Treating Temporomandibular Disorders in the 21st Century: Can We Finally Eliminate the “Third Pathway”?
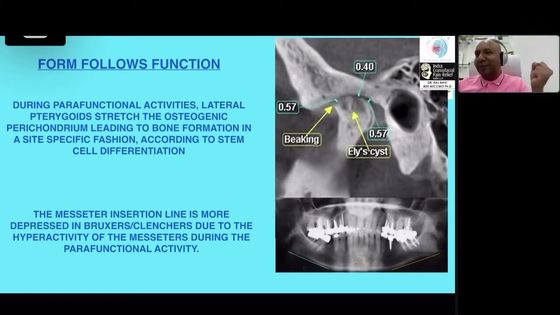
Within the orofacial pain discipline, the most common group of afflictions is temporomandibular disorders (TMD). The pathologic and functional disorders included in this condition closely resemble those that are seen in the orthopedic medicine branch of the medical profession, so it would be expected that the same principles of orthopedic diagnosis and treatment are applied. Traditional orthopedic therapy relies on a “Two Pathway” approach involving conservative and/or surgical treatments. However, over the course of the 20th century, some members of the dental community have created another way of approaching these disorders-referred to in this paper as the “Third Pathway”—based on the assumption that signs and symptoms of TMD are due to a “bad” relationship between the mandible and skull, leading to a variety of irreversible occlusal or surgical corrective treatments. Since no other human joint is discussed in these terms within the orthopedic medicine communities, it has become progressively clear that the Third Pathway is a unique and artificial conceptual creation of the dental profession.
However, many clinical studies have utilized the medically oriented conservative/surgical Two-Pathway model to diagnose and treat TMD within a biopsychosocial model of pain. These studies have shown that TMD comprise another domain of orthopedic illness that requires a medically oriented approach for good outcomes while avoiding the irreversible aspects of the Third Pathway. This review presents historical and current evidence that the Third Pathway is an example of unorthodox medicine that leads to unnecessary overtreatment and further proposes that it is time to abandon this approach as we move forward in the TMD field. J Oral Facial Pain Headache 2020;34:206–216. doi:10.11607/ofph.2608
Further details are accessible for you to learn about temporomandibular disorders management in our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
Here is one trend in dentistry of which every dentist must be aware:
The profession is growing ever closer to the medical profession in a variety of ways. The scientific basis for diagnostic and treatment procedures relies on the same fundamental biologic principles, and the clinical activities in both professions must be proposed and defended on that basis. Thus, within all undergraduate dental colleges around the world, dental students are receiving increasing exposure to medical information that will influence how their patients should be evaluated. Obviously, this leads to dental treatment protocols for each patient that must take such information into account.
The two postgraduate dental disciplines with the deepest and most sophisticated relationships with the medical profession are oral medicine and orofacial pain. Within the orofacial pain discipline, the most common group of afflictions is temporomandibular disorders (TMD), which are a diverse set of musculoskeletal conditions involving the temporomandibular joints (TMJs) and their related structures.1 This group closely resembles the pathologic and functional conditions commonly seen within the orthopedic medicine (OM) branch of the medical profession. Consequently, the principles of orthopedic diagnosis and treatment can be expected to play a significant role in the clinical management of TMD patients. However, unlike most other common orofacial pain conditions, TMD have been distinguished by a history of controversies going back nearly 100 years that continue to have a pernicious effect on the practice of caring for such patients.2,3
This paper discusses the traditional OM approaches to management of medical orthopedic problems, described as the “Two-Pathway” model, and then contrasts this approach with what is happening in some dental communities. In the Two-Pathway model, strategies to manage patients in the clinical setting belong to either a conservative or a surgical group of treatment.
The conservative medical approach incorporates many noninvasive modalities as well as many self-management strategies. Several different adjectives are used to describe the benign, reversible, and nonradical nature of these approaches, with some words that are merely descriptive and others that are more judgmental. The other approach is the surgical domain, where again a variety of procedures may be utilized (ranging all the way from various intracapsular interventions to total joint replacements), and, again, for which a variety of descriptive and judgmental adjectives are used. However, this is not a binary choice model, but rather a continuum or spectrum of possible clinical approaches to both diagnosis and treatment, with the utilization of many reasonable combinations of and compromises between these two approaches as medical practitioners deal with each individual case. However, when it comes to TMD, the dental profession has created another approach in which neither of these pathways plays much of a role.
That pathway, which will be referred as the “Third Pathway,” is based on three assumptions4–6:
The mandible-to-skull relationship at the condylar level may not be “good” (also described as misaligned, malpositioned, acquired, nonideal, suboptimal, etc).
This relationship can be analyzed by a variety of so-called “diagnostic” methods, ranging from pushing on the chin to measurements using sophisticated electronic devices.
If the existing jaw relationship is deemed to be “bad,” then it can be improved by a variety of irreversible dental techniques, ranging from occlusal adjustments to orthognathic surgery.
It should be pointed out that no other human joint is discussed in these terms within the OM medical community. No physician questions whether your knee or shoulder is in the right place or correctly aligned, or whether the femur of your hip is properly seated in its acetabulum. Moreover, there are no specific OM treatment protocols designed to permanently reposition any other joints into some kind of “better” relationship. Therefore, it is clear that this Third Pathway is a unique and artificial conceptual creation arising from the dental profession based on a biologic and mechanical viewpoint that deserves to be challenged. The authors intend to show, by reviewing the available evidence, that this is indeed the case, and further intend to argue that it is time to abandon this approach as we move forward in the TMD field.
Why Did the Dental Profession Create a Third Pathway?
Establishing a Diagnosis. Since no other branch of the medical profession has proposed a malpositioning-repositioning approach to diagnosing or treating other human joint disorders, it would be expected that the TMJ has some unique features that make it possible, and even attractive, to analyze TMD patients in such a framework. The most obvious anatomical feature is the fact that no other joint has a definitive stopping mechanism external to the joint structures that requires the joint to move into a specific position upon “seating” of the opposing parts.
This “stop” occurs when the maxillary and mandibular teeth (which are located several inches away from the TMJs) meet in maximum intercuspation (MIP). In healthy dentate patents, teeth meet in a precise and repeatable manner, and this event will determine with great precision and repeatability where the mandibular condyle will end up relative to the skull when the mouth is fully closed.
Therefore, when patients began to report to their 20th century dentists that they were having symptoms involving the TMJ region, it was not entirely unreasonable to hypothesize that their joints and muscles were not comfortable due to some malalignment of the dental occlusion. Oddly enough, this kind of thinking arose more from the early work of an otolaryngologist named Costen than from any dental experts.
Costen observed that many patients who reported facial pain in his practice were either partially or fully edentulous and thought that mandibular overclosure was the reason for developing symptoms.7 Subsequent occlusal and skeletal disharmony theories proposed by many dental clinicians were mostly variations on this theme, with the macro-overclosure replaced by a variety of mini-disharmonies (occlusal interferences, deep bites, crossbites, etc). Many narrative and systematic reviews over the past decade have commented on this topic.8–10
Because both occlusal relationships and TMJ relationships could be tentatively measured using many clinical techniques, this kind of mechanistic thinking inevitably led to a variety of analytic procedures, ranging from simple chin manipulations to complex kinesiographic recordings. For instance, radiographs of the TMJ could be measured for concentricity of the condyle-fossa relationship, or articulators could be used to provide a bench-top view of the occlusal relationships based on various methods of recording.
These approaches were proposed for diagnostic purposes despite the fact that no baseline values or normality ranges existed for determining what a “good” or “bad” condyle position ought to be, while ignoring the fact that TMJ functional anatomy cannot be reproduced by articulators. All of these measurement and evaluation systems had a built-in bias about what was biologically acceptable so that clinicians could render judgements about their findings in several ways.
Treatments Based on Diagnosis. Once the idea was accepted that some “negative” features of a patient’s MIP could be a major etiologic factor in the development of a TMD condition, it was then logical to utilize various dental techniques and procedures to “correct” that relationship.11 Of course, this also meant that the original TMJ position would now be permanently altered. In some cases, this irreversible approach was the only treatment provided, with no preceding attempts to relieve pain, reduce inflammation, or relax sore muscles. Some other clinicians preferred to begin their TMD treatment with various conservative measures (such as medications, physical therapy, home care, etc) to relieve symptoms and to identify a purported “ideal” mandible position before initiating any irreversible treatment. This approach became known as the Phase 1–Phase 2 method and included a wide variety of treatment procedures. Approaches (with or without a Phase 1) led to irreversible modifications to the dentition; for example, as soon as the initial diagnosis was “established,” a complete occlusal adjustment (equilibration) could be performed, a complete orthodontic correction could be initiated, or a complete full-mouth reconstruction could be carried out.
However, the most commonly used treatment modality in this mechanistic framework was the oral appliance (splint) approach because it was argued that the response to such treatment would determine what subsequent steps must be taken. These appliances were variously described as jaw muscle relaxers, deprogrammers, joint unloaders, bite openers for establishing a new vertical dimension of occlusion (VDO), and other labels based on the personal concepts of each clinician. Since the MIP in all of these procedures was being temporarily altered by wearing a splint, any positive responses in terms of symptomatic improvement were seen as indicators of (1) the validity of the initial diagnostic and etiologic theory, and (2) the need for making permanent changes in jaw position based on the new occlusal/jaw relationship.
In short, the entire conceptual framework of the Third Pathway was based on circular reasoning with self-referenced treatment theories based on the interpretation of “diagnostic findings” produced using various unproven diagnostic procedures and protocols.
What Does the Literature Say About the Third Pathway?
Throughout most of the 20th century, the dental literature has described the above procedures in terms of clinical concepts and protocols rather than by presenting controlled clinical trials and studies. Scorecards of successful case outcomes were a frequent feature of such papers. For most of that century, the focus was on myogenous and arthrogenous pain conditions, with little or no attention paid to the articular disc. Near the end of that century, attention shifted more to the topic of TMJ disc displacements, and articles began to focus on how to treat these conditions. For the sake of brevity, this article will not cite or summarize the hundreds of old case reports and anecdotal papers dealing with early uses of splints and jaw repositioning methods as described in the above section for treating muscle and joint pain. Instead, the focus of this literature review was on one specific corner of the TMD universe, the Third Pathway approach to recapturing anteriorly displaced discs, in order to demonstrate how this model has influenced clinical practice in the TMD field.
With this objective in mind, a systematic search was performed in the Medline database on June 4, 2019, to identify clinical trials that compared the treatment effectiveness of permanent mandible repositioning (MR) strategies to any other treatment modalities for patients with TMJ disc displacement.
Out of more than 18,000 results retrieved with the keyword “temporomandibular disorders,” 172 articles remained after combining that keyword with “jaw repositioning.” Of these, 157 papers were left after limiting the search to clinical trials, but even the 15 remaining articles were not specifically designed to address the topic of mandible repositioning for TMD purposes.
In general, studies on repositioning strategies are limited to early papers on the use of anterior repositioning (AR) appliances that aim to recapture the disc and improve symptoms in patients having disc displacement with reduction.12–15 Some investigations have reported that joint sounds can be reduced more with AR appliances than flat appliances, which is an implicitly obvious finding based on the rationale of using AR to place the condyle under the displaced disc. However, no literature is available that confirms the long-term superiority of any definitive disc-repositioning strategies in comparison to conservative approaches for pain management in such cases.
Over 30 years ago, some authors suggested that AR strategies failed to take into account the tri-dimensional features of the joint while also ignoring the fact that factors other than disc position contribute to pain symptoms.16,17 In addition, the progressive increase in knowledge regarding the natural course of TMJ clicks has shown that most do not progress to a more serious TMJ disorder. Together with the emerging observations that disc displacement is frequently accompanied by adaptive morphologic changes (especially in the retrodiscal tissues), this has dismantled the rationale for targeting treatment toward disc recapture, thus diminishing the potential indications for the use of AR appliances.
In summary, the findings from the literature reviewed in this search can be summarized as follows:
Early reports of positive outcomes regarding the effectiveness of MR reflect a misunderstanding regarding the treatment targets of pain reduction and avoiding development of joint degenerative changes. Ultimately, the important studies on these phenomena show that recapturing the TMJ disc is not necessary to reduce pain, reduce future degenerative joint disease problems, or establish a definitive stability of the disc position.
In the short term, there are some clinical suggestions that AR appliances may be superior to flat appliances in providing pain relief in patients having disc displacement with reduction.
It is biologically plausible that this outcome has more to do with capsular distension and load change than any actual improvement in condylar position or disc-condyle relationships, thus making permanent condylar repositioning again not recommendable.
Well-controlled comparative studies have never been performed over the years to see if one group (ie, a group treated with conservative therapies) shows better or worse outcomes than another group undergoing MR treatments.
There have been prospective studies to determine whether presymptomatic dental procedures (equilibration, orthodontics, orthognathic surgery, bite opening, etc) would prevent later onset of TMD conditions, and the outcome evidence is almost entirely negative for such studies.
Thus, the available evidence suggests that the Third Pathway approach for TMJ repositioning has not been proven necessary for treating either simple muscle or joint TMD problems, nor for the long-term treatment of displaced disc conditions (ie, disc recapture), even after decades of practice. In the absence of such evidence, it seems reasonable instead to discuss the possible clinical usefulness of the Third Pathway by appraising it in terms of medical necessity and biologic plausibility.
Medical Necessity and Biologic Plausibility
If the Third Pathway, which relies on analyzing TMJ relationships and repositioning the mandible, is truly valid and worthwhile as a treatment approach for TMD signs and symptoms, it should meet the criteria for being medically necessary and biologically plausible for some or all of the patients suffering from these conditions—in other words, it should be possi-lble to demonstrate through clinical research that this approach is not only biologically plausible, but also that it produces positive results for some or all TMD patients that cannot be achieved by other means.
This section will consider whether that evidence has been produced.
A recent paper by Greene and Obrez has raised lthe question of medical necessity directly in its title: “Treating Temporomandibular Disorders with Permanent Mandibular Repositioning: Is It Medically Necessary?”18 The article discussed six criteria for medical necessity and concluded that the concept of mandibular repositioning did not sufficiently satisfy any of them:
The medical condition (ie, mandibular malpositioning) is generally not recognized as a valid health problem or disease.
The diagnostic tests used to assess whether the patient has this condition are not valid with acceptable specificity and sensitivity.
The patient’s condition will not get worse unless a specific Third Pathway procedure is done.
The clinical procedures required for MR do not have specificity for addressing the patient’s particular problem (eg, symptoms of TMD).
The procedures are not clinically efficacious for managing TMD problems according to evidence-based criteria (ie, they could be effective due to other reasons, such as placebo effects or natural fluctuations).
It has not been demonstrated that most TMD cannot be generally resolved by performing less invasive procedures that do potentially have high benefit-to-risk ratios.
One might think that well-controlled comparative studies would have been performed over the years to assess whether a group of TMD patients treated with conservative therapies shows better or worse outcomes than another group provided with MR treatment. However, no such side-by-side study has ever been published, and it is doubtful that an institutional review board from any academic institution would approve such a study today in light of current knowledge.
However, it bears reminding that the paper by Greene and Obrez does not rule out the possibility that some patients may need major occlusal modifications for a variety of dental reasons. Every patient who undergoes orthodontic or reconstructive dental treatment will have both a new TMJ position and new occlusal relationships established as a routine component of these complex processes.
In addition, a person who has had a severe form of degenerative TMJ arthritis (eg, juvenile rheumatoid arthritis, idiopathic condylar resorption) will certainly need to have a new occlusion established once the primary disease is under control. However, none of these scenarios are related to the common arthrogenous or myogenous forms of TMD, so they should be discussed under the rubric of conventional dentistry.
Are There Subgroups of TMD Patients Who May Need Third Pathway Treatment?
Because TMD are a heterogenous group of clinical problems, there is no single treatment protocol for managing all types of patients, especially considering the well-known complex interface between Axis I (ie, muscle or joint disorders) and Axis II (ie, psychosocial issues) findings.19,20 This reality has been well recognized in the 21st century literature on these topics. Publications like the Diagnostic Criteria for TMD (DC/TMD), the American Association of Orofacial Pain (AAOP) Guidelines, the American Association of Oral and Maxillofacial Surgeons (AAOMS) Parameters of Care, and the European Academy of Orofacial Pain and Dysfunction (EAOPD) recommendations provide much information to clinicians about how to deal with this variety of clinical challenges.21–24 None of these guideline documents advocate the Third Pathway approach as discussed in this paper.
Nonetheless, it seems appropriate to ask the question: Is there a subgroup of TMD patients who might have a malpositioned condyle-fossa relationship who would then benefit from the Third Pathway approach to treatment? One way of providing an answer would be to compile a list of subjective symp-ltoms that would indicate the need for MR treatment, but until now, no reputable group of researchers or clinicians has produced such a list. A different picture emerges, however, when discussing so-called objective signs and findings. For example, manipulation of the mandible might produce a finding of centric relation (CR) that does not coincide with the MIP of the patient’s teeth. This is usually is described as a CR-MIP discrepancy, and the difference is called a “slide.” Similarly, electronic “diagnostic” machines may find a discrepancy between “neuromuscular” CR and MIP, while radiographic images may show a condylar position that looks “wrong.” Likewise, a deprogramming splint may produce muscular responses that allow the condyles to wander somewhere further backward or forward from their original position. It must be kept in mind, however, that all of these findings are self-referential, which means that they are based on the original assumptions that led the clinician to make that type of assessment in the first place. Thus, it is not surprising that there is a complete absence of literature in support of those theories.25–29 Therefore, this type of circular logic cannot be cited as proof that the patient has a malpositioned TMJ and will require irreversible occlusal changes to correct it.
Another common argument to support the need for MR comes from positive responses to oral appliance (OA) therapy. As early as the 1970s, Ramfjord and Ash were claiming that successful OA therapy proved that the occlusion was the original cause for developing a TMD condition and that this proof was sufficient to justify irreversible equilibration and restorative procedures.30 Similar arguments have been made for bite-opening appliances used in patients who were presumed to have loss of VDO (or “bite collapse”) and therefore would need to have bite-opening occlusal work if their symptoms improved with OA treatment. It was not until the last third of the 20th century that researchers began to demonstrate that positive responses to OA therapy did not require a second phase of irreversible dental treatment.31–34 As a result, the idea of considering OAs to be valuable primarily as symptom-relieving orthotic devices has become widely accepted and remains the standard rationale among TMD experts today.35,36
Finally, there is the argument presented by some lthat failure to respond to currently recommended conservative TMD treatments provided within a biopsychosocial framework could be the justification for “escalating” to the more aggressive forms of TMD treatment. The general concept of escalating from conservative treatment protocols to more aggressive ones is well-accepted in many areas of the normal Two-Pathway system of medical practice, but it cannot be applied to every type of medical condition—for example, there are almost no examples of headache conditions that would be improved or eliminated by some kind of surgery, no matter how poorly the patient is responding to standard medical approaches.
On the other hand, the orthopedic field contains many examples of legitimate escalation from conservative treatment to a variety of more aggressive treatments. However, this applies almost entirely to arthrogenous conditions or to spinal disc and nerve conditions (in back and neck pain problems), not to most common myogenous disorders. As for the TMJ, surgery can be a first-choice approach that is indicated for select joint disorders rather than a second-step, unspecific attempt to provide pain re-lief.37–39 However, failure to respond to a variety of well-conducted clinical procedures (eg, medications, physical therapy, self-care, or OA) for treating both arthrogenous and myogenous conditions is not rare in TMD pain patients. When symptoms of myogenous origin (both local types and general conditions, such as fibromyalgia) are the main problem, there is no surgical option available to use as an “escalation” for treating those patients.
Unfortunately, the Third Pathway offers dentists an alternative for analyzing and treating TMD patients who are not responding to currently recommended conservative treatment protocols, regardless of whether their problems are arthrogenous or myogenous. Given the arguments presented above about the general validity of this Third Pathway, this must be considered as an example of unorthodox medicine rather than an example of true escalation. Because the use of Third Pathway treatments is still widely advocated, the possible side effects and negative consequences of that approach must be discussed next.
What Are the Risks of Third Pathway Treatment Procedures?
It is difficult to imagine that any set of irreversible treatment protocols would not carry some risk with them. In medical circles, these are referred to as risk/benefit ratios, and it often can be argued that the potential benefits will most likely outweigh the risks. In many cases, a specific medical problem may require the use of irreversible therapies, and the risks will simply have to be explained to the patient as part of the informed consent process.
So, the question is: Where does the Third Pathway approach, as described in this paper, fall on that risk/benefit spectrum? Given the weak evidence for this approach and the existence of more conservative and traditional treatments for managing TMD, the following list of outcomes should be seriously considered. Because each of them has been discussed extensively in the dental literature, they will only be briefly described here:
Development of occlusal awareness/dysesthesia/hypervigilance is not uncommon in patients who have undergone extensive locclusion-changing procedures, regardless of whether they were for routine dental processes—such as orthodontics or full-mouth reconstruction—or for treating TMD. Despite the fact that there is no guaranteed way to reestablish the original occlusion, such patients often become obsessive about pursuing various kinds of occlusal treatment.40–42
Surgical or occlusal treatments to reposition the mandible may be attempted in patients who primarily have either myogenous TMD or some other form of orofacial pain referred to the TMJ area. This will usually produce not only a failure to improve, but also a likelihood of worsening the entire facial pain situation.43
There is a tendency for peripheral pain problems to become central sensitization problems over time. Delays in providing appropriate treatment or wasting time and resources on a Third Pathway approach will often lead to this kind of negative outcome. This can lead to chronification of pain, which is one of the greatest challenges faced by all clinicians treating pain. Predictors for that outcome are limited, but it is known that, among other things, misdiagnosis, undertreatment, delays in treatment, failure to address psychologic impairment, and multiple invasive treatments enhance the risk of chronic pain development.44,45 Since Third Pathway treatments are usually carried out over a fairly long time, this adds to their potential for increasing this risk.
Many patients have reported a worsening of their pain due to the bite-changing and jaw-repositioning aspects of Third Pathway treatment.46,47 This kind of secondary complication will likely make it even more difficult to resolve the clinical situation.
Orofacial pain experts who work in university and hospital clinics around the world have reported seeing all of these above phenomena in their patient populations. Because they often function as tertiary care centers, they probably see more of these negative scenarios than any normal dental practice would encounter.
Why Does the Third Pathway Continue to be Widely Used in the TMD Field?
In spite of the lack of scientific support, concepts and treatments based on the Third Pathway have not yet been fully abandoned in orofacial pain medicine. On the contrary, they are still widely accepted and utilized clinically by many members of the dental community. There are at least six reasons for this paradoxical situation: (1) the type of disease; (2) history of early concepts; (3) cultural beliefs; (4) social reasons; (5) the market of self-proclaimed experts; and (6) financial issues.
Type of Disease. As discussed in the above sections on diagnosis and treatment, signs and symptoms of TMD are typically fluctuating and mostly self-limiting, as in the case of many other musculoskeletal conditions.48–51 Within the Two Pathway model, treatment is mainly provided in the form of symptomatic management, and there is much overlap among many of the treatment approaches directed toward TMJ or muscle pain relief.52 For arthrogenous pain, dysfunction, and disease, however, TMJ arthrocentesis and surgery are two examples of specific treatment modalities.53 Many TMD patients improve regardless of the specific treatment approach, while a minority of patients progress toward chronicity or persistence of symptoms in a way that suggests they are vulnerable to a poor response to any intervention. Recent studies suggest that there are some predictive factors to explain such outcomes, but they are difficult to identify early in the clinical situation.54–56
This means that, at least to a certain extent, treatment outcome is achieved “by chance”; ie, independent of the putative causal reasons.57 This has important implications for Third-Pathway approaches that require irreversible changes of dental occlusion and condyle positioning within the TMJ fossa because they are based on the false premise that such treatment is indicated if the patient responded well to the initial reversible treatment. When clinical improvement is produced by this Phase 1–Phase 2 approach, both the dentist and patient may be persuaded that the entire treatment package was both necessary and responsible for the positive outcome. Such paradoxes are well known to expert TMD and orofacial pain practitioners. The majority of currently recommended treatments share several common objectives: in the physical domain, there is a focus on restoration of jaw function, achievement of dental and orthopedic stability, and relief from pain.
In the psychosocial domain, improvement in quality of life, reduction in psychologic distress, and improvement in pain-related impairment are fundamental targets independent of the Axis I diagnosis. Due to the generally benign natural course and good remission with mild self-care regimens, symptomatic improvement can be partially attributed to the familiar “regression to the mean”; ie, the tendency for severe initial symptoms to get better over time.58 Such observations are supported in part by seeing “waiting-list” patients improving during certain clinical trials despite not yet receiving any treatment.
Moreover, recent neurophysiologic advances have given the placebo effect the deserved dignity of being recognized as an active treatment, the positive effects of which are related to the patient’s expectations and go far beyond the simple psychologic effect on the patient’s attitude toward the disease.59,60
At present, there are no instruments to predict the profiles of placebo responders, but one might hypothesize that subjects with high levels of psychologic distress and certain personality profiles as seen in many chronic TMD patients may be candidates for a good placebo response.
The average practitioner is used to fixing problems and to performing inductive reasoning (ie, “I do this, it works, so I build a hypothesis of action”), without any deductive strategy (ie, “I build a hypothesis of action, and I will test it with comparative trials”). Deductive approaches are the modus operandi of clinical researchers, who are too often negatively described as “messengers living in ivory towers.” Remarkably, this bias occurs despite their extensive clinical expertise and their evidence-based pleas for general dentists to think as a physiatrist or a neurologist when dealing with TMD and orofacial pain patients.
History of Early TMJ Concepts. Unfortunately, the impact of the original Costen theory of mandibular overclosure and jaw malpositioning is still alive and well 85 years after its proposal. It is not infrequent for an orofacial pain expert to receive patients who are referred by some general physicians or other nondental professionals because of the presence of Costen’s syndrome. This is not just an old name for a disease, but a concept that survives in many medical and allied health schools, where very limited information on TMD is often provided. As for the dental profession itself, the figure of the “gnathologist” as the dental professional who takes care of jaw dys-function by correcting mechanical problems in the teeth-to-mandible position is a myth that should be past its time.61
Today, stomatognathic physiology is a much broader field than the classical gnathologic view of mechanical concepts of CR and cast mounting on articulators for diagnosing purported dysfunction.
Based on that, it is recommendable that international academies and recognized experts/board members must attempt to increase cross-specialist knowledge on this issue. This is already occurring in various national and international pain groups (eg, the International Association for the Study of Pain [IASP], International Association for Dental Research/International Network for Orofacial Pain and Related Disorders Methodology [IADR/INfORM]), but not within most dental specialties or in other disciplines.
Cultural Beliefs. A side effect of this historical heritage is the widespread cultural belief that pain in the face depends on something being wrong in the teeth-to-mandible position and other similar mechanical theories. As a result, the vast majority of patients seeking TMD advice still believe they have some kind of mandibular malpositioning or teeth misalignment.
Patient forums on the internet, and even associations of people having TMD symptoms, have been created to share experiences and find reciprocal support while searching for the best advice on how to find the right dentist to fix their own mandible position.
Social Issues. A possible reason for some patients to keep believing in the Third Pathway is that sometimes people are afraid of admitting emotional and psychologic issues. It is not rare that a patient with TMD pain due to stress sensitivity–related muscle tension prefers to give credit to some mechanical theory instead of discussing inner issues. The fact that many patients with chronic pain often present with a complex medical history, in addition to the presence of comorbid conditions (eg, headache, irritable bowel syndrome, gastritis, dysmenorrhea, affective disorders), further complicates their interaction with the dentist.62,63 Therefore, instead of discussing such issues with their dentist—which could create a fundamental therapeutic partnership by sharing responsibilities with the caregiver64—those patients may tend to see the dentist only as the professional figure who must find a mechanical solution to fix the problem.
Market of Self-Proclaimed Experts. The current era of dental practice is characterized by a positive interchange of knowledge among professionals with different expertise. In many countries, the main academies organize yearly multidisciplinary events to facilitate communications among experts and provide better management of patients in the clinical setting.
For instance, orthodontists can frequently attend orthodontic symposia or congresses with qualified experts lecturing on how to manage the periodontium with orthodontic forces, how to understand the surgical difficulties of creating enough space to place implants, or how to evaluate prosthodontic needs to realize esthetic success after an orthodontic treatment. Such strategies are effective ways of creating a virtuous circle to improve the quality of the profession, and, generally speaking, the presentations meet high standards of quality. It is hard to imagine a periodontist speaking in front of an important ortho audience and giving “personal” information not in line with the recognized periodontal academies.
Unfortunately, the situation is quite different when it comes to “expert” speakers on TMD presenting at various congresses or meetings. An audience of dentists may be exposed to some excellent and current concepts by certain speakers, while others may be exposed to outdated and very personalized theories. Similarly, at the same congress where dentists can listen to top-tier periodontists or prosthodontists, they also may be offered a debate on occlusion and TMD, with a series of anecdotal claims by professionals without any certified education in TMD and/or orofacial pain. This makes it even more fundamental for the orofacial pain academies to organize events and educational activities of clinical interest for general dentists.
Financial Issues. For years, the TMJ has been jokingly referred to as “the money joint.” Self-proclaimed experts have organized courses on occlusal dogmas and have sold Third Pathway treatments that can produce thousands of dollars/euros for the dentists who follow their teachings. In addition, there are many academies, institutes, and study clubs that exist to promote Third Pathway approaches to TMD management.
This attitude is not likely to change in the near future, especially given the five other reasons of Third Pathway survival listed above. However, it would be interesting to see a future detailed discussion based on the emerging concepts of dental marketing and productivity. Indeed, there could be arguments presented in support of the idea that providing current TMD standard-of-care treatments (ie, conservative approaches) may be even more productive in terms of net income than correcting dental occlusion. Despite the large amount of money that a full-mouth restoration approach based on the Third Pathway can generate, an analysis of costs (eg, lab technicians, materials, staff, total time needed [cost per hour]) would be interesting to assess the real financial advantage of following the Third Pathway.
For instance, marketing analysis could assess the effectiveness of TMD clinics providing an ideal care regimen based on a simple flat appliance delivery plus three to five 30-minute cognitive behavioral therapy sessions by comparing this protocol to Third Pathway clinics spending years of unnecessary time for each patient. At present, country-to-country differences in terms of insurance markets make it difficult to provide a global picture, but any possible efforts on this delicate issue could reveal information that may contribute to discouraging irreversible approaches.
There are additional details about temporomandibular disorders that you can discover in our course "Evidence-based treatment of TMJ dysfunction".
Conclusions
In this paper, the term “Third Pathway” was introduced as a shorthand label for the early traditional method of managing TMD, which of course is still strongly persisting in the profession. That method includes diagnostic assessments of occlusal, skeletal, and TMJ relationships as likely factors in the etiologies of various TMD conditions, leading to a variety of bite-changing and jaw-repositioning therapies. It is based on concepts and procedures that are unique to the dental profession and the TMJ because no other branch of orthopedic medicine utilizes such assessments or treatments for other body joints.
Over the past 50 years, however, that concept has been challenged from two different directions. First, there have been many studies questioning the validity or utility of these so-called “diagnostic” findings (eg, “good” or “bad” occlusal or joint relationships). These studies have led to concerns about the medical necessity of performing the irreversible dental treatment procedures that are commonly done. Second, a separate line of research has emerged in which investigators have totally ignored the Third Pathway and instead utilized the medically oriented conservative/surgical treatment model (Two-Pathway approach) to diagnose and treat TMD. This approach also included incorporation of the biopsychosocial model to understand the behavioral aspects and impacts of chronic pain problems. Thus, the dental and medical professions began to converge on the issues surrounding the management of TMD as another orthopedic pain management area that requires a medically oriented approach for good outcomes while avoiding the irreversible aspects of the Third Pathway. Given recent discoveries about genetic susceptibility factors and comorbidity of pain disorders, this convergence has proven to be most appropriate.
Therefore, as we enter the third decade of the 21st century, the evidence provided in this paper and so many others should be sufficient to argue for abandonment of the Third Pathway (Table 1). The fact that it is a model leading to irreversible treatment procedures requires that it must be both theoretically sound and clinically effective. The authors believe that this burden of proof cannot be met and that the more conservative Two Pathway system has sufficient evidence to justify its routine use in dental practice. For those who wish to argue the opposite viewpoint, the burden of proof to overcome this powerful evidence lies with them.
Table 1 Summary of Main Arguments and Reasons for Abandoning the Third Pathway in the Management of TMD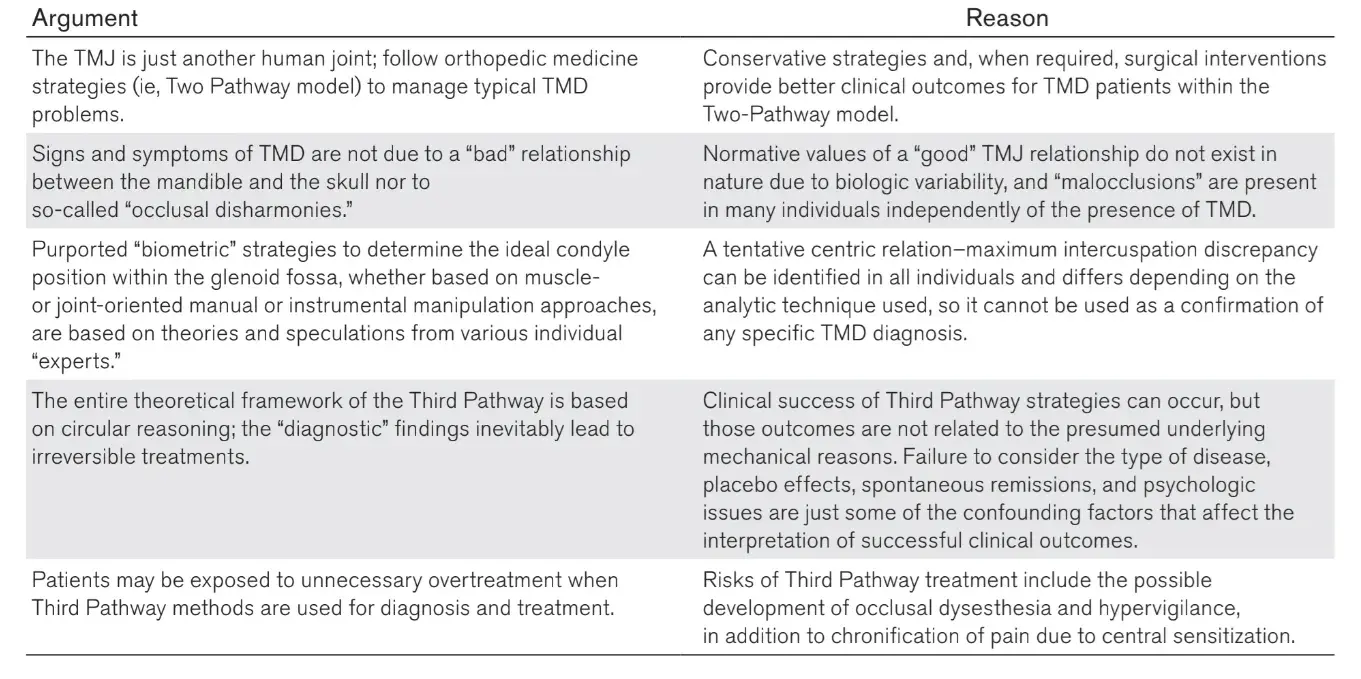
Acknowledgments
The authors did not receive any funding to prepare this manuscript. The authors declare they have no conflicts of interest.
References
Schiffman E, Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J Am Dent Assoc 2016;147:438–445.
Laskin DM, Renapurkar SK. Current controversies in the management of temporomandibular disorders. Oral Maxillofac Surg Clin North Am 2018;30:xiii.
McNeill C. Management of temporomandibular disorders: Concepts and controversies. J Prosthet Dent 1997;77:510–522.
Friedman MH. Therapeutic condylar repositioning: Fact or fancy? Quintessence Int 1985;16:195–199.
Piehslinger E, Celar A, Celar R, Jäger W, Slavicek R. Reproducibility of the condylar reference position. J Orofac Pain 1993;7:68–75.
Weinberg LA. Definitive prosthodontic therapy for TMJ patients. Part I: Anterior and posterior condylar displacement. J Prosthet Dent 1983;50:544–557.
Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol 1934;43:1–15.
Manfredini D, Lombardo L, Siciliani G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: End of an era? J Oral Rehabil 2017;44:908–923.
Türp JC, Schindler H. The dental occlusion as a suspected cause for TMDs: Epidemiological and etiological considerations. J Oral Rehabil 2012;39:502–512.
Rinchuse DJ, Kandasamy S. Myths of orthodontic gnathology. Am J Orthod Dentofacial Orthop 2009;136:322–330.
Manfredini D. Occlusal equilibration for the management of temporomandibular disorders. Oral Maxillofac Surg Clin North Am 2018;30:257–264.
Lundh H, Westesson PL, Jisander S, Eriksson L. Disk-repositioning onlays in the treatment of temporomandibular joint disk displacement: Comparison with a flat occlusal splint and with no treatment. Oral Surg Oral Med Oral Pathol 1988;66:155–162.
Westesson PL, Lundh H. Temporomandibular joint disk displacement: Arthrographic and tomographic follow-up after 6 months’ treatment with disk-repositioning onlays. Oral Surg Oral Med Oral Pathol 1988;66:271–278.
Okeson JP. Long-term treatment of disk-interference disorders of the temporomandibular joint with anterior repositioning occlusal splints. J Prosthet Dent 1988;60:611–616.
Anderson GC, Schulte JK, Goodkind RJ. Comparative study of two treatment methods for internal derangement of the temporomandibular joint. J Prosthet Dent 1985;53:392–397.
Greene CS. A critique of nonconventional treatment concepts and procedures for TMJ disorders. Compend Contin Educ Dent 1984;5:848–851,854.
Zamburlini I, Austin D. Long-term results of appliance therapies in anterior disk displacement with reduction: A review of the literature. Cranio 1991;9:361–368.
Greene CS, Obrez A. Treating temporomandibular disorders with permanent mandibular repositioning: Is it medically necessary? Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:489–498.
Manfredini D, Ahlberg J, Winocur E, Guarda-Nardini L, Lobbezoo F. Correlation of RDC/TMD axis I diagnoses and axis II pain-related disability. A multicenter study. Clin Oral Investig 2011;15:749–756.
Ohrbach R, Dworkin SF. The evolution of TMD diagnosis: Past, present, future. J Dent Res 2016;95:1093–1101.
Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 2014;28:6–27.
De Leeuw R, Klasser GD. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management, ed 6. Chicago: Quintessence, 2018.
American Association of Oral and Maxillofacial Surgeons. Parameters of Care: Clinical Practice Guidelines for Oral and Maxillofacial Surgery (AAOMS ParCare 2017), Sixth Edition. Rosemont, IL: AAOMS, 2017.
De Boever JA, Nilner M, Orthlieb JD, Steenks MH; Educational Committee of the European Academy of Craniomandibular Disorders. Recommendations by the EACD for examination, diagnosis, and management of patients with temporomandibular disorders and orofacial pain by the general dental practitioner. J Orofac Pain 2008;22:268–278.
Rinchuse DJ, Kandasamy S. Centric relation: A historical and contemporary orthodontic perspective. J Am Dent Assoc 2006;137:494–501.
Türp JC, Schlenker A, Schröder J, Essig M, Schmitter M. Disk displacement, eccentric condylar position, osteoarthrosis-Misnomers for variations of normality? Results and interpretations from an MRI study in two age cohorts. BMC Oral Health 2016;16:124.
Lelis ÉR, Guimarães Henriques JC, Tavares M, de Mendonça MR, Fernandes Neto AJ, Almeida Gde A. Cone-beam tomography assessment of the condylar position in asymptomatic and symptomatic young individuals. J Prosthet Dent 2015;114:420–425.
Vozzi F, Favero L, Peretta R, Guarda-Nardini L, Cocilovo F, Manfredini D. Indexes of jaw muscle function in asymptomatic individuals with different occlusal features. Clin Exp Dent Res 2018;4:263–267.
Manfredini D, Cocilovo F, Favero L, Ferronato G, Tonello S, Guarda-Nardini L. Surface electromyography of jaw muscles and kinesiographic recordings: Diagnostic accuracy for myofascial pain. J Oral Rehabil 2011;38:791–799.
Ramfjord SP, Ash MM. Occlusion, ed 2. Philadelphia: W.B. Saunders, 1971.
Greene CS, Laskin DM. Splint therapy for the myofascial pain—Dysfunction (MPD) syndrome: A comparative study. J Am Dent Assoc 1972;84:624–628.
Goodman P, Greene CS, Laskin DM. Response of patients with myofascial pain-dysfunction syndrome to mock equilibration. J Am Dent Assoc 1976;92:755–758.
Dahlström L, Carlsson GE, Carlsson SG. Comparison of effects of electromyographic biofeedback and occlusal splint therapy on mandibular dysfunction. Scand J Dent Res 1982; 90:151–156.
Okeson JP, Moody PM, Kemper JT, Calhoun TC. Evaluation of occlusal splint therapy. J Craniomandibular Pract 1983;1: 47–52.
Greene CS, Menchel HF. The use of oral appliances in the management of temporomandibular disorders. Oral Maxillofac Surg Clin North Am 2018;30:265–277.
Dao TT, Lavigne GJ. Oral splints: The crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med 1998;9:345–361.
Dimitroulis G. Temporomandibular joint surgery: What does it mean to the dental practitioner? Aust Dent J 2011;56:257–264.
Koslin MG, Indresano AT, Mercuri LG. Temporomandibular joint surgery. J Oral Maxillofac Surg 2012;70(11 suppl 3): e204–e231.
Dolwick MF. Temporomandibular joint surgery for internal derangement. Dent Clin North Am 2007;51:195–208.
Melis M, Zawawi KH. Occlusal dysesthesia: A topical narrative review. J Oral Rehabil 2015;42:779–785.
Cioffi I, Michelotti A, Perrotta S, Chiodini P, Ohrbach R. Effect of somatosensory amplification and trait anxiety on experimentally induced orthodontic pain. Eur J Oral Sci 2016; 124:127–134.
Manfredini D, Landi N, Romagnoli M, Cantini E, Bosco M. Etiopathogenesis of parafunctional habits of the stomatognathic system. Minerva Stomatol 2003;52:339–349.
Manfredini D, Bucci MB, Montagna F, Guarda-Nardini L. Temporomandibular disorders assessment: Medicolegal considerations in the evidence-based era. J Oral Rehabil 2011; 38:101–119.
Slade GD, Ohrbach R, Greenspan JD, et al. Painful temporomandibular disorder: Decade of discovery from OPPERA studies. J Dent Res 2016;95:1084–1092.
Huttunen J, Qvintus V, Suominen AL, Sipilä K. Role of psychosocial factors on treatment outcome of temporomandibular disorders. Acta Odontol Scand 2019;77:119–125.
Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofac Surg 2003;61:655–660.
Bucci MB, Aversa M, Guarda-Nardini L, Manfredini D. Occlusion and temporomandibular disorders: A malpractice case with medical legal considerations. Minerva Stomatol 2011; 60:65–74
Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res 1998;77:361–365.
de Bont LG, Dijkgraaf LC, Stegenga B. Epidemiology and natural progression of articular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83:72–76.
Stohler CS. Phenomenology, epidemiology, and natural progression of the muscular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83:77–81.
Manfredini D, Favero L, Gregorini G, Cocilovo F, Guarda-Greene L. Natural course of temporomandibular disorders with low pain-related impairment: A 2-to-3-year follow-up study. J Oral Rehabil 2013;40:436–442.
Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med 2008;359:2693–2705.
Laskin DM. Arthroscopy versus arthrocentesis for treating internal derangements of the temporomandibular joint. Oral Maxillofac Surg Clin North Am 2018;30:325–328.
Forssell H, Kauko T, Kotiranta U, Suvinen T. Predictors for future clinically significant pain in patients with temporomandibular disorder: A prospective cohort study. Eur J Pain 2017; 21:188–197.
Kapos FP, Look JO, Zhang L, Hodges JS, Schiffman EL. Predictors of long-term temporomandibular disorder pain intensity: An 8-year cohort study. J Oral Facial Pain Headache 2018;32:113–122.
Ohrbach R, Fillingim RB, Mulkey F, et al. Clinical findings and pain symptoms as potential risk factors for chronic TMD: Descriptive data and empirically identified domains from the OPPERA case-control study. J Pain 2011;12 (11 suppl):T27–T45.
Greene CS, Laskin DM. Long-term evaluation of conservative treatment for myofascial pain-dysfunction syndrome. J Am Dent Assoc 1974;89:1365–1368.
Whitney CW, Von Korff M. Regression to the mean in treated versus untreated chronic pain. Pain 1992;50:281–285.
Greene CS, Goddard G, Macaluso GM, Mauro G. Topical review: Placebo responses and therapeutic responses. How are they related? J Orofac Pain 2009;23:93–107.
Porporatti AL, Costa YM, Réus JC, et al. Placebo and nocebo response magnitude on temporomandibular disorder-related pain: A systematic review and meta-analysis. J Oral Rehabil 2019;46:862–882.
Laskin DM. Temporomandibular disorders: A term past its time? J Am Dent Assoc 2008;139:124–128.
Costa YM, Conti PC, de Faria FA, Bonjardim LR. Temporomandibular disorders and painful comorbidities: Clinical association and underlying mechanisms. Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:288–297.
Dahan H, Shir Y, Velly A, Allison P. Specific and number of comorbidities are associated with increased levels of temporomandibular pain intensity and duration. J Headache Pain 2015; 16:528.
Laskin DM, Greene CS. Influence of the doctor-patient relationship on placebo therapy for patients with myofascial pain-dysfunction (MPD) syndrome. J Am Dent Assoc 1972; 85:892–894.