 2020), with overall LOE = 1+. The quality assessment for the included retrospective case-control study was also scored as ‘fair’ (LOE = 2+). The lack of a sample size justification and/or power description was deemed to negatively affect the overall study quality. Out of the 11 case series, 8 were scored as ‘good’ (LOE = 3), (Cvek, 1978, 1993; Fuks et al., 1987, 1993; Haikal et al., 2020; Klein et al., 1985; Maguire et al., 2000; Witherspoon et al., 2006), two as‘fair’ (LOE = 3) (Gelbier & Winter, 1988; Koyuncuoglu et al., 2013) and one as ‘poor’ (LOE = 3) (de Blanco, 1996).
DISCUSSION
Despite the common nature of TDIs, to the authors’ knowledge, no systematic reviews looking into the clinical and radiographic success/survival of various VPT interventions in pulpal exposed traumatized permanent teeth have been reported. Due to the specific nature of TDIs, prospective controlled clinical trial are difficult to perform. Therefore, cohort, case-control and case series studies with a minimum of five cases were included in this review. Although of low evidence level, the decision to include case series was based on the number of factors.
Firstly, there is a paucity of the literature on this topic. Also, many such studies are considered in the literature as longitudinal single-arm studies on which the current dental trauma guidelines are based (Bourguignon et al., 2020; Krastl et al., 2021). These studies also included a large number of cases, treated using standardized protocols, which is more valuable than a standard case series (with no standardized protocol). As an example, one study reported 178 cases (Cvek, 1993), but because of the noncomparative nature of this study, for the purpose of our review, it was considered to be a case series according to the Algorithm suggested for classification of studies by National Institute for Health and Care Excellence (NICE, 2014).
The NIH quality assessment tool, one of the recommended tools by the NationalInstitute for Health and Care Excellence (NICE, 2014), was utilized in the current review as it enables the assessment of various study designs using comprehensive evaluation criteria. A 14-criteria based tool is used for controlled intervention studies and observational cohort studies, while a 9-criteria based tool is used for case series studies covering all aspects of bias including selection, detection, performance, attrition and reporting bias.
In this review, a total of 14 studies were included with an overall quality ranging from ‘good’ to ‘poor’. In the two clinical trials that were included, performance bias was high due to the lack of blinding of operators, which is quite clinically impractical due to the nature of the clinical intervention. Regarding detection bias, although blinding of assessors was claimed in some studies, it remained possible for the assessors to identify the treatment provided as a result of radiographic differences in material radio-opacities and crown discolouration associated with certain materials used. Additionally, both performance and reporting bias negatively affected the overall quality rating of the included retrospective case-control study. Despite the inherent limitations within uncontrolled clinical studies, the majority of these case series rated low bias. Unfortunately, based on the limited number of included RCTs, substantial heterogeneity in terms of clinical protocols, assessment criteria and out-come reporting among included studies a meta-analysis was not performed.
Additionally, several variables, including the VPT technique, haemostatic/irrigation agent used and the skill of the operator, pulp capping material, size of the pulpal exposure, time interval from trauma to VPT/ VPT to definitive coronal seal, the presence of a concomitant trauma, root development stage, pulp contamination appear to affect the prognosis of traumatized teeth with pulpal exposure. However, the evidence on some of these factors remains contradictory and will be briefly discussed in the context of this review.
Vital pulp treatments
In this review, partial pulpotomy was the main reported clinical procedure following traumatic pulpal exposure of vital permanent teeth, accounting for approximately 71.4% of the studies and the highest overall success rate (82.9–100%). On the contrary, full pulpotomy was reported in only 21.4% of studies with lower success rates (79.4–85.7%). With regard to direct pulp capping, a surprisingly low success rate of 19.5% was reported; however, these data cannot be generalized as data were extracted from a sole retrospective study design of a limited sample size. More recently, given the low reported success rates of direct pulp capping in comparison to partial pulpotomy its use in traumatized exposed pulps has been questioned (Krastl, Weiger, Ebeleseder, et al., 2021). Indeed, partial pulpotomy has been reported to provide better control of the exposure wound, hence enhancing the clinical stability of the pulp capping material(Cvek, 1978). Additionally, irrespective of the applied treatment, various clinicalsteps such as water cooling, irrigation solutions, haemostatic agent, applied pressure and aseptic field could potentially affect the treatment outcome and should be considered in future studies. Although, the effect of different irrigation solutions/concentrations on the survival of stem cells from the apical papilla has been widely studied (Martin et al., 2014; Trevino et al., 2011), little is known about their effect on the superficial pulp tissue following traumatic pulp exposure. Furthermore, the skill of the (operator treatment provider) was under-reported in the majority of the included studies. Although, it is logical to assume that the skill of the operator directly affects the treatment outcome. Nevertheless, the effect of this factor on the success and survival of treated teeth has not been ascertained.
Pulp capping materials
Several pulp capping materials have been used with variable physio-mechanical properties such as sealing ability, wound healing, antimicrobial efficacy, biocompatibility and bioactivity properties when placed in contact with the inflamed pulp tissue (da Rosa, Cocco, et al., 2018). Calcium hydroxide is well-known as the standard pulp capping material with a long track record of clinical success mainly related to its excellent antimicrobial activity, biocompatibility and the ability to induce calcific bridge formation (Krastl et al., 2021; Mohammadi & Dummer, 2011).
In the current review, Ca(OH)2 was the main reported material in 10 out of the 14 included studies, with an overall high clinical and radiographic success (79.4–100%). Calcium hydroxide drawbacks such as mechanical instability, poor sealing ability and a ‘tunnel defect’ in the newly formed calcific bridge (Krastl et al., 2021; Mohammadi & Dummer, 2011) have been documented in the literature that led to further material innovation. Additionally, the occurrence of internal resorption has also been reported with Ca(OH)2 use as a pulp medicament in traumatized permanent teeth with pulp exposures (Akhlaghi & Khademi, 2015).
The use of MTA, a bioactive endodontic cement mainly comprised of calcium and silicate elements, introduced by Torabinejad and colleagues in the 1990s, is another well-known favourable pulp capping material (Torabinejad et al., 1993). Advantages of MTA, such as no or low solubility, high pH, excellent sealing and biocompatibility properties are well documented (Parirokh et al., 2018). However, difficult handling characteristics, prolonged setting time, high cost and tooth discolouration are known potential clinical drawbacks (Parirokh et al., 2018). Additionally, in spite of continuous material improvements, tooth discolouration remains an adverse clinical issue (Belobrov & Parashos, 2011; Sabeti et al., 2021). In the current review, ProRoot MTA was utilized in two case series and an RCT in comparison with Biodentine®, with an overall high clinical and radiographic success (80–100%). Despite, previous systematic reviews reporting a comparable clinical success rate of ProRoot Grey MTA and Ca(OH)2 as a pulp capping material for partial pulpotomy in permanent molars with deep carious lesions (Qudeimat et al., 2007), none of the included studies in this systematic review directly compared both these materials. It would not be prudent to compare the results from the use of such materials used for VPT in trauma and caries as the pathophysiology of the pulp is completely different in these two clinical scenarios. In carious exposures, the pulp is likely to be inflamed whereas in traumatic pulp exposures, it is more likely to be merely contaminated with perhaps inflammation in just the superficial part exposed to the oral environment, especially where treatments are performed quite soon after the injury (Cvek et al., 1982; Heide & Mjör, 1983).
To circumvent the limitations of MTA, a variety of new bioactive cements based on calcium silicate composition such as Biodentine® (Septodont) and IRoot® BP Plus (Innovative BioCeramix), have been developed. IRoot® BP Plus has been shown to enhance human dental pulp cells attachment, proliferation, migration, mineralization and dentine bridge formation (Mahgoub et al., 2019). This review found that in comparison with Ca(OH)2, IRoot® BP Plus had a greater ability to increase calcific bridge thickness; however, overall similar clinical and radiographic success was reported. In line with these results, the cost-effectiveness of IRoot® BP Plus in comparison to Ca(OH)2 will most likely hinder clinicians to select new and expensive materials of a similar clinical outcome to cheaper competitors.
Biodentine® as a ‘dentine replacement’ material has also gained significant clinical attention. Recent RCTs assessing ProRoot white MTA and Biodentine® as a pulp capping material found no significant difference between clinical and radiographic success rates for both materials following full pulpotomy in carious (Abuelniel et al., 2021) and traumatized (Abuelniel et al., 2020) exposed pulp tissue. MTA has been commonly linked to coronal discolouration of teeth, which has been attributed to the presence of bismuth oxide content. Similarly, this review found a significantly higher coronal discolouration with MTA use as compared to Biodentine®, thus suggestive that Biodentine® may be considered a suitable alternative material with better aesthetic outcomes, which is especially significant when carrying out VPT in permanent anterior teeth.
In addition, irrespective of material classification, other factors such as blood contamination (Chen et al., 2020; Lenherr et al., 2012), type of irrigant solution (Camilleri et al., 2020), the influence of light and environmental conditions (Vallés et al., 2013a, 2013b) should be carefully controlled and may negatively contribute to tooth discolouration.
Size of pulp exposure
The effect of the size of the pulpal exposure on the prognosis of traumatized teeth has been assessed in some studies. The size of the pulpal exposure ranging from 0.5 to 4.0 mm following Ca(OH)2 partial pulpotomy in relation with traumatized teeth resulted in no influence on the frequency of healing (Cvek, 1978). Similarly, Fuks and colleagues also found that the size of pulp exposure, did not affect treatment outcome, as long as the remaining pulp tissue is vital (Fuks et al., 1987, 1993).
Time interval between trauma, VPT treatment and placement of definitive restoration
The time interval between trauma and VPT treatment has been reported with conflicting results. In three case series, the time interval from trauma to treatment did not affect treatment outcome, as long as the remaining pulp tissue is vital (Cvek, 1978; Fuks et al., 1987, 1993). Contrastingly, a study by Cvek of a 3–15-years follow-up found a statistically significant difference in the frequency of healing in teeth treated within 72 h after trauma in comparison to those treated after a longer time interval (Cvek, 1993). This is echoed by Gilber and Winter, who reported that only 12% of teeth treated within 24 h lost their vitality compared with 32% of teeth treated after 24 h following pulp exposure (Gelbier & Winter, 1988). The time interval between the VPT treatment and placement of a definitive restoration varied, either at the first visit or subsequent visits, within the included studies. In a retrospective study design, the immediate placement of a bonded definitive coronal seal increased the mean survival time for vitality in both mature and immature teeth (Maguire et al., 2000). Indeed following VPT in a traumatized tooth, it is advisable that a definitive bonded restoration should be placed as soon as possible, ideally during the same visit, to prevent any unwanted coronal leakage and subsequent pulp infection (Krastl et al., 2021). Unfortunately, in several studies included in this review, a definitive bonded restoration was placed at a subsequent follow-up visit. The effects of this delay on the success and survival of treated teeth cannot be ascertained in the context of this review; however, it is highly encouraged that placement of a definitive bonded restoration at the initial treatment visit.
Concomitant trauma
The presence of concomitant injury, sustaining more than one injury, is reported to create a synergist effect, hence resulting in a more detrimental effect than a single injury (Bourguignon et al., 2020). In this review, Haikal et al. (2020) reported that the presence of concurrent luxation injury was the only independent variable that significantly affected the treatment outcome. In line with the above, a significant increase of pulp necrosis in mature teeth with crown fractures combined with concussion or subluxation injuries has been reported (Lauridsen et al., 2012). However, we must acknowledge that the healing scenario is complex and multifactorial related to patient, trauma or treatment factors (Lauridsen et al., 2012).
Stage of root development
The effects of stage of root development (immature, mature) on the clinical outcome following VPT has been debatable, with previous reports restricting VPT to only young patients with immature roots (Koyuncuoglu et al., 2013). However, several studies have shown that patients with agesranging from 6 to 70-years-old have been treated successfully with VPT (Aguilar & Linsuwanont, 2011).
This is in line with the results of the current systematic review. Indeed, it has been shown that the complete removal of the inflamed pulp is a critical clinical factor for pulp healing, rather than the stage of root development (Aguilar & Linsuwanont, 2011).
Pulpal diagnosis
The diagnosis of the injured pulp status is an important clinical factor; however, accurate diagnosis even to the experienced clinician is challenging, especially in young patients who may be uncooperative following a traumatic injury. Additionally, the commonly used pulp sensibility tests (electric and/or thermal stimulation) physiologically rely on a functional vascular supply. However, pulpal oedema following trauma results in a temporary loss of sensibility, limiting their diagnostic accuracy (Krastl et al., 2021).
Moreover, pulp sensibility testing especially in immature teeth remains a challenge, partly due to delay in the full development of the plexus of Rashkow, which has been shown to take place up to 5-years post tooth eruption (Johnsen, 1985). Furthermore, pulp sensibility testing in teeth, which have undergone VPT and have a thick layer of pulp capping material and restorative coronal seal material, such as those with deep coronal pulpotomy may impede responses to conventional cold and electric pulp tests, with clinicians depending mainly on radiographic evidence of continued root development as the most reliable sign of pulp vitality. Physiology aside, it should also be acknowledged that pulp sensibility testing in anxious young patients cannot always be substantiated and are often unreliable.
Othersuggested forms of pulp testing that have shown to offer a more objective assessment and better diagnostic accuracy in evaluating the tooth’s vascular supply include the use of Laser Doppler Flowmetry or pulse oximetry (Krastl et al., 2021). However, it should be noted that studies supporting its use were subject to a high level of bias (Ghouth et al., 2018). The use of such device was further challenged by the results of an RCT showing a subclinical accuracy of the Laser Doppler Flowmetry (Ghouth et al., 2019).
Strengths, limitations and future directions Inherent strengths of this systematic review rely on the robust inclusion and exclusion criteria to maintain the focus of the review question. In addition to the risk of bias assessment, the LOE of the included studies was graded to reflect and compare the quality of evidence. However, this systematic review has the following limitations: the majority of included studies were uncontrolled clinical studies with inherent bias resulting from the lack of a control group, the presence of substantial heterogeneity in terms of clinical protocols, assessment criteria and outcome reporting among included studies, which prevented data synthesis, the exclusion of non-English language manuscripts as a result of lack of funding and access to professional translation services.
Further assessment of the effect of the VPT technique, pulp capping material, size of the pulpal exposure, time interval from trauma to VPT, time interval from VPT to definitive coronal seal, the presence of a concomitant trauma, root development stage, pulp contamination, haemostatic/irrigation agent used and the skill of the operator, is recommended in future studies using well designed controlled prospective clinical trials. In order to standardize future studies, the authors would like to recommend a list of minimum clinical and radiographic criteria for outcome assessment as outlined in Table 4. Such criteria would help improve study standardization and reduce heterogeneity between studies. Both clinical and radiographic success parameters should be clearly defined, assessed and reported. Additionally, all RCTs should register and strictly comply with the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
TABLE 4 Recommended criteria for outcome evaluation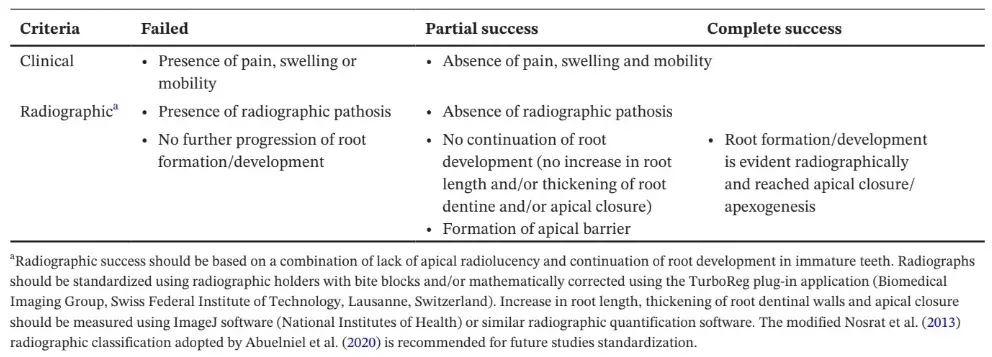
CONCLUSION
Despite the common occurrence of complicated TDIs, high-quality evidence-based studies are scarce. The present systematic review reports high clinical and radiographic success rates of VPT interventions in the treatment of traumatized vital permanent teeth, although based on limited clinical evidence of variable quality rating. Calcium hydroxide was the most studied pulp capping material with favourable clinical outcomes.
The most recent evidence, although of limited studies, also suggests that alternative bioactive biomaterials (Biodentine®, IRoot® BP and MTA) are associated with high clinical and radiographic success and are regarded as a suitable VPT biomaterial. Crown discolouration following the use of MTA limits its use in the management of traumatized anterior teeth in comparison to Ca(OH)2 and other less discolouring calcium silicate material such as Biodentine® and non-bismuth oxide–containing MTA.
Further details about permanent teeth treatment are accessible for you to learn on our course "WHAT’S NEW in pediatric dentistry".
List of author:
Manal Matoug-Elwerfelli, Ahmed S. ElSheshtawy, Monty Duggal, Huei Jinn Tong, Hani Nazzal
References
Abuelniel, G.M., Duggal, M.S. & Kabel, N. (2020) A comparison of MTA and biodentine as medicaments for pulpotomy in traumatized anterior immature permanent teeth: a randomized clinical trial. Dental Traumatology, 36, 400–410.
Abuelniel, G.M., Duggal, M.S., Duggal, S. & Kabel, N.R. (2021) Evaluation of mineral trioxide aggregate and biodentine as pulpotomy agents in immature first permanent molars with carious pulp exposure: a randomised clinical trial. European Journal of Paediatric Dentistry, 22, 19–25.
Aguilar, P. & Linsuwanont, P. (2011) Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. Journal of Endodontics, 37, 581–587.
Akhlaghi, N. & Khademi, A. (2015) Outcomes of vital pulp therapy in permanent teeth with different medicaments based on review of the literature. Dental Research Journal, 12, 406–417.
Andersson, L. (2013) Epidemiology of traumatic dental injuries. Pediatric Dentistry, 35, 102–105.
Belobrov, I. & Parashos, P. (2011) Treatment of tooth discoloration after the use of white mineral trioxide aggregate. Journal of Endodontics, 37, 1017–1020.
Bjørndal, L., Reit, C., Bruun, G., Markvart, M., Kjaeldgaard, M., Näsman, P. et al. (2010) Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. European Journal of Oral Sciences, 118, 290–297.
de Blanco, L.P. (1996) Treatment of crown fractures with pulp exposure. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics, 82, 564–568.
Bourguignon, C., Cohenca, N., Lauridsen, E., Flores, M.T., O'Connell, A.C., Day, P.F. et al.(2020)International association of dentaltraumatology guidelinesforthe management of traumatic dental injuries: 1. Fractures and luxations. Dental Traumatology, 36, 314–330.
Camilleri, J., Borg, J., Damidot, D., Salvadori, E., Pilecki, P., Zaslansky, P. et al. (2020) Colour and chemical stability of bismuth oxide in dental materials with solutions used in routine clinical practice. PLoS One, 15, e0240634.
Chen, S.J., Karabucak, B., Steffen, J.J., Yu, Y.H. & Kohli, M.R. (2020) Spectrophotometric analysis of coronal tooth discoloration induced by tricalcium silicate cements in the presence of blood. Journal of Endodontics, 46, 1913–1919.
Cohenca, N., Paranjpe, A. & Berg,J. (2013) Vital pulp therapy. Dental Clinics of North America, 57, 59–73.
Cushley, S., Duncan, H.F., Lappin, M.J., Chua, P., Elamin, A.D., Clarke, M. et al. (2021) Efficacy of direct pulp capping for management of cariously exposed pulps in permanent teeth: a systematic review and meta-analysis. International Endodontic Journal, 54, 556–571.
Cvek, M. (1978) A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. Journal of Endodontics, 8, 232–237.
Cvek, M. (1993) Partial pulpotomy in crown-fractured incisors-results 3 to 15 years after treatment. Acta Stomatologica Croatica, 27, 167–173.
Cvek, M., Cleaton-Jones, P.E., Austin, J.C. & Andreasen, J.O. (1982) Pulp reactionsto exposure after experimental crown fractures or grinding in adult monkeys. Journal of Endodontics, 8, 391–397.
DiAngelis, A.J., Andreasen, J.O., Ebeleseder, K.A., Bakland, L.K., Malmgren, B. & Barnett, F. et al. (2016) Guidelines for the management of traumatic dental injuries: 1. fractures and luxations of permanent teeth. Pediatric Dentistry, 38, 358–368.
Duncan, H.F., Galler, K.M., Tomson, P.L., Simon, S., El-Karim, I., Kundzina, R. et al. (2019) European Society of Endodontology Position Statement: management of deep caries and the exposed pulp. International Endodontic Journal, 52, 923–934.
Fuks, A.B., Cosack, A., Klein, H. & Eidelman, E. (1987) Partial pulpotomy as a treatment alternative for exposed pulps in crown-fractured permanent incisors. Endodontics & Dental Traumatology, 3, 100–102.
Fuks, A.B., Gavra, S. & Chosack, A. (1993) Long-term followup of traumatized incisors treated by partial pulpotomy. Pediatric Dentistry, 15, 334–336.
Gelbier, M.J. & Winter, G.B. (1988) Traumatised incisors treated by vital pulpotomy: a retrospective study. British Dental Journal, 164, 319–323.
George, A., Sousa, M.S., Kong, A.C., Blinkhorn, A., Patterson Norrie, T., Foster, J. et al. (2019) Effectiveness of preventive dental programs offered to mothers by non-dental professionalsto control early childhood dental caries: a review. BMC Oral Health, 19, 1–9.
Ghouth, N., Duggal, M.S., BaniHani, A. & Nazzal, H. (2018) The diagnostic accuracy of laser doppler flowmetry in assessing pulp blood flow in permanent teeth: a systematic review. Dental Traumatology, 34, 311–319.
Ghouth, N., Duggal, M.S., Kang, J. & Nazzal, H. (2019) A diagnostic accuracy study of laser doppler flowmetry for the assessment of pulpal status in children’s permanent incisor teeth. Journal of Endodontics, 45, 543–548.
Haikal, L., Ferraz dos Santos, B., Vu, D.D., Braniste, M. & Dabbagh, B. (2020) Biodentine pulpotomies on permanent traumatized teeth with complicated crown fractures.Journal of Endodontics, 46, 1204–1209.
Heide, S. & Mjör, I.A. (1983) Pulp reactions to experimental exposures in young permanent monkey teeth. International Endodontic Journal, 16, 11–19.
Johnsen, D.C. (1985) Innervation of teeth: qualitative, quantitative, and developmental assessment. Journal of Dental Research, 64 Spec No, 555–563.
Klein, H., Fuks, A., Eidelman, E. & Chosack, A. (1985) Partial pulpotomy following complicated crown fracture in permanent incisors: a clinical and radiographical study. The Journal of Pedodontics, 9, 142–147.
Kodonas, K., Fardi, A., Gogos, C. & Economides, N. (2021) Scientometric analysis of vital pulp therapy studies. International Endodontic Journal, 54, 220–230.
Koyuncuoglu, G., Gorken, F.N., Ikikarakayali, G., Zorlu, S., Erdem, A.P., Sepet, E. et al. (2013) Management of open apices in thirteen traumatized permanent incisors using mineral trioxide aggregate: case series. Pediatric Dental Journal, 23, 51–56.
Krastl, G., Weiger, R., Ebeleseder, K. & Galler, K. (2021) Present status and future directions – endodontic management of traumatic injuries to permanent teeth. International Endodontic Journal, 00, 1–17.
Krastl, G., Weiger, R., Filippi, A., Van Waes, H., Ebeleseder, K., Ree, M. et al.(2021) Endodontic management of traumatized permanent teeth: a comprehensive review. International Endodontic Journal, 54, 1221–1245.
Krastl, G., Weiger, R., Filippi, A., Van Waes, H., Ebeleseder, K., Ree, M. et al. (2021) European Society of Endodontology position statement: endodontic management of traumatized permanent teeth. International Endodontic Journal, 54, 1473–1481.
Lauridsen,E.,Hermann, N.V., Gerds,T.A., Ahrensburg, S.S., Kreiborg, S. & Andreasen, J.O. (2012) Combination injuries 1. The risk of pulp necrosis in permanent teeth with concussion injuries and concomitant crown fractures. Dental Traumatology, 28, 364–370.
Lenherr, P., Allgayer, N., Weiger, R., Filippi, A., Attin, T. & Krastl, G. (2012) Tooth discoloration induced by endodontic materials: a laboratory study. International Endodontic Journal, 45, 942–949.
Maguire, A., Murray, J.J. & Al-Majed, I. (2000) A retrospective study of treatment provided in the primary and secondary care services for children attending a dental hospital following complicated crown fracture in the permanent dentition. International Journal of Paediatric Dentistry, 10, 182–190.
Mahgoub, N., Alqadasi, B., Aldhorae, K., Assiry, A., Altawili, Z. &Tao, H. (2019) Comparison between iRoot BP Plus (endosequence root repair material) and mineral trioxide aggregate as pulpcapping agents: a systematic review. Journal of International Society of Preventive and Community Dentistry, 9, 542–552.
Martin, D.E., De Almeida, J.F.A., Henry, M.A., Khaing, Z.Z., Schmidt, C.E., Teixeira, F.B. et al. (2014) Concentration-dependent effect of sodium hypochlorite on stem cells of apical papilla survival and differentiation. Journal of Endodontics, 40, 51–55.
Mohammadi, Z. & Dummer, P.M.H. (2011) Properties and applications of calcium hydroxide in endodontics and dental traumatology. International Endodontic Journal, 44, 697–730.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G. & PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6, e1000097.
Munir, A., Zehnder, M. & Rechenberg, D.K. (2020) Wound lavage in studies on vital pulp therapy of permanent teeth with carious exposures: a qualitative systematic review. Journal of Clinical Medicine, 9, 984.
Nazzal, H. & Duggal, M.S. (2017) Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? European Archives of Paediatric Dentistry, 18, 3–15. NICE. (2014) Developing NICE guidelines: the manual.
Nosrat, A., Seifi, A. & Asgary, S. (2013) Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: a randomized clinical trial. International Journal of Paediatric Dentistry, 23, 56–63.
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. (2016) Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5, 1–10.
Parirokh, M., Torabinejad, M. & Dummer, P.M.H. (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview – part I: vital pulp therapy. International Endodontic Journal, 51, 177–205.
Qudeimat, M.A., Barrieshi-Nusair, K.M. & Owais, A.I. (2007) Calcium hydroxide vs. mineral trioxide aggregates for partial pulpotomy of permanent molars with deep caries. European Archives of Paediatric Dentistry, 8, 99–104.
Rao,Q.,Kuang,J.,Mao,C.,Dai,J.,Hu,L.,Lei,Z.etal.(2020)Comparison of iRoot BP Plus and calcium hydroxide as pulpotomy materials in permanent incisors with complicated crown fractures: a retrospective study. Journal of Endodontics, 46, 352–357.
da Rosa, W.L.O., Cocco, A.R., Silva, T.M.d., Mesquita, L.C., Galarça, A.D., da Silva, A.F. et al. (2018) Current trends and future perspectives of dental pulp capping materials: A systematic review. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 106, 1358–1368.
da Rosa, W.L.O., Piva, E. & da Silva, A.F. (2018) Disclosing the physiology of pulp tissue for vital pulp therapy. International Endodontic Journal, 51, 829–846.
Sabeti, M., Huang, Y., Chung, Y.J. & Azarpazhooh, A. (2021) Prognosis of vital pulp therapy on permanent dentition: a systematic review and meta-analysis of randomized controlled trials. Journal of Endodontics, 47, 1683–1695.
SIGN 50 (2019) SIGN 50: A guideline developer’s handbook. Scottish Intercollegiate Guidelines Network (SIGN) Grading System.
Torabinejad, M., Watson, T.F. & Ford, T.P. (1993) Sealing ability of a mineral trioxide aggregate when used as a root end filling material. Journal of Endodontics, 19, 591–595.
Trevino, E.G., Patwardhan, A.N., Henry, M.A., Perry, G., Dybdal-Hargreaves, N., Hargreaves, K.M. et al. (2011) Effect of irrigants on the survival of human stem cells of the apical papilla in a platelet-rich plasma scaffold in human root tips. Journal of Endodontics, 37, 1109–1115.
Vallés, M., Mercadé, M., Duran-Sindreu, F., Bourdelande, J.L. & Roig, M. (2013a) Color stability of white mineral trioxide aggregate. Clinical Oral Investigations, 17, 1155–1159.
Vallés, M., Mercadé, M., Duran-Sindreu, F., Bourdelande, J.L. &
Roig, M. (2013b) Influence of light and oxygen on the color stability of five calcium silicate–based materials. Journal of Endodontics, 39, 525–528.
Witherspoon, D.E., Small, J.C. & Harris, G.Z. (2006) Mineral trioxide aggregate pulpotomies: a case series outcomes assessment. Journal of the American Dental Association, 137, 610–618.
Yang, Y., Xia, B., Xu, Z., Dou, G., Lei, Y. & Yong, W. (2020) The effect of partial pulpotomy with iRoot BP Plus in traumatised immature permanent teeth: a randomised prospective controlled trial. Dental Traumatology, 36, 518–525.

Article
OHI-S
23 April 2024

Article
OHI-S
25 April 2024
Video
OHI-S
11 January 2024


