Treatment of temporomandibular dysfunction with jaw functional orthopedics: a retrospective study
Abstract
What are my chances of getting better?” And “How long will it take for the discomfort to improve?” are the two basic questions asked by individuals after they know about the influence of the stomatognathic system (SS) on their discomfort. Despite the biological unpredictability and variation, these individuals need some information. When searching in MEDLINE, some parameters may be found, but there are none about Jaw Functional Orthopedics (JFO). This study sample was composed of 146 patients with TMD and/or headache/neck pains, who were treated with JFO and divided into three groups. Group 1 exclusively with TMD; Group 2 with head and/or neck pain without symptoms of TMD (pain on palpation or movement); and Group 3 with TMD and head/neck pain. The symptoms monitored were arthralgia, and myalgia of the temporal, masseter or suprahyoid muscles, neck pain on movement or palpation, headache and cervicalgia reported. Odontogenic pain and headache originating from other sources (sinusitis, flu, pre-menstrual period, photophobia, hangover, etc.) were excluded from the study. The sample was aligned with the literature relative to prevalence of age and sex. Results showed that JFO treatment was effective in patients of the three groups. There was no statistical difference in mean time for remission among the groups. The results and conclusions should be analyzed with caution since there was no control group, and long term follow up is needed to check the behavior of the symptoms. However, the data from this study suggested that JFO was an efficient tool for treatment of patients with occlusal and biomechanical alterations of the SS, with chronic TMD, head and/or neck pain in a short period of time.
You have the opportunity to gather more in-depth information about temporomandibular disorders treatment in our Online congress of Myofunctional Orthodontics and Functional Jaw Orthopedics.
Introduction
JFO is a Specialty in Brazil and a branch of Dentistry around the world. Basically, it deals with functional, removable intra-oral appliances, with very well defined rules, which always lead to Mandibular Posture Changes (MPC), and changes in the tongue position [1-4]. This is the sine qua non condition for an appliance to be classified as a Functional Orthopedic Appliance (FOA) and defines the difference between a removable orthodontic appliance and a FOA [1, 2]. MPC achieved with functional appliances was first described by Pierre Robin in 1902 [5]. Since Costen [6], in 1934, described otologic symptoms related to the temporomandibular joint, much has been discussed on the etiology and treatment protocols for temporomandibular disorders (TMD).
With regard to the psychosocial aspect of the problem, there has been some discussion about its real influence on the TMD [7-11]. Lobbezoo el al. [12], in an international consensus described clenching/bruxism as a behavior but not all bruxers have TMD.
The role of occlusion in TMD has also been extensively discussed, and the results have been somewhat controversial. Searching in MEDLINE, using the keywords “temporomandibular pain AND occlusion”, the oldest article found was Granger’s dating back to 1958 [13]. When using “TMD AND occlusion” the oldest found were those of Pullinger and Monteiro [14] dated 1988.
The discussion has been going on for a long time and shows the lack of consensus on the results; moreover, occlusal factors are no longer considered the main etiology. This article does not aim to end the discussion, but rather to add some data and contribute to knowledge about TMD. “What are my chances of getting better?” And “How long will it take for the discomfort to improve?” are the two basic questions asked by individuals after knowing about the influence of the stomatognathic system (SS) on their discomfort. When searching MEDLINE (05/03/2021) about time for improvement of symptoms, 36 references were found [8, 10, 13, 15-36]. Since none of them was about JFO, the questions still remained unanswered, even if JFO were to help in the treatment of TMD.
Changes in the condylar position and mandibular biomechanics due to occlusal changes have been reported in the literature [1, 2, 37-41], and so have changes in the condyle/fossa relationship with the use of intraoral splints [42] Neck muscles are also affected by occlusal changes [43-46] and by the use of devices that change jaw position [47]. Individuals who have TMD symptoms for the first time, should not be treated with JFO. Conservative treatment would be the most suitable [19, 24]. But individuals with chronic pain, occlusal and biomechanical alterations of the SS, who experience no improvement with conservative treatment should receive irreversible intervention [46], and are serious candidates for treatment with JFO.
It is true that not all individuals with altered biomechanics of the SS are symptomatic, just as not all smokers develop lung cancer. The converse is also true: those who do not smoke are not free of the risk of contracting lung cancer; and those who have no biomechanical changes are not free of symptoms of TMD. Both (as is the case with most diseases) are multifactorial problems. This understanding is of fundamental importance in the indication of JFO for the treatment of TMD.
Methodology
A sample of patients with chronic TMD (arthralgia and/or myalgia), headache and cervicalgia, treated in private practice, in a 5-year period, were studied. The individuals who had symptoms for the first time, and those with systemic arthritis were excluded from this study. The sample consisted of 146 individuals: 121 (82.87 %) were female and 25 (17.13 %) were male. The mean age at the time of pretreatment data collection was = 35.37±15.07 (ranging from a minimum of 6 and a maximum of 76 years).
The subjects were divided into three groups. Group 1 (G1) consisted of individuals with TMD, temporomandibular joint (TMJ) pain and/or masseter, temporalis, and suprahyoid muscle pain on movement or palpation only. Group 2 (G2) consisted of individuals with headache and/or neck pain without signs or symptoms of TMD. Group 3 (G3) consisted of individuals with symptoms of TMD (the same as G1) and headache and/or neck pain. The division was made due to the need for distinct diagnoses and clinical procedures between the groups. In G1, where the signs and symptoms of TMD were evident there was no need for differential diagnosis, while in G2 and G3, the differential diagnosis was made not only to eliminate incorrect diagnosis but to detect any co-morbidity.
In G1 𝑛 = 43, of whom 7 (16.3 %) were male and 36 (83.7 %), female. The mean age of patients at the time of data collection was = 31.91 ± 15.42 (range, minimum 6 to maximum of 63 years). In G2 𝑛 = 49, of whom 6 (12.5 %) were male and 42 (87.5 %), female. The mean age of patients at the time of data collection was = 38.10 ± 12.87 (range, minimum 9 to maximum of 67 years). In G3 𝑛 = 54, of whom 14 (26.9 %) were male and 38 (73.1 %), female. The mean age of patients at the time of data collection was= 35.71 ± 16.33 (range, minimum 6 to maximum of 76 years).
The symptoms monitored were arthralgia and myalgia of the temporal, masseter and suprahyod muscles, on movement and/or palpation for G1 and G3, palpation of sternocleidomastoid, and trapezius muscles, and report of headache and/or cervicalgia for G2 and G3. Headaches originating from other sources (sinusitis, flu, pre-menstrual period, hangover, etc) were not considered.
Clinical examination of the bilateral TMJ and muscle palpation were performed as described in the literature [40, 49-51]. Palpation of the trapezius and sternocleidomastoid was performed bilaterally, using the protocol by Gelb and Gelb [38]. Excursive free movement and against resistance were analyzed for mandibular opening, protrusion, right and left lateral movements as described in the literature [38, 49].
Functional analyses of the SS with regard to the pattern of motion were made studying the protrusive movement in accordance with the recommendations by Simões [1, 2]. Lateral movements were analyzed relative to the skill to perform them (normal, impaired or unable), the direction of movement (lateroprotrusion, laterality or lateroretrusion), the asymmetry of the vertical dimension between the two side was assessed using parameters described by Simões [1, 2]. The range of motion of protrusive and lateral movements was measured in millimeters. The occlusal plane conditions were studied in paster models mounted on Planas gnathostato [52]. For diagnosis and control of the symptoms, a numerical scale was used [20] both on palpation and in the dynamic analysis, due to its reliability. Clinical and radiographic exams were performed for differential diagnosis of odontogenic pain.
All patients with neck pain had previously undergone physical therapy or were undergoing treatment without complete remission. They were all instructed not to change their behavior (continuing without treatment or keeping to the current treatment parameters). In the same way, patients with headache were also requested not to change the present treatment situation they were undergoing. The techniques used were Bimler’s [1, 2, 53], Planas’ [1, 2, 52, 53], Simões’ [1, 2, 53] and/or Santiago’s [54-56].
No Control Group was used, in accordance with a tendency in the literature [33, 34, 50]. Considering humanitarian reasons, the impossibility of contacting individuals who declined treatment, and inaccuracy of diagnosis because another type of treatment was being carried out, were the reasons why no control group was used.
The data were analyzed by the program SPSS for Windows version 17.0, SPSS Inc, Chicago, IL, USA). Regarding sex and age, the non-paired t test was used. For comparison of symptoms before and after treatment we used Shapiro-Wilk test for normal distribution, 𝑝 = 0.038. (not normal), we used the Wilcoxon test for paired samples with two non-normal sample distribution. Time for remission analyses did not show normal distribution (Kolmogorov-Smirnov test, 𝑝 < 0.001). The non-parametric test Kruskal-Wallis followed by the Mann-Whitney test for two non-paired samples with Bonferroni correction were used to test the remission time between groups.
Results
In G1 the pretreatment intensity of TMJ symptoms were = 5.28 ± 2.45 [(95 % CI 4.45 to 6.11)], (minimum 2 and maximum 10). After being submitted to treatment the values were = 0 ± 0 0 minimum and maximum. Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.038 (not normal). When using the Wilcoxon test for paired samples with two non-normal distribution, 𝑝 = 0.000 there was statistically significant difference between the intensity of arthralgia observed before and after treatment. (Table 1) The intensity values of muscle symptoms before treatment were 5.74 ± 2.39 [(95 % CI 4.70 to 6.78)], (minimum 2 and maximum 10). Shapiro-Wilk test for normal distribution, 𝑝 = 0.110 (normal). The values for symptoms after treatment were = 0 ± 0 0 minimum and maximum. Using the 𝑡 test for 2 paired samples with normal distribution, 𝑝 = 0.000 also showed statistically significant difference. The average time of remission was 49.11 days +–45.58 days ranging from 6 to 196 days (Table 1).
Table 1. Symptoms before and after treatment
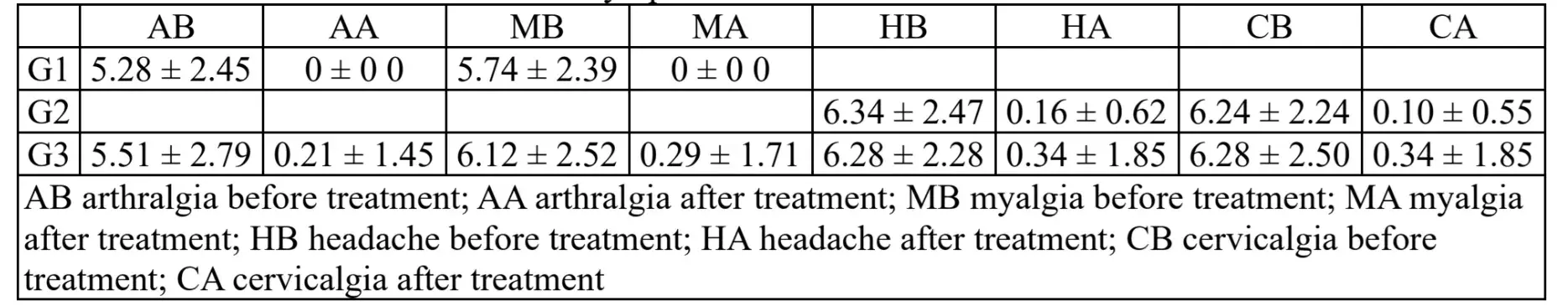
In G2 the values for intensity of headache symptoms before treatment were = 6.34 ± 2.47 [(95 % CI 5.45 to 7.23)], (minimum 2 and maximum 10). Using Shapiro-Wilk test for normal distribution, p = 0.043 (not normal). Intensity values of headache reported after treatment = 0.16 ± 0.62 [(95 % CI -0.07 - 0.38)], (minimum of 0 and a maximum of 3). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.000 (not normal). Wilcoxon test for paired samples with two non-normal distribution, 𝑝 = 0.000. There was statistically significant difference between the intensity values for headaches observed before and after treatment.
Initial values for symptoms of cervicalgia were = 6.24 ± 2.24 [(95 % CI 5.39 to 7.10)], (minimum of 3 and a maximum of 10). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.034 (not normal). Intensity values for cervicalgia after treatment were = 0.10 ± 0.55 [(95 % CI -0.11 - 0.32)], (minimum of 0 and a maximum of 3). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.000 (not normal). Wilcoxon test for paired samples with two non-normal distribution, 𝑝 = 0.000. There was statistically significant difference between the score observed for neck pain before and after treatment. The average time for remission of symptoms was 42.63 days with standard deviation of 43.82 days ranging from 3 to 217 days.
In G3 the initial intensity values for symptoms of headache were = 6.28 ± 2.28 [(95 % CI 5.41 to 7.14)]. Using Shapiro-Wilk test for normal distribution, p = 0.011 (not normal). Intensity values for symptoms after treatment were = 0.34 ± 1.85 [(95 % CI -0.36 - 1.05)], (minimum of 0 and a maximum of 10). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.000 (not normal).
Wilcoxon test for paired samples with two non-normal distribution, 𝑝 = 0.000 (Table 1). There was statistically significant difference between the intensity of values for headache observed before and after treatment. Intensity values for cervicalgia symptoms before treatment were 6.28 ± 2.50 [(95 % CI 5.38 to 7.18)], (minimum 2 and maximum 10). Using Shapiro-Wilk test for normal distribution, p = 0.016 (not normal). Intensity values for symptoms after treatment were = 0.34 ± 1.85 [(95 % CI -0.36 - 1.05)], (minimum of 0 and a maximum of 10). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.000 (not normal). Wilcoxon test for paired samples with two non-normal distribution), 𝑝 = 0.000. There was statistically significant difference between the score observed for cervicalgia before and after treatment. The intensity values for arthralgia before treatment were = 5.51 ± 2.79 [(95 % CI 4.69 to 6.33)], (minimum of one and maximum of 10). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.001 (not normal). Intensity of symptoms after treatment = 0.21 ± 1.45 [(95 % CI -0.22 - 0.64)], (minimum of 0 and a maximum of 10). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.000 (not normal). Wilcoxon test for paired samples with two non-normal distribution, 𝑝 = 0.000. There was statistically significant difference between the intensity values for arthralgia observed before and after treatment. The intensity values for symptoms of myalgia before treatment were = 6.12 ± 2.52 [(95 % CI 5.23 to 7.00)], (minimum 2 and maximum 10). Shapiro-Wilk test for normal distribution, p = 0.016 (not normal). Intensity values for symptoms after treatment were = 0.29 ± 1.71 [(95 % CI -0.30 - 0.89)], (minimum of 0 and a maximum of 10). Using Shapiro-Wilk test for normal distribution, 𝑝 = 0.000 (not normal). Wilcoxon test for paired samples with two non-normal distribution, 𝑝 = 0.000. There was statistically significant difference between the values for myalgia observed before and after treatment (Table 1). The average time for remission of symptoms was 38.82 days with standard deviation of 36.18 days ranging from 1 to 175 days.
With regard to the time needed for remission of symptoms, using the one way ANOVA (parametric test) for the 3 groups (𝑝 = 0.556), using the Tukey HSD test comparing: G1 and G2 𝑝 = 0.910; G1 and G3 𝑝 = 0.893; G2 and G3 𝑝 = 0.867. There was no statistically significant difference between G1, G2 and G3.
Discussion
This sample was in alignment with the literature relative to populations seeking TMD treatment in terms of mean age [50, 57-63] and prevalence of sex [50, 57-61]. The diagnosis of TMD in children and adolescents (11 subjects in the first decade of life and 12 the second) was also in alignment with the literature [62, 63].
As regards the technique used in treatment, it was not possible to compare the data of this study with findings in the literature since no study was found, reporting the efficacy of JFO in the treatment of TMD.
With the use of JFO, the mean time for statistically significant improvement to be shown was 38.83 days whereas with the use of cognitive and drug therapy, it took 7 weeks [58], and from 6 weeks up to 3 months with the use of cognitive therapy [27, 29, 59], respectively. With physical therapy and exercise in a period of two weeks. there was impact on the quality of life, but there was no mention of the rate of reduction in symptom intensity [30].
Concerning the efficacy of treatment with splints, results in literature were conflicting. There was a report of no improvement with the use of occlusal splints. without cognitive therapy [59], and reports of improvement with hard and soft splints [64, 65]. Piancino et al. [60] and Miralles et al. [51] showed improvement in the pattern of movement of the SS, with positive influence on the cervical spine, respectively, when using JFO, corroborating the findings of the present investigation.
Yatani et al. [19] and Vrbanovic & Alajbeg [66] reported long-term stability of TMD treatment using occlusal splints. This type of data was not found in the literature for the results of JFO, showing the need for research about the stability of JFO results. Improvement in symptoms using non conservative treatment of individuals with significant changes in the occlusal plane have been reported in the literature [28, 38, 49], however, reports of no improvement of these individuals with conservative therapy have also been found [31, 32].
Patients with TMD headache/and or cervicalgia, described by Fischer et al [32] as “complex regional pain syndrome”, had no improvement with splints, therefore, the data found for Group G3 suggest that the JFO can be a good option for the treatment of these patients. Sabine et al [42] showed that the change that occurred in the condyle/fossa could be modulated, depending on the type of device used. JFO was capable of changing the mandibular posture in more than 16 ways [1, 2].
Literature reports indicated that the use of drug therapy could be effective in a short period in the initial treatment, but the side effects of drugs contraindicated prolonged treatment [18, 23, 25]. As shown in the above-mentioned studies, the use of some drugs for acute symptoms, in a short period of time, could be a good choice, but side effects compromised the occlusal plan and mandibular biomechanics, therefore, contraindicating the use of drugs in cases of chronic TMD, and JFO could be a good choice of treatment.
The present data suggested that JFO could be an efficient tool for the treatment of TMD in individuals with significant occlusal and biomechanical alterations of the SS. Despite the high rate of efficacy found in the three groups, results should be viewed with caution, due to the absence of a control group. These individuals need to be followed-up in the long term to check the stability of results and to discard any possibility of the results of remission of symptoms in this investigation being a part of the natural course of TMD [10].
Further resources about temporomandibular disorders diagnosis and treatment are accessible for you to learn on our website.
Conclusions
The data suggested that Jaw Functional Orthopedics can be an effective tool in treating. Individuals with chronic symptoms of TMD, headache and/or neck pain with significant occlusal and biomechanical alterations of the SS.
There was no statistical difference in time of improvement of symptoms for TMD, Headache/neck pain, and TMD & headache/neck in pain patients treated with JFO.
The results should be carefully analyzed due to the absence of a control group.
Randomized controlled studies concerning the efficacy of JFO are needed as well as research to evaluate the long term stability of the treatment.
Authors: Orlando Santiago Júnior, Marcus Vinicius Lucas Ferreira, Rudolf Huebner
References
W. A. Simões, “Ortopedia Funcional dos Maxilares Através da Reabilitação Neuro-Oclusal,” (in Portuguese), 3th Ed., São Paulo; Editora Artes Médica. 2003.
W. A. Simões, “Ortopedia funzionale dei mascellari Attraverso La Riabilitazione Nuero-Occlusale,” (in Italian), 5th. Ed., Orbetello. 2010.
Jr O. Santiago, I. P. M. Santiago, R. C. O. Pedroni, “Tratamento da distoclusão com mordida aberta e com sobremordida com ortopedia funcional dos maxilares: diferenças clínicas e laboratoriais,” in: Nova visão em ortodontia: ortopedia funcional dos maxilares, (in Portuguese), São Paulo, Brazil, 2005.
Jr. O Santiago, I. P. M. Santiago, “Atlas de Construção de Aparelhos Ortopédicos Funcionais”, (in Portuguese), Ribeirão Preto, 1th Ed., 2010.
P. Robin, “Observation sur un nouvel appareil de redressement,” Rev Stomatol, Vol. 9, pp. 423-432, 1902.
J. B. Costen, “The present status of the mandibular joint syndrome in otolaryngology,” Transactions - American Academy of Ophthalmology and Otolaryngology, Vol. 55, pp. 809-823, 1951.
W. E. Bell, “Dores Orofaciais. Classificação, Diagnóstico, Tratamento,” (in Portuguese), Rio de Janeiro, Quintessence books, 1991.
P. A. Steed, “Etiological factors and temporomandibular treatment outcomes: the effects of trauma and psychological dysfunction,” The Functional orthodontist, Vol. 14, No. 4, pp. 17-20, 1997.
D. C. Turk, T. E. Rudy, H. S. Zaki, “Avaliação multiaxial e classificação de pacientes com dor de desordem temporomandibular,” (in Portuguese), in Dor Orofacial E Desordens Temporomandibulares, São Paulo, pp. 145-163, 2003.
R. Ohrbach and S. F. Dworkin, “Five-year outcomes in TMD: relationship of changes in pain to changes in physical and psychological variables,” Pain, Vol. 74, No. 2, pp. 315–326, Jan.
C. S. Greene, “Managing the care of patients with temporomandibular disorders,” The Journal of the American Dental Association, Vol. 141, No. 9, pp. 1086–1088, Sep. 2010.
F. Lobbezoo et al., “Consensus‐based clinical guidelines for ambulatory electromyography and contingent electrical stimulation in sleep bruxism,” Journal of Oral Rehabilitation, Vol. 47, No. 2, pp. 164–169, Sep. 2019.
E. R. Granger, “Occlusion in temporomandibular joint pain,” The Journal of the American Dental Association., Vol. 56, No. 5, pp. 659–664, 1958.
A. G. Pullinger and A. A. Monteiro, “History factors associated with symptoms of temporomandibular disorders,” Journal of Oral Rehabilitation, Vol. 15, No. 2, pp. 117–124, Mar. 1988.
H. Kjellberg, “Juvenile chronic arthritis. Dentofacial morphology, growth, mandibular function and orthodontic treatment,” Swedish Dental Journal. Supplement, Vol. 109, pp. 1–56, 1995.
G. Widmark, “On surgical intervention in the temporomandibular joint,” Swedish Dental Journal, Vol. 123, pp. 1–87, 1997.
H. Yatani, T. Kaneshima, T. Kuboki, A. Yoshimoto, Y. Matsuka, A. Yamashita “Long-term follow-up study on drop-out TMD patients with self-administered questionnaires,” Journal of Orofacial Pain, Vol. 11, No. 3, pp. 258–269, 1997.
D. J. DeNucci, C. Sobiski, R. A. Dionne, “Triazolam improves sleep but fails to alter pain in TMD patients,” Journal of Orofacial Pain, Vol. 12, No. 2, pp. 116–123, 1998.
H. Yatani, H. Minakuchi, Y. Matsuka, T. Fujisawa, A. Yamashita, “The long-term effect of occlusal therapy on self-administered treatment outcomes of TMD,” Journal of orofacial pain, Vol. 12, Issue 1, pp. 75–88, 1998.
P. C. R. Conti, L. R. De Azevedo, N. V. W. De Souza, and F. V. Ferreira, “Pain measurement in TMD patients: evaluation of precision and sensitivity of different scales,” Journal of Oral Rehabilitation, Vol. 28, No. 6, pp. 534–539, Jun. 2001.
T. Magnusson, A. M. Adiels, H. L. Nilsson, M. Helkimo, “Treatment effect on signs and symptoms of temporomandibular disorders-comparison between stabilization splint and a new type of splint (NTI). A pilot study,” Swedish Dental Journal, Vol. 28, No. 1, pp. 11–20, 2004.
P. A. Stee, “The Longevity of temporomandibular disorder improvements after active treatment modalities,” CRANIO, Vol. 22, No. 2, pp. 110–114, Apr. 2004.
D. Manfredini, M. Romagnoli, E. Cantini, and M. Bosco, “Efficacy of tizanidine hydrochloride in the treatment of myofascial face pain,” Minerva medica, Vol. 95, No. 2, pp. 165-171, 2004.
A. Anastassaki and T. Magnusson, “Patients referred to a specialist clinic because of suspected temporomandibular disorders: a survey of 3194 patients in respect of diagnoses, treatments, and treatment outcome,” Acta Odontologica Scandinavica, Vol. 62, No. 4, pp. 183–192, Jan. 2004.
P Cardelli, M Lattari, P Massaro, M Pollicita, A Barlattani, “Pharmacologic treatment of the dysfunctional patient”, Minerva Stomatologica, Vol. 54, No. 5, pp. 265–279, 2005.
L. LeResche, J. J. Sherman, K. Huggins, K. Saunders, L. A. Mancl, G. Lentz, S. F. Dworkin, “Musculoskeletal orofacial pain and other signs and symptoms of temporomandibular disorders during pregnancy: a prospective study”, Journal of Orofacial Pain, Vol. 19, No. 3, pp. 193–201, 2005.
J. A. Turner, L. Mancl, and L. A. Aaron, “Brief cognitive-behavioral therapy for temporomandibular disorder pain: Effects on daily electronic outcome and process measures,” Pain, Vol. 117, No. 3, pp. 377–387, Oct. 2005.
S. Wolfart et al., “Effects of prosthetic treatment for shortened dental arches on oral health-related quality of life, self-reports of pain and jaw disability: results from the pilot-phase of a randomized multicentre trial,” Journal of Oral Rehabilitation, Vol. 32, No. 11, pp. 815–822, Nov. 2005.
J. A. Turner, L. Mancl, and L. A. Aaron, “Short- and long-term efficacy of brief cognitive-behavioral therapy for patients with chronic temporomandibular disorder pain: A randomized, controlled trial,” Pain, Vol. 121, No. 3, pp. 181–194. 2006.
E. S. Furto, J. A. Cleland, J. M. Whitman, and K. A. Olson, “Manual physical therapy interventions and exercise for patients with temporomandibular disorders,” CRANIO®, Vol. 24, No. 4, pp. 283–291, Oct. 2006.
G. T. Clark, K. Baba, C. P. McCreary, “Predicting the outcome of a physical medicine treatment for temporomandibular disorder patients,” Journal of Orofacial Pain, Vol. 23, No. 3, pp. 221–229, 2009.
M. J. Fischer et al., “Do Occlusal Splints Have an Effect on Complex Regional Pain Syndrome? A Randomized, Controlled Proof-of-concept Trial,” The Clinical Journal of Pain, Vol. 24, No. 9, pp. 776–783, Nov. 2008.
M. Nilner, E. Ekberg, M. Doepel, J. Andersson, K. Selovuo, and Y. Le Bell, “Short-term effectiveness of a prefabricated occlusal appliance in patients with myofascial pain,” Journal of Orofacial Pain, Vol. 22, No. 3, pp. 209–218, 2008.
Erik Lindfors, Håkan Nilsson, Martti Helkimo, and Tomas Magnusson, “Treatment of temporomandibular disorders with a combination of hard acrylic stabilisation appliance and a soft appliance in the opposing jaw. A retro- and prospective study,” Swedish Dental Journal, Vol. 32, No. 1, pp. 9–16, 2008.
M. G. Piancino, L. Roberi, G. Frongia, M. Reverdito, R. Slavicek, and P. Bracco, “Computerized axiography in TMD patients before and after therapy with ‘function generating bites,’” Journal of Oral Rehabilitation, Vol. 35, No. 2, pp. 88–94, Jan. 2008.
H. Nilsson, D. Vallon, and E. C. Ekberg, “Long-term efficacy of resilient appliance therapy in TMD pain patients: a randomised, controlled trial,” Journal of Oral Rehabilitation, Vol. 38, No. 10, pp. 713–721, Mar. 2011.
F. Mongini, “O Sistema estomatognático. Função, disfunção e reabilitação,” (in Portuguese), Chicago, Quintessence Publishing Co., 1988.
H. Gelb, M. Gelb, “An orthopedic approach to the diagnosis and treatment of craniocervical mandibular disorders,” in New Concepts in Craniomandibular and Chronic Pain Management, London, Mosby-Wolfe, pp. 215-259, 1994.
C. G. Wheaton, “Mandibular rest position: relationship to occlusion, posture and muscle activity,” in New Concepts in Craniomandibular and Chronic Pain Management, London, Mosby-Wolfe, pp. 163–175, 1994.
J. P. Okeson, “Fundamentos De Oclusão E Desordens Temporo-Mandibulares,” (in Portuguese), São Paulo, 2th Ed., Artes Médicas, 1992.
M. D. Lerman, “A revised view of the dynamics, physiology, and treatment of occlusion: a new paradigm,” CRANIO®, Vol. 22, No. 1, pp. 50–63, Jan. 2004.
S. S. Linsen, H. Stark, and A. Matthia, “Changes in condylar position using different types of splints with and without a chinstrap: a case-control study,” CRANIO®, Vol. 30, No. 1, pp. 25–31, Jan. 2012.
C. Zuñiga et al., “Influence of variation in jaw posture on sternocleidomastoid and trapezius electromyographic activity,” CRANIO®, Vol. 13, No. 3, pp. 157–162, Jul. 1995.
R. Miralles et al., “Vertical dimension. Part 2: the changes in electrical activity of the cervical muscles upon varying the vertical dimension,” CRANIO®, Vol. 20, No. 1, pp. 39–47, Jan. 2002.
M. Leiva et al., “Effects of laterotrusive occlusal scheme and body position on bilateral sternocleidomastoid EMG activity,” CRANIO®, Vol. 21, No. 2, pp. 99–109, Apr. 2003.
R. Miralles et al., “Body position and jaw posture effects on supra- and infrahyoid electromyographic activity in humans,” CRANIO®, Vol. 24, No. 2, pp. 98–103, Apr. 2006.
R. Miralles et al., “Increase of the vertical occlusal dimension by means of a removable orthodontic appliance and its effect on craniocervical relationships and position of the cervical spine in children,” CRANIO®, Vol. 15, No. 3, pp. 221–228, Jul. 1997.
M. Kamisaka, H. Yatani, T. Kuboki, Y. Matsuka and H. Minakuchi, “Four-year longitudinal course of TMD symptoms in an adult population and the estimation of risk factors in relation to symptoms,” Journal of orofacial pain, Vol. 14, No. 3, pp. 224-232, 2000.
F. Mongini, “Headache and Facial Pain”, Nova York, Thieme, 1999.
D. Manfredini, L. Guarda-Nardini, E. Winocur, F. Piccotti, J. Ahlberg, and F. Lobbezoo, “Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings,” Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, Vol. 112, No. 4, pp. 453–462, Oct. 2011.
R. Ohrbach, “History and clinical examination”, in Temporomandibular joint and masticatory muscle desorders, St Louis, USA, Mosby, pp. 406–434, 1995.
P. Planas, “Rehabilitacion Neuro-Oclusal (RNO),” (in Spanish), 2th ed., Barcelona, España, Masson Salvat Odontologia, 1994.
Jr. O. Santiago, I. P. M. Santiago, “Atlas de Construção de Aparelhos Ortopédicos Funcionais,” (in Portuguese), Ribeirão Preto, Brazil, 1th Ed., 2010.
Jr. O. Santiago, “Dispositivo Ortopédico Funcional Dos Maxilares Para Desprogramação Mandibular e Aumento de Dimensão Vertical – Modelo de Uso Diurno Orlando Santiago System 1- OSS 1”, (in Portuguese), Patente apresentada ao Centro Universitário Hermínio Ometto – UNIARARAS, para obtenção do Título de Mestre em Odontologia, Área de Concentração em Ortodontia, 2010.
B. P. Moreira, “Dispositivo Ortopédico Funcional Dos Maxilares Para Avanço Mandibular E Aumento De Dimensão Vertical – Modelo De Uso Diurno Com Barra Ondulada Superior”, Orlando Santiago System 2”, (in Portuguese), Patente apresentada ao Centro Universitário Hermínio Ometto – UNIARARAS, para obtenção do título de mestre em Odontologia. Área de concetração em ortodontia, 2010.
G. Costa, “GNC Dispositiivo Ortopédico Funcional dos Maxilares Para Avanço Mandibular e Aumento de Dimensão Vertical – Modelo de uso Diurno com Aletas Inferiores – Orlando Santiago System 3”, (in Portuguese), Patente apresentada ao Centro Universitário Hermínio Ometto – UNIARARAS, para obtenção do título de mestre em Odontologia. Área de concetração em ortodontia, 2011.
Y. D. Fragoso, H. H. C. Alves, S. O. Garcia, and A. Finkelsztejn, “Prevalence of parafunctional habits and temporomandibular dysfunction symptoms in patients attending a tertiary headache clinic,” Arquivos de Neuro-Psiquiatria, Vol. 68, No. 3, pp. 377–380, Jun. 2010.
P. dos S. Calderon, M. de L. M. Tabaquim, L. C. de Oliveira, A. P. A. Camargo, T. de C. Ramos Netto, and P. C. R. Conti, “Effectiveness of cognitive-behavioral therapy and amitriptyline in patients with chronic temporomandibular disorders: a pilot study,” Brazilian Dental Journal, Vol. 22, No. 5, pp. 415–421, 2011.
A. Michelotti, G. Iodice, S. Vollaro, M. H. Steenks, and M. Farella, “Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles,” The Journal of the American Dental Association, Vol. 143, No. 1, pp. 47–53, Jan. 2012.
M.G. Piancino, S. Cirillo, G. Frongia, F. Cena, A.A. Bracco, P. Dalmasso, P. Bracco, “Sensitivity of magnetic resonance imaging and computed axiography in the diagnosis of temporomandibular joint disorders in a selected patient population,” The International Journal of Prosthodontics, Vol. 25, No. 2, pp. 120–126, 2012.
A. S. de Oliveira et al., “Impacto da dor na vida de portadores de disfunção temporomandibular,” Journal of Applied Oral Science, Vol. 11, No. 2, pp. 138–143, Jun. 2003.
M. C. Carra et al., “Prevalence and risk factors of sleep bruxism and wake-time tooth clenching in a 7- to 17-yr-old population,” European Journal of Oral Sciences, Vol. 119, No. 5, pp. 386–394, Aug. 2011.
L. Sonnesen, M. Bakke, and B. Solow, “Temporomandibular disorders in relation to craniofacial dimensions, head posture and bite force in children selected for orthodontic treatment,” The European Journal of Orthodontics, Vol. 23, No. 2, pp. 179–192, Apr. 2001.
E. Vrbanović, I. Lapić, D. Rogić, and I. Z. Alajbeg, “Changes in salivary oxidative status, salivary cortisol, and clinical symptoms in female patients with temporomandibular disorders during occlusal splint therapy: a 3-month follow up,” BMC Oral Health, Vol. 19, No. 1, Jun. 2019.
I. Z. Alajbeg, E. Vrbanović, I. Lapić, I. Alajbeg, and L. Vuletic, “Effect of occlusal splint on oxidative stress markers and psychological aspects of chronic temporomandibular pain: a randomized controlled trial,” Scientific Reports, Vol. 10, No. 1, Jul. 2020.
E. Vrbanović and I. Z. Alajbeg, “Long-term Effectiveness of Occlusal Splint Therapy Compared to Placebo in Patients with Chronic Temporomandibular Disorders,” Acta Stomatologica Croatica, Vol. 53, No. 3, pp. 195–206, Sep. 2019,
To continue learning and get access to all the other articles, log in or create an account
Or log in / create an account here:


