Towards a Standardized Tool for the Assessment of Bruxism (STAB)—Overview and general remarks of a multidimensional bruxism evaluation system
ABSTRACT
The aim of the present paper was to give an overview of the general project and to present the macrostructure of a comprehensive multidimensional toolkit for the assessment of bruxism, viz. a bruxism evaluation system. This is a necessary intermediate step that will be detailed in a successive extended publication and will ultimately lead to the definition of a Standardized Tool for the Assessment of Bruxism (STAB) as the final product. Two invitation-only workshops were held during the 2018 and 2019 General Session & Exhibition of the International Association for Dental Research (IADR) meetings. Participants of the IADR closed meetings were split into two groups, to put the basis for a multidimensional evaluation system composed of two main axes: an evaluation Axis A with three assessment domains (ie subject-based, clinically based and instrumentally based assessment) and an aetiological/risk factors Axis B assessing different groups of factors and conditions (ie psychosocial assessment; concurrent sleep and non-sleep conditions; drug and substance use or abuse; and additional factors). The work of the two groups that led to the identification of different domains for assessment is summarised in this manuscript, along with a road map for future researches. Such an approach will allow clinicians and researchers to modulate evaluation of bruxism patients with a comprehensive look at the clinical impact of the different bruxism activities and aetiologies. The ultimate goal of this multidimensional system is to facilitate the refinement of decision-making algorithms in the clinical setting. Further details are accessible for you to learn about diagnostic protocols of bruxism in our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
INTRODUCTION
Bruxism is a controversial and often-discussed topic in dentistry. This has led to recent international efforts to reach consensus and provide an updated definition for widespread use in clinical and research settings.1,2 The criteria for assessment of sleep bruxism (SB) were based on polysomnographic (PSG) recordings, which allow the identification of typical masseter muscle electromyographic (EMG) events that may be associated with sleep arousals and are labelled as rhythmic masticatory muscle activities (RMMAs).3 Over recent years, however, the construct of bruxism has been broadened to encompass a wider spectrum of jaw-muscle activities performed during sleep or whilst awake, also including longer-lasting, prolonged activities that are typical of muscle bracing.2,4 This means that PSG/SB criteria may provide only a partial picture of the complex range of jaw-muscle activities incorporated within the construct of bruxism. Further, no definitive criteria have ever been established for awake bruxism (AB), and no information is available on the necessity to identify the presence of bruxism, as in some individuals it can be a relatively harmless behaviour, without any clinical consequences.5
To construct a framework for the validity of different approaches, a grading system has been proposed by a consensus expert panel.1,2
The grading system suggests that possible sleep/awake bruxism is based on a positive self-report only; probable sleep/awake bruxism is based on a positive clinical findings, with or without a positive self-report; and definite sleep/awake bruxism is based on a positive instrumental assessment, with or without a positive self-report and/or a positive clinical findings.2
The authors of the consensus pointed out that this grading system was only a proposal, and could even be difficult to adapt to current knowledge on the poor clinical validity of cut-off points for assessing the presence or absence of clinically relevant SB and AB.6
In addition to that, the emerging knowledge on the complexity of bruxism aetiology, its concurrent conditions and associated factors, as well as the need for a better understanding of the potential clinical consequences, suggest that a comprehensive assessment system is now required for a better definition of management strategies (eg treatment indications) of patients in the clinical setting.
Given this, an invitation-only workshop entitled “DC/Bruxism,” with experts from around Europe (see Table 1) took place in London, UK, prior to the 96th General Session & Exhibition of the International Association for Dental Research (IADR, July 2018). The meeting was organised by the authors of this article on behalf of the International Network for Orofacial Pain and Related Disorders Methodology (INfORM) of the IADR. A second invitation-only workshop was held in Vancouver, during the 97th General Session & Exhibition of the International Association for Dental Research (IADR, June 2019). The aim of the meetings was to sketch a route towards a future comprehensive publication of a Standardized Tool for the Assessment of Bruxism (STAB). Invited experts unable to attend contributed to the discussion process via email exchanges.
The aim of the present paper is to give an overview of the general project and to present the macrostructure of a comprehensive multidimensional toolkit for the assessment of bruxism, viz. a bruxism evaluation system. This is a necessary intermediate step that will be detailed in a successive extended publication and will ultimately lead to the definition of a set of standardised tools for assessing bruxism as the final product. The final goal of providing a tool for a comprehensive evaluation is to enable and facilitate easy comparison of studies in the research setting and, importantly, to provide a better care of patients in the clinical setting.
TABLE 1 Participants and contributors to the IADR Consensus Meetings (“DC/bruxism”) that were held in London on 26 July 2018 and in Vancouver on 19 June 2019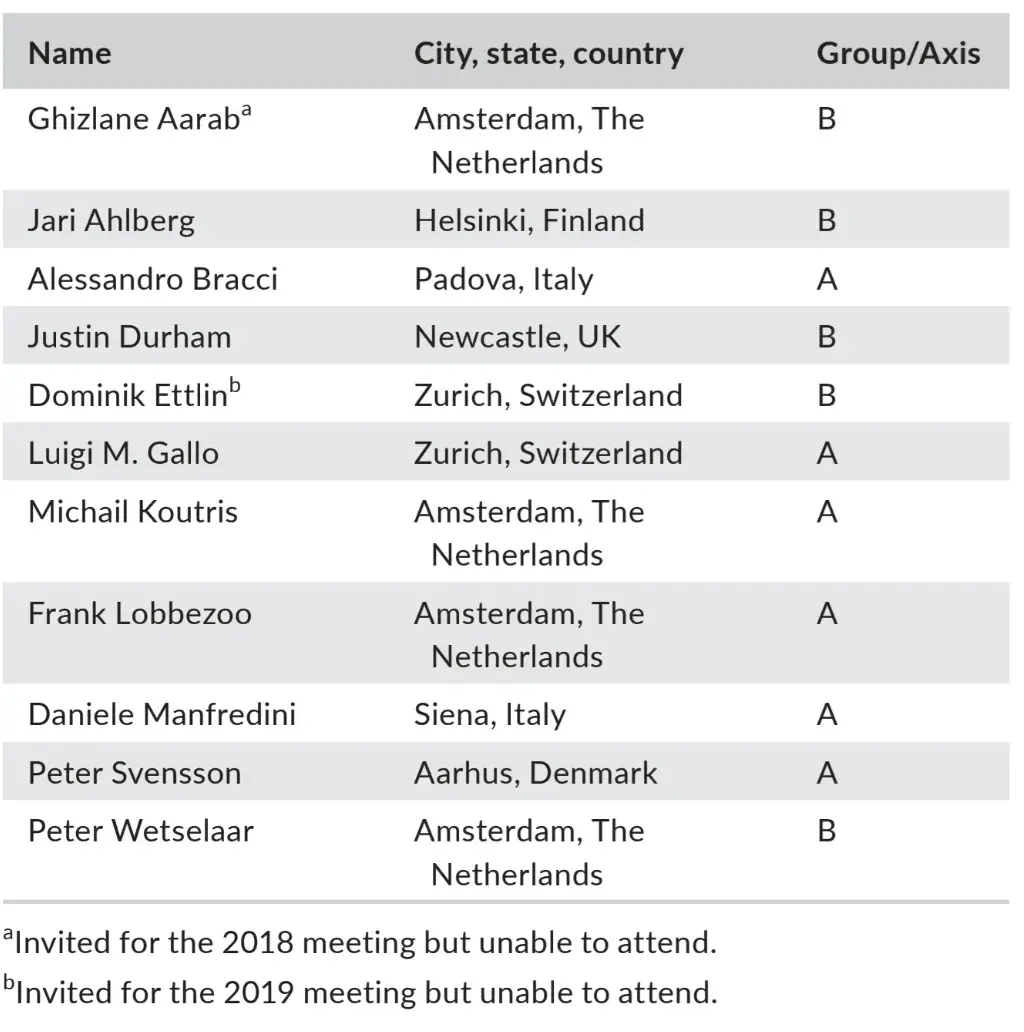
GENER AL STRUCTURE OF THE PROJECT
There are several possible strategies available to help designing instruments for the assessment of the multidimensional nature of bruxism. In particular, clinicians must be aware of the fact that, in an ideal setting, there should be a reference standard (“gold standard”) that can be used to compare the different approaches, as per the grading proposal (ie possible, probable, definite bruxism).2 In the field of bruxism, the gold standard should be based on masticatory muscle activity (MMA) measurement in its continuum. For a number of reasons that have been elucidated in some sequential papers, currently available instruments (ie polysomnography [PSG], electromyography [EMG]) are more theoretical than practical reference standards, since they focus on the peaks of EMG activity of an amplitude that has been associated with sleep arousals.3,7 This means that a definite assessment can be achieved only for that portion of SB activity, but not for the full amount of muscle work exerted by the jaw muscles during sleep time.
Similarly, awake EMG can be obtained and analysed, but practical problems exist to differentiate the different types of recorded muscle activity. Thus, awake muscle work may at this stage more easily be assessed as a behaviour that can be reported by the patient at the time it occurs, viz. by means of ecological momentary assessment.1 Nonetheless, only preliminary data on young adults are available on this approach, thus making it too early to speculate about any reference normality values.8-10
The evolution and enlargement of the bruxism construct over recent years has revealed the need to reconceptualise the complex literature on its clinical correlates, which was often inconclusive, because it did not recognise the different bruxism activities and their multidimensional nature.11,12 In addition, different aetiologies and concurrent conditions may contribute to the amount of bruxism activity and make it complex to find a clear relationship with clinical signs and symptoms.4,13,14
Based on these premises, the first step towards the standardisation of bruxism assessment is the proposal of a bruxism evaluation system, which should undergo a stringent validation process to generate a possible scoring system. Its general structure will be based on a multimodular system that has two clear-cut main axes: an evaluation Axis A and an aetiological/risk factors Axis B.
Axis A deals with the assessment of bruxism/MMA (self-reports, clinical evaluation [signs/symptoms/consequences], instrumental assessment).
Axis B deals with the aetiology and with risk factors and concurrent conditions associated with bruxism/MMA.
Participants of the IADR closed meetings that put the basis for the assessment guidelines were thus split into two groups, coordinated by Frank Lobbezoo and chaired by Daniele Manfredini (Group/Axis A) and Jari Ahlberg (Group/Axis B). The constructive within- and between-group discussions led to some general remarks about the possible splitting of both Axis A and Axis B into multiple subaxes. Lists of putative areas that must be part of the assessment as well as of aetiological factors, concurrent conditions, and risk, protective and associated factors have been prepared.
As part of the future work schedule, specific instruments for the evaluation of each item will be selected and evaluated on-field for inclusion in the extended version of the Bruxism Evaluation System. Then, a stringent validation process will determine the best possible scoring strategy for inclusion in the Standardized Tool for the Assessment of Bruxism (STAB). The work of the two groups is summarised below.
AXIS A—BRUXISM ASSESSMENT
The following issues emerged as a general background for the development of an Axis A:
The Axis A should focus on the evaluation of bruxism status, including the clinical signs, symptoms and other consequences that are potentially associated with bruxism.
Three main domains for assessment of bruxism status were identified, based on the source and strategy adopted to gather information, viz. subject-based assessment, clinically based assessment and instrumentally based assessment.
Within these premises, the three main assessment domains are conceptualised as follows:
The subject-based assessment includes self-report (eg questionnaires, interviews) of current bruxism status; a history report of bruxism status; and a report of complaints possibly related to bruxism.
The clinically based assessment provides an evaluation of clinical data that are directly related to bruxism (ie signs) as well as others that are indirectly associated (ie symptoms and other potential consequences). It includes a clinical assessment of the temporomandibular joint (TMJ) and muscles status; an intraoral examination and inspection of the soft and hard tissues; and dentistry-related signs of events potentially due to bruxism (eg signs in oral mucosal tissues, mechanical tooth wear; broken restorations).
The instrumentally based assessment includes EMG for recording sleep MMA; ecological momentary assessment (EMA) for AB; and additional instruments such as PSG to gather data on arousal-related events and their correlates.
Based on the above-described general framework for Axis A, a specific list of items can be identified for each assessment domain. In turn, each domain is divided into three subaxes, as identified by the best possible grouping of evaluation items in terms of homogeneity of contents:
Subject-Based Assessment (SBA):
A1 (Current bruxism report): interview or questionnaire-based report about awareness and frequency on current bruxism.
A2 (History of bruxism report): interview or questionnaire-based report about past bruxism.
A3 (Patient complaints): report of non-painful muscle symptoms as well as muscle pain; joint pain; teeth soreness; tooth wear-related complaints (ie deterioration in aesthetic appearance; sensitivity; functional problems; pain); dental history (eg history of broken teeth or restorations); pain on awakening; intermittent locking; grinding sounds; and neck/shoulder pain. For each complaint, information on awareness, perceived intensity, current frequency, duration, history and level of burden will be collected.
As an important note, it must be remarked that report of current bruxism (“A1”) should be considered different from the report of past/history of bruxism (“A2”), since the report of bruxism history adds an extra dimension to the assessment that cannot be evaluated with instrumentation. It should be also specified that discrimination is required between the awareness of possible signs/symptoms related to bruxism (“A3”) vs the awareness of bruxism itself (ie keeping the muscle tense during the wakefulness or sleep, grinding teeth during night) (“A1”). For all items, existing and validated questionnaires should be used, when available. If not available, specific questions will be selected and adapted to that purpose via Delphi process and subsequent on-field testing.
Clinically Based Assessment (CBA):
A4 (Joint/Muscles): joint palpation for sounds and pain; masseter muscle palpation for structure, asymmetry and pain; temporalis area palpation for pain; dynamic/static testing for function-dependent pain; and neck/shoulder muscles palpation for consistency and pain.
A5 (Intraoral tissues): linea alba; tongue scalloping; lip impressions; and exostoses.
A6 (Teeth and Restorations): mechanical tooth wear, with possible discrimination from chemical tooth wear, as well as between physiological and non-physiological tooth wear; periodontal problems; endodontic problems; cracked teeth; broken restorations; prosthodontic failures, including mechanical complications on implant-supported restorations; and oral appliance evaluation.
For all items, existing and validated techniques and rating scales should be used, when available. For some items, especially concerning the intraoral inspection part of the examination, standardised evaluation tools are not available yet. Thus, reliability assessment strategies will be suggested for an acceptable calibration of different examiners.
Instrumentally Based Assessment (IBA):
A7 (Sleep bruxism): EMG activity of jaw muscles during sleep (eg EMG traces of PSG recordings; single-channel EMG recordings).
A8 (Awake bruxism): EMA for frequency of report; and EMG for MMA recording.
A9 (Additional instruments): full PSG, and possible definition of biological markers that may reflect the presence of bruxism (eg MRI evaluation of muscle volume; spectroscopy; ultrasonography for muscle thickness; bite force on appliances).
For all items of the IBA, validated instruments should be used, when available. If not available, instruments will be developed to that purpose.
AXIS B—BRUXISM AETIOLOGY, RISK FACTORS AND CONCURRENT CONDITIONS
The following issues emerged as a general background for the development of an Axis B:
The Axis B should focus on the evaluation of bruxism aetiology, risk factors and concurrent conditions, even including those conditions that may lead to positive health outcomes related to bruxism, and the vulnerability factors that may facilitate the onset of bruxism-related consequences.
Different categories of factors and conditions are identified and grouped into the following domains: psychosocial assessment; concurrent sleep and non-sleep conditions; drug and substance use or abuse; and additional factors.
Given the evolving nature of knowledge, any clear-cut splitting into categories based on the actual kind of relationship that each factor/condition has with bruxism (ie either aetiological or associated condition) was not performed.
Within these premises, the main assessment domains are conceptualised as follows:
The psychosocial assessment includes an evaluation of the full spectrum of psychological and social factors that may be associated with bruxism.
The concurrent sleep-related conditions assessment provides an evaluation of the sleep disorders and conditions that may be associated with bruxism.
The concurrent non-sleep conditions assessment focuses on concurrent disorders and conditions that are not necessarily related with sleep but may be associated with increased MMA.
The prescribed medications and use of recreational substances assessment evaluates the intake of any substance that may act as an additive or reductive factor for the amount of bruxism activity.
The additional factors assessment provides a list of individual features that may predispose to the onset of bruxism-related clinical consequences as well as additional factors that are potentially related with bruxism and are not included in the preceding domains.
Based on the above general framework for Axis B, a specific list of items can be identified for each assessment domain:
Psychosocial assessment:
Psychological factors potentially associated with bruxism (eg anxiety, stress sensitivity, coping skills). There will potentially be many others, especially considering the complex relationship with pain, but at present, the list is limited to the ones that are most commonly studied for a direct association with bruxism.
Concurrent sleep-related conditions assessment:
Disorders, including signs and symptoms: obstructive sleep apnoea (OSA), parasomnia, insomnia (prolonged latency, disruptions, early awakening), daytime fatigue and periodic sleep movement disorder.
Epiphenomenon: neurovegetative signs (sleep studies).
Nocturnal gastroesophageal reflux disorder (nGERD).
Concurrent non-sleep conditions assessment:
Neurological disorders: Parkinson/REM sleep behaviour disorder, epilepsy, CVA and traumatic head injury (primary versus secondary).
Endocrine disorders: for example hyperthyroidism.
GERD.
Prescribed medications and use of recreational substances assessment:
Drugs thought to have increasing or decreasing effects on bruxism/MMA: selective serotonin reuptake inhibitors (SSRI); selective norepinephrine reuptake inhibitors (SNRI); antipsychotics; tricyclic antidepressants (TCA); benzodiazepines; clonidine; and other hypotension-inducing drugs.
Drugs thought to have dual effects on bruxism/MMA: antiparkinsonian medications (they may reduce bruxism, but at long term, there might be an increase in dyskinesic MMA)
Substances associated with increased bruxism/MMA: nicotine; caffeine; alcohol; and psychoactive substances.
Biological biomarkers and additional factors:
Biological markers: salivary cortisol; urinary catecholamine; substance P; and genotype and receptor expression.
Additional factors: somatosensory information (central and peripheral sensitisation).
For all items of the Axis B domains, validated instruments should be used, when available. A definitive subdivision of the Axis B in specific subaxes might also be taken into consideration as evidence on specific relationships with bruxism emerges.
There are additional details about diagnostic and treatment protocols of bruxism in our course "Encyclopedia of Bruxism and Apnea".
DISCUSSION
The emerging paradigm of bruxism as a complex spectrum of centrally mediated jaw-muscle activities without a clear-cut relationship with clinical consequences makes the establishment of assessment guidelines a compelling need for the practice of several medical disciplines. Within this premise, an ideal evaluation system should define the status of having/not having a condition (ie bruxism) with certainty.
In the field of bruxism, such a definite characterisation is currently achievable only for certain EMG events identified as a rhythmic masticatory muscle activity (RMMA) typical of arousal-related sleep bruxism. Tonic contractions featuring prolonged periods of isometric, sustained muscle activity during sleep require a dedicated elaboration of the EMG signal to be properly identified and measured, which is not achievable yet. It should also be defined which masticatory muscles should be monitored and which analysis criteria would be the most accurate to use. Indeed, there has been a shift from the contraction episode analysis 15 to the low level, long-lasting activity (duty factor analysis).16-18 Similarly, the measurement of jaw-muscle activity during wakefulness presents technical difficulties, which may be overcome with future progress in the development of dedicated tiny sensors. In addition, a real-time report of patients’ awake bruxism behaviours is a promising strategy that requires refinement and calibration.
This means that, in spite of the recent suggestions of a grading system, the current enlarged bruxism construct (ie including muscle activities not limited to the typical sleep-time RMMA) makes it difficult to build up a practical hierarchy of accuracy. The theoretical framework of a “possible,” “probable” and “definite” bruxism should remain the ideal target. It categorises the way bruxism has been assessed so far and adds to a better understanding of the phenomenon of interest, but it must be pointed out that such a grading system cannot be based on an existing standard of reference.
For this reason, a comprehensive evaluation system will be based on the idea that gathering as much information as possible is the best available option to start the process of defining a set of standardised bruxism assessment toolkits. A list of items reflecting the subject-reported and clinically and instrumentally reported information represents the basis for any future steps.
The core premise of the project is that a clear-cut relationship between aetiology, bruxism and clinical consequences has never been established, because of the absence of differentiation between the muscle activities that are included under the umbrella term “bruxism.” The unspecific use of the term bruxism has created confusion as for the clinical relevance of research findings and viceversa, making it hard to even define when bruxism status is actually a risk factor for certain health outcomes or a potentially protective factor for others, and when not. Many conceptual and clinical speculations can be made on this issue. For instance, from a conceptual view-point, should bruxism be considered a problem only when clinical consequences are present, or should it be considered pathological when the amount of muscle activity or reported behaviour is high, independent of the presence of clinical consequences? On the other hand, from a clinical viewpoint, it is likely that investigations on the bruxism-pain or bruxism-tooth wear relationship would benefit from the discrimination of the muscle behaviours, even included the engagement in tooth contact habits. Thus, a comprehensive instrument trying to link the possible causes that lead to the different types of bruxism and, in turn, to the possible different consequences could have an important impact on multiple medical communities.
To shed light on this issue, the choice has been to identify two separate axes, with the goal of separating the bruxism status itself from its possible aetiology.4 This strategy is in line with the bruxism definition, from which all hints at aetiological aspects, associations and consequences have been removed.1 Thus, an Axis A dealing with the assessment of the bruxism status will be complemented by an Axis B investigating for the possible aetiological, concurrent and associated factors and conditions that may be associated with bruxism/MMA.
As for Axis B, it is important to note that the listed conditions include those that may lead to positive health outcomes related to the associated bruxism activity. The need to separate the aetiology from the consequences is best exemplified by an imaginary individual with severe (mechanical) tooth wear. Mechanical tooth wear maybe due to sleep-time masticatory muscle activity, which in turn maybe associated with respiratory arousals and may decrease with the reduction in apnoea events in some individuals, thus representing a positive indirect health outcome. A similar example could concern the relationship between bruxism, tooth wear and gastroesophageal reflux disease.19
The result of the above considerations is a multidimensional system, with two main evaluation axes that interact with each other. The outcome is a network of subject-based and clinically and instrumentally based information related to bruxism status and the related issues.
The challenges for the future, as detailed below, are (a) to create a full version of the bruxism evaluation system that will be extensively evaluated on-field and will ultimately result in the Standardized Tool for the Assessment of Bruxism (STAB), and (b) to create a scoring system for each subject-based, clinically based and instrumentally based domain, viz. ideally representing the concept that the higher the score the more severe the bruxism activity in terms of clinical impact and patient's burden. Ideally, a graphical visualisation of the multidimensional evaluation should be conceptualised, to help clinicians with a tool that offers an immediate insight into the bruxism status.
The advantages of such multidimensional evaluation are multiple. In particular, it must be pointed out that it is a rational attempt to connect the aetiology with all types of information concerning the patient-related and instrumental findings, even comprising the clinical manifestations and consequences. This is important for the adoption of such model in the clinical setting, since it will help clinicians’ understanding that bruxism is a complex result of different possible Axis B conditions and factors and that the management of clinical consequences, when present, can be more easily planned by taking into account a careful multidimensional evaluation. Thus, a comprehensive evaluation system can be viewed as an intermediate step towards the definition of a set of standardised tools for the assessment of bruxism, which could lead to clinical decision-making algorithms that might shed light on the “when and when not” issue concerning bruxism management at the individual level. To reach that goal, cluster and/or multivariate discriminant analysis algorithms could be used.
Another interesting feature of a multidimensional evaluation system is its possible implementation and refinement with future knowledge. Just a couple of examples concern the EMG assessment strategies and the categorisation of Axis B. As for the EMG, within the set of instrumental tools, there is now agreement that EMG could be enough for an evaluation of sleep-time MMA and that a yes/no approach based on cut-off thresholds is premature to adopt at this stage of knowledge. As soon as new, dedicated software is available to elaborate EMG signals, a more comprehensive evaluation strategy (eg measurement of the amount of muscle work) with respect to the current peaks counting, could be implemented. As for Axis B, possible different strategies to provide a less item-specific categorical approach than the current detailed list, which evidently remains incomplete, could emerge. For instance, a subdivision of factors into morphological, psychosocial, physiological and biological, and exogenous variables could be equally useful for providing the clinician with an orientation of the bruxism status.20
Future steps
The road map of the next steps provides the upcoming release of a detailed bruxism evaluation system, which will be finalised in the near future by this group of authors.
As a first step, the panel members will prepare a list of questionnaire and clinical items for possible inclusion in the SBA and CBA domains. Items will be proposed based on personal knowledge and integrated with a thorough literature review on the questionnaire-based, interview-based and clinically based methods that have been used to assess the bruxism status and evaluate the potential correlation with clinical signs/symptoms. As a general remark, the main recommendation is to adopt current classifications or evaluation tools, when available, so that priority will be given to pre-existing validated, standardised items. A Delphi process could be adopted to define a list of provisional items. The provisional SBA and CBA subaxes will undergo multicentre on-field testing to identify possible overlap and/or redundancy of items and assess internal consistency. Such process will allow reducing the number of items, to create the definitive SBA and CBA, and finalise the Axis A of the Bruxism Evaluation System. Similarly, a list of conditions and factors will also be prepared with the same strategy to finalise the Axis B.
As a second step, the Standardized Tool for the Assessment of Bruxism (STAB) will be developed. To do that, all the various subaxes of the proposed multidimensional bruxism evaluation system will be cross-correlated via a series of investigations on different populations. The aims of this phase will be (a) the definite identification of bruxism status based on the levels of MMA during sleep or wake-fulness as well as the frequency of behaviour during wakefulness, and (b) the assessment of correlation of such status with the subject-based and clinically based assessment domains as well as with the different Axis B categories. For all primary investigations, the core expert panel will be expanded with the inclusion of selected research groups and co-authors, based on their availability to carry on on-field work. At the end of this second phase, the interconnection of domains will be established—from aetiology and concurrent conditions (Axis B) to bruxism status (Axis A—IBA) and subjective and/or clinical markers (Axis A—SBA/CBA).
As a third and final step, artificial intelligence strategies will be used to mine the amount of data collected with primary researches. Indeed, it could be expected that the quantity of collected data quickly reaches a hardly manageable size, so that new analysis strategies should be developed (eg big data, artificial intelligence). Scoring criteria for each subaxis could be defined to figure out a graphical visualisation of the bruxism assessment. Models to predict causes for additive bruxism in the presence of certain subjective or clinical items, and vice versa, could be built up. Different usage strategies for research and clinical purposes and for a tailored management at the individual level will be defined. The deriving implications could be interesting, especially concerning the possible fit with on-going developmental efforts in the fields of sleep and pain medicine classification.
During all phases of the project, a series of manuscripts will be prepared to explain methods, to provide data from primary researches, to facilitate the dissemination of the system and to inform the clinical and research communities on the future developments. To that aim, individuals external to this core panel could be invited to co-author specific articles on selected subtopics. For instance, this could be important in helping to determine the need, or otherwise, to assess bruxism in children and adolescents, which is not yet included in the project and has been source of much speculation and discussion in the clinical settings. Papers dealing with the topics of bruxism and (mechanical) tooth wear, bruxism and pain, and bruxism and concurrent conditions are other examples of future expansion works.
Each paper could represent the basis to establish working groups on the topic. Within these premises, a better management of bruxism in the clinical setting is expected as the ultimate goal of the entire project, as well as an improvement of knowledge on bruxism as a whole and a better communication between the different communities of bruxism experts and general practitioners.
CONCLUSIONS
Despite being a very common topic in recent dental and sleep medicine literature, bruxism has never been the subject of standardised assessment guidelines. This paper presents the first step towards the possible creation of a Standardized Tool for the Assessment of Bruxism (STAB). A bruxism evaluation system has been proposed, which is currently under preparation and refinement by the panel of professionals listed in Table 1 on behalf of the INfORM network of the IADR. The underlying idea is that the general grading template, that was introduced by the recent consensus papers, will be adapted and refined into a multidimensional evaluation system, providing an assessment of both bruxism status (Axis A) and the presence of aetiological, concurrent, risk, protective and associated factors and conditions (Axis B). Such an approach will allow clinicians and researchers to evaluate bruxism patients with a comprehensive look at the clinical impact of the different bruxism activities and aetiologies. The ultimate goal of this multidimensional system is to facilitate the refinement of decision-making algorithms in the clinical setting.
Author's information
Daniele Manfredini
Jari Ahlberg
Ghizlane Aarab
Alessandro Bracci
Justin Durham
Dominik Ettlin
Luigi M. Gallo
Michail Koutris
Peter Wetselaar
Peter Svensson
Frank Lobbezoo
References
Lobbezoo F, Ahlberg J, Glaros AG, et al. Bruxism defined and graded: An international consensus. J Oral Rehabil. 2013;40:2-4.
Lobbezoo F, Ahlberg J, Raphael KG, et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018;45:837-844.
Lavigne GJ, Rompré PH, Montplaisir JY. Sleep bruxism: validity of clinical research diagnostic criteria in a controlled polysomnographic study. J Dent Res. 1996;75:546-552.
Manfredini D, De Laat A, Winocur E, Ahlberg J. Why not stop looking at bruxism as a black/white condition? Aetiology could be unrelated to clinical consequences. J Oral Rehabil. 2016;43:799-801.
Raphael KG, Santiago V, Lobbezoo F. Is bruxism a disorder or a behaviour? Rethinking the international consensus on defining and grading of bruxism. J Oral Rehabil. 2016;43(10):791-798.
Manfredini D, Ahlberg J, Wetselaar P, Svensson P, Lobbezoo F. The bruxism construct: from cut-off points to a continuum spectrum. J Oral Rehabil. 2019;46(11):991-997.
Rompré PH, Daigle-Landry D, Guitard F, Montplaisir JY, Lavigne GJ. Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res. 2007;86:837-842.
Bracci A, Djukic G, Favero L, Salmaso L, Guarda-Nardini L, Manfredini D. Frequency of awake bruxism behaviors in the natural environment. A seven-day, multiple-point observation of real time report in healthy young adults. J Oral Rehabil. 2018;45:423-429.
Zani A, Lobbezoo F, Bracci A, Ahlberg J, Manfredini D. Ecological momentary assessment and intervention principles for the study of awake bruxism behaviors, Part 1: general principles and preliminary data on healthy young Italian adults. Front Neurol. 2019;10:169.
Osiewicz MA, Lobbezoo F, Bracci A, Ahlberg J, Pytko-Polończyk J, Manfredini D. Ecological momentary assessment and intervention principles for the study of awake bruxism behaviors, Part 2: development of a smartphone application for a multicenter investigation and chronological translation for the Polish version. Front Neurol. 2019;10:170.
Svensson P, Jadidi F, Arima T, Baad-Hansen L, Sessle BJ. Relationships between craniofacial pain and bruxism. J Oral Rehabil. 2008;35:524-547.
Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e26-50.
Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil. 2001;28:1085-1091.
Thymi M, Shimada A, Lobbezoo F, Svensson P. Clinical jaw-muscle symptoms in a group of probable sleep bruxers. J Dent. 2019;85:81-87.
Gallo LM, Gross SS, Palla S. Nocturnal masseter EMG activity of healthy subjects in a natural environment. J Dent Res. 1999;78(8):1436-1444.
Manfredini D, Fabbri A, Peretta R, Guarda-Nardini L, Lobbezoo F. Influence of psychological symptoms on home-recorded sleep-time masticatory muscle activity in Healthy subjects. J Oral Rehabil. 2011;38(12):902-911.
Raphael KG, Janal MN, Sirois DA, et al. Masticatory muscle sleep background electromyographic activity is elevated in myofascial temporomandibular disorder patients. J Oral Rehabil. 2013;40(12):883-891.
Iwasaki LR, Gonzalez YM, Liu H, Marx DB, Gallo LM, Nickel JC. A pilot study of ambulatory masticatory muscle activities in temporomandibular joint disorders diagnostic groups. Orthod Craniofac Res. 2015;18(Suppl 1):146-155.
Wetselaar P, Manfredini D, Ahlberg J, et al. Associations between tooth wear and dental sleep disorders. A narrative overview. J Oral Rehabil. 2019;46(8):765-775.
Lobbezoo F, Van Der Zaag J, Naeije M. Bruxism: its multiple causes and its effects on dental implants – an updated review. J Oral Rehabil. 2006;33:293-300.