Temporomandibular disorders assessment: medicolegal considerations in the evidence-based era
SUMMARY
Temporomandibular disorders (TMD) are a frequent finding in cases of facial trauma or dental malpractice, and legal claims for TMD damage have been increased over the years. Temporomandibular disorders assessment in the medical legal setting is complicated by the peculiarities of these disorders, whose symptoms are heterogeneous, fluctuant, and recognise a multifactorial origin. A systematic Medline search in the National Library of Medicine’s PubMed database pointed out that, despite the medical legal aspects of the dental profession are gaining a growing attention, there is a paucity of literature dealing with patients with TMD assessment. For these reasons, evidence-based knowledge in the field of TMD diagnosis and treatment was summarised in this article with the aim of providing useful suggestions for a medical legal approach to TMD.
You have the opportunity to gather more in-depth information about temporomandibular disorders diagnosis and treatment in our Online congress on evidence-based temporomandibular disorders and bruxism treatment .
INTRODUCING
Temporomandibular disorders (TMD) are a heterogeneous group of pathologies affecting the temporomandibular joint (TMJ), the masticator muscles, or both (1). Temporomandibular disorders may present with a number of signs and symptoms, the most common of which are pain localised in the pre-auricular area and ⁄ or in the masticatory muscles; jaw motion abnormalities; articular sounds, such as click and ⁄ or crepitus, during mandibular movements (2). A specific etiopathogenesis is rarely demonstrable, because most cases have to be reconducted to a multifactorial etiopathogenetic pathway (3–5). Epidemiological data showed a female pre-dominance, which is more marked in patients’ populations, and a mean age of onset around 35–45 years, with two distinct age peaks for internal joint derangements and inflammatory-degenerative disorders (6–11).
The complex etiopathogenesis and the variability of symptoms make it difficult to adopt standardised diagnostic and therapeutic protocols, thus reflecting in the proposal of several different treatment approaches, such as occlusal splints (12, 13), physiotherapy (14, 15), behavioural treatments (16, 17), physical therapy (18), drugs (18–21), minor (22–24) and, major surgery (25–27).
In the recent years, many progresses have been made in the attempt to design reference principles for the diagnosis and treatment. This led to the diffusion of internationally recognised academic guidelines for the assessment and management of patients with TMD in the clinical setting (28–32) and to the adoption of a standardised protocol translated in several languages, viz., the Research Diagnostic Criteria for TMD (33–36), for the diagnosis and classification of such disorders in the research setting. Also, some seminal articles provided evidence-based invoices for the adoption of low-technology, high-prudence, conservative, reversible approaches to TMD (37–39). Nevertheless, non-specialist and non-expert practitioners still refer many uncertainties at both diagnostic and therapeutic levels (40, 41), thus suggesting that the quality of communication between the research and clinical settings, viz., the science transfer process, should be enhanced (42, 43). In particular, it seems that the well-documented view of TMD as non-dentally related disorders (44–47) is hard to be accepted by the general dental practitioners, who had been accustomed for years to provide occlusally based treatments to their patients with TMD and are reluctant to accept any paradigmatic shifts in their daily practice (48, 49).
The problems of diffusion of evidence-based knowledge into the clinical TMD practice might influence the approach to the assessment of TMD also in the medical legal setting, because of the potential selection of courts’ advisors among practitioners not belonging to the group of front-line experts, researchers, and academicians. In the next future, also considering that the legal aspects of the dental profession are gaining a growing attention, this may become a matter of concern, because TMD and, more in general, orofacial pain symptoms are a common finding in cases of facial trauma or dental malpractice. In both cases, an assessment of the functional limitation of the masticatory system is an essential part of the medical legal evaluation. Considering these premises, this article is intended to pursue the twofold aim to review systematically the medical legal literature on TMD and to briefly summarise up-to-date evidence-based knowledge in the field of TMD diagnosis and treatment, thus providing a useful tool for consultation in the medical legal setting.
Literature search
On 6 November 2009, a systematic search within the National Library of Medicine’s PubMed database was performed to identify English-language, peer-reviewed articles published in the medical literature dealing with the medical legal aspects of TMD assessment and management. The search was performed by two of this review’s authors (D.M.; M.B.B.), who assessed independently the lists of citations to screen for titles of potential interest. In cases of disagreement between the two reviewers, the article was retrieved in full text. Full-texts articles were then included in the review by consensus, which was reached in all cases. The first step of search strategy provided that the following two Medical Subjects Headings (MeSH) terms were used:
Temporomandibular joint disorders: A variety of conditions affecting the anatomical and functional characteristics of the TMJ. Factors contributing to the complexity of temporomandibular diseases are its relation to dentition and mastication and the symptomatic effects in other areas that account for referred pain to the joint and the difficulties in applying traditional diagnostic procedures to TMJ pathology where tissue is rarely obtained and X-rays are often inadequate or non-specific. Common diseases are developmental abnormalities, trauma, subluxation, arthritis, and neoplasia. Year introduced 1997 (previous indexing: TMJ diseases 1982–1996).
Forensic medicine: the application of medical knowledge to questions of law. Year introduced: 1965. The combination of the two MeSH terms, which yielded, respectively, 12 189 and 73 182 citations if used alone, provided only five citations, three of which were in languages other than English and none of which dealt with the issue of this review.
Thus, as a second step in literature search, some combinations of terms were used to try identifying other potential references to be included in the review. The terms ‘legal medicine and temporomandibular disorders’ identified 17 citations. After screening of the titles and available abstracts, four articles were retrieved in full text, but none of them was included for further processing in the review because of either the absence of focus on the medical legal assessment (50) or their character of brief opinions ⁄ letters (51–53). The terms ‘forensic medicine and temporomandibular disorders’ yielded an eight-citation subgroup of the former. Finally, 14 citations were yielded by the terms ‘medical legal and temporomandibular disorders’, among which two articles to be included in the review were found (54, 55). Search was then expanded to the related articles to the included ones, but no other titles of interest for the review were found. Thus, only two articles were retrieved dealing with the argument of TMD and legal medicine.
In consideration of the fact that a systematic assess-lment within the PubMed database showed that only two articles were published on the issue under review, the authors were forced to withdraw from the original purpose to provide an updated comprehensive review of the available literature on TMD assessment for legal purposes, and the following sections were forcedly intended to provide an overview on the medical legal aspects of TMD assessment in relation to the currently available evidence-based concepts on TMD diagnosis and management. 102 D. MANFREDINI et al.
TMD in the era of evidence-based medicine
There is consensus in the scientific community that the decisions taken in a clinical setting should be scientifically supported, in accordance with the principles of the so-called evidence-based medicine (EBM) (56). The field of TMD should not be an exception but, unfortunately, it seems that some misbelieves characterising past theories on TMD aetiology, diagnosis and treatment are still diffused among clinical practitioners (57).
Since the time, 75 years ago, the otorhinolaryngologist Costen described the case of a patient with symptoms in the pre-auricular area and attributed their onset to the loss of molar support (58), dentists have been unofficially reserved the right to treat patients affected by the so-called Costen’s syndrome. Several aetiological theories and treatment approaches, all based upon the occlusal paradigm, were then proposed over the years in the attempt to refine the early observations, and supposed occlusal abnormalities were considered the causal factor, and their correction was viewed as the therapeutic target (4, 57). Notwithstanding that, as early as in the 1950s, more and more evidence began to emerge that other factors play an important role in the onset of signs and symptoms of stomatognathic dysfunction (59, 60); consequently, the original occlusal theory was progressively modified to include new risk factors in a multifactorial model for disease, and many different terms were proposed to indicate the disorders underlying clinical symptoms (e.g. myofascial pain dysfunction syndrome; TMJ dysfunctional syndrome; algico-dysfunctional syndrome). It was only in the last decade that the long-lasting quarrel about the name of the disease apparently ceased with the adoption of the term TMD with broad consensus of the international community (33).
Nonetheless, because of their complexity and variability of symptoms, TMD have been continued to be approached empirically, and the diffusion of science-based knowledge outside from the research setting has been much less than optimal (43). This brought much confusion in the clinical setting, where a number of pseudoscientific approaches grown up either within or outside the dental profession, viz., applied kinesiology (61), neuromuscular dentistry (62), posturography (63), contributed to mud waters in the field of TMD practice. Several systematic reviews of the literature performed over the past two decades have shown beyond any reasonable doubt that such approaches, which basically are ‘restyled’ versions of the old-fashioned occlusal theories, do not deserve scientific dignity because of their failure to fulfil basic requirements needed to provide support to their clinical validity (e.g. test–retest and inter-operator reliability; diagnostic accuracy; relation with the main diagnostic markers or therapeutic outcome variables, viz., pain; cost-effectiveness ratio) (64–70). Research on TMD aetiology has now entered the genomic era (71, 72), the clinical approach to such disorders has now found many similarities with what provided to other chronic pain patients (73–75), and, definitively, TMD are now viewed as musculoskeletal disorders belonging to the complex chapter of orofacial pains (1, 76). Occlusally based theories have been repeatedly dismantled by works showing the low predictive value of occlusal features to identify patients with TMD (77, 78), by investigations showing the poor clinical significance of symptoms induced by the insertion of artificial occlusal interferences in healthy subjects (79, 80), and, even more importantly, by multiple systematic reviews suggesting that occlusal treatment is not useful to treat or prevent TMD (81–84).
In view of those considerations, one would expect that occlusion is no more the focus of TMD treatment and that the supposed usefulness of any diagnostic or treatment technique still focusing on the analysis of dental occlusion would be diminished in the daily activity of the TMD practitioners. Moreover, one would expect that occlusal practitioners are asked for the proofs of evidence justifying their actions, in accordance with some basic ethical and medical legal principles (85). Lastly, one would expect that evidence-based knowledge provides the guiding principles for all the legal decisions in the sphere of TMD practice.
Evidence-based knowledge on TMD diagnosis and management
It appears obvious that, even if in a clinical setting science-based data have to be integrated with experience-based knowledge to provide the best available service to the patients, medical legal advices should be based on evidence-based knowledge alone to avoid any possible opinion-related evaluation bias (85).
Systematic reviews, ranked IIA in the hierarchy of evidence (56), must be considered the most suitable source to retrieve scientifically sound information on the best protocols to diagnose and treat diseases. Thus, again, a systematic search in the PubMed database performed on 6 November 2009 by the use of the terms ‘temporomandibular disorders and diagnosis’ and ‘temporomandibular disorders and treatment’ showed that 9 and 16 reviews were conducted in the form of systematic assessment of literature data on TMD diagnosis and treatment, respectively.
TMD diagnosis
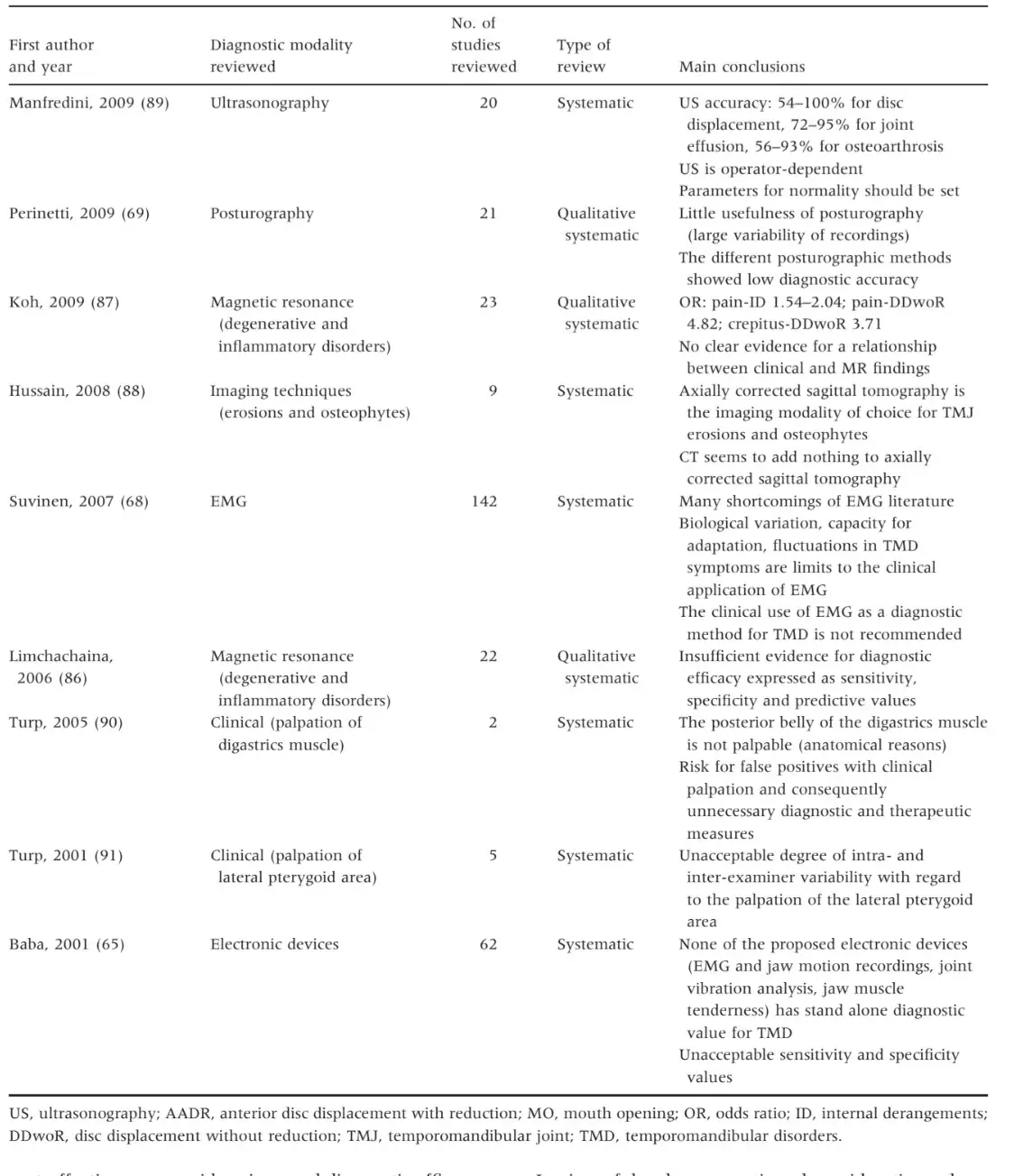
Systematic reviews on the diagnostic approach to TMD covered the arguments of the accuracy of several diagnostic tools, viz., magnetic resonance (n = 2) (86, 87), imaging techniques (n = 1) (88), ultrasonography (n = 1) (89), clinical diagnosis (n = 2) (90, 91), electronic devices (n = 2) (65, 68), posturography (n = 1) (69) (Table 1). Taken together, findings suggest that a clear-cut relationship between clinical symptoms and specific instrumental or imaging signs has been shown only in a minority of cases. Pain is the guiding symptom in the phases of decision-making and treatment planning, and efforts should be directed towards its definition, description and management (92).
At present, a concrete relation between muscle pain and an instrumental sign has not been demonstrated, except that pain within the masseter muscle elicited by a pressure algometer (93). Several instrumental and electronic devices, mainly based on electromyographic activity measurement and jaw motion recording, were proposed during the years as the definitive diagnostic tool for myofascial pain of masticatory muscles but, as in the case of other similar muscle disorders, they lack in reliability and accuracy (64, 94). This consideration is applicable to both surface electromyography and mandibular kinesiography, which do not allow an improvement in diagnostic accuracy with respect to clinical assessment alone, mainly because no direct relation between pain and electromyography (EMG) levels has been well documented, as shown by both the most recent systematic (68) and comprehensive literature reviews (95, 96). This means that pain is not a dependent variable of EMG values and prevents from establishing an evidence-based cut-off value to discriminate pathological from non-pathological EMG levels, so limiting the diagnostic validity of EMG-based instruments. Similarly, evidence is lacking to support the use of posturographic techniques in any phase of the TMD practice (69, 97, 98), thus not justifying their inclusion in any clinical or medicolegal assessment protocol.
The majority of data on the accuracy of TMD diagnosis came from studies on the relationship between clinical and imaging findings. Pain within the TMJ seems to be related with magnetic resonance effusion (99, 100), and effusion has a much debated relation with disc displacements (101–103) and a more clear association with inflammatory-degenerative disorders (104). The diagnostic process for TMD may be integrated with the adoption of appropriately selected imaging techniques to get deeper into the study of the different joint structures. As stated in some articles and early reviews dating back to the past decade (105, 106), magnetic resonance still remains the first choice examination, representing the standard of reference for soft tissues assessment, and it allows depicting the disc position and structure abnormalities with a good accuracy when compared to autopsy specimen (107), also allowing to achieve a good intra-observer achievement (108). Computerised tomography should be reserved to the most complex post-traumatic and surgical cases, when an accurate depiction of bone structures is strongly requested (107), and recent evidences suggest that cone-beam computerised tomography (CBCT) may be a valid alternative to CT, thanks to the lower dose of radiations (109). According to the present knowledge, there is no place for traditional tomography and orthopantomography in the specialistic phase of the TMD diagnostic process (110, 111), while ultrasonography, which has been recently introduced in the TMD literature, gave promising results and may be useful for repeated assessments of joint effusion rather than disc displacement evaluation, even if it is operator-dependent and not yet supportable for routine use (89).
The application of high-quality imaging techniques to the study of the TMJ has allowed gaining a better insight into this joint, also allowing to better correlate joint abnormalities with pain, which is the main reason for patients to seek for TMD treatment. This made the diagnosis of joint disorders easier and may have some impact in the choice of the treatment approach as well. Notwithstanding that, the available systematic reviews pointed out that the knowledge on TMJ imaging techniques is based on studies of less than optimal methodological quality (86, 87); importantly, cost-effectiveness considerations and diagnostic efficacy thinking should be at the basis of the prescription of TMJ imaging modalities in the clinical setting (112).
In view of the above-mentioned considerations, there is consensus that the standard of care for TMD diagnosis is a thorough clinical evaluation performed according to a validated diagnostic scheme and reliable and repeatable techniques, as pointed out in the diagnostic guidelines proposed by several scientific academies (29–32). A millimetre rule and the observation of jaw movement patterns are enough to intercept a restriction in mouth opening (1). As for the differential diagnosis of joint pathologies that may cause an alteration of jaw movements patterns, a clinical evaluation performed by a trained investigator has a good diagnostic agreement for the two main groups of joint disorders (disc displacements, inflammatory-degenerative disorders) when compared with the standard of reference among the imaging techniques (i.e. magnetic resonance) (100, 113), and only long-lasting disc displacement without reduction and without functional limitation is hard to diagnose with clinical assessment alone (114). When compared with magnetic resonance findings, accuracy of clinical diagnosis of disc displacement with reduction ranged between 79% and 90% among different studies (113, 115, 116), while it ranged between 65% and 89% for cases of disc displacement without reduction (113–115, 117), and it is about 80% for TMJ pain (100). As for muscle disorders, the main symptom of which is pain, the absence of a gold standard instrument for pain rating makes clinical evaluation itself the most useful diagnostic approach (118), even if a low intra- and interexaminer reliability of findings from palpation of some muscle sites, viz., digastrics and lateral pterygoid areas, have been reported (90, 91).
There is now a consistent amount of literature in support of the reliability and accuracy of many clinical examination procedures, if they are standardised and performed by calibrated operators (119). Several studies also suggest that calibration of the examiners is not hard to achieve (120) and leads to the achievement of acceptable to excellent levels of inter-examiners reliability for all the main clusters of TMD symptoms (121, 122).
In summary, the diagnosis of TMD is clinical, appropriately selected imaging techniques should be reserved to a minority of cases (i.e. patients non-responding to common conservative treatments; surgical planning, traumatic events), while electronic devices provide nothing more than ancillary documentation.
Table 1. Summary of findings from systematic reviews on TMD diagnosis (PubMed search, 9 November 2009)
TMD treatment
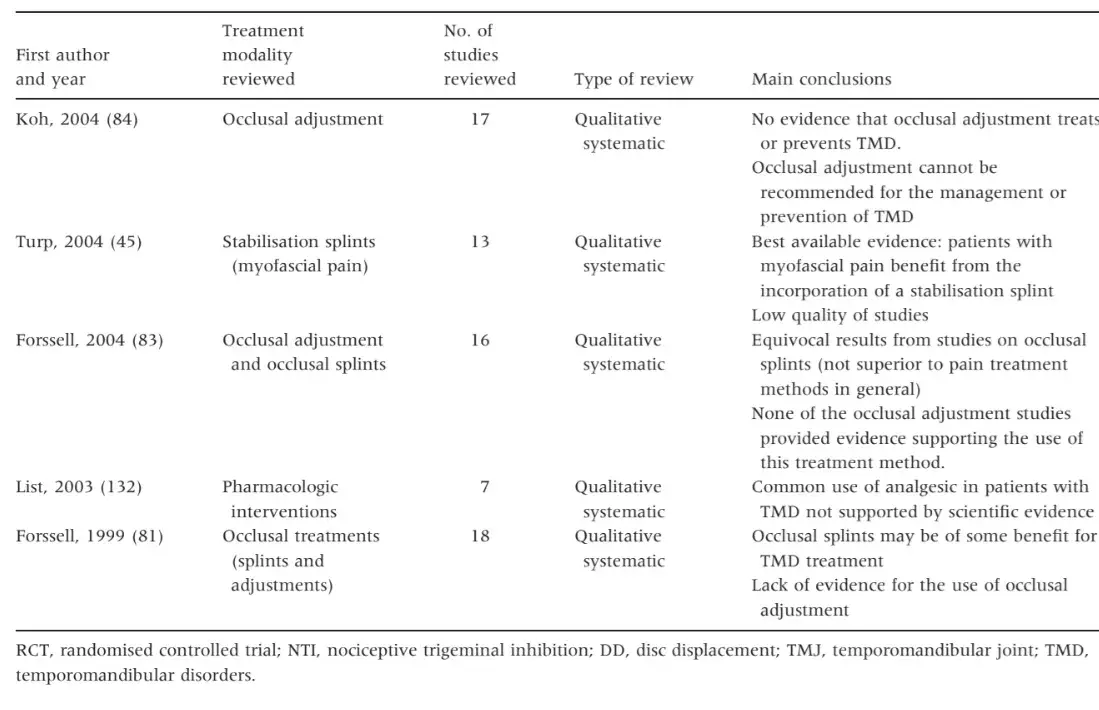
Systematic reviews on TMD treatments covered the arguments of the effectiveness of several treatment modalities, viz., occlusal treatments (n = 5) (45, 81, 83, 84, 123), orthognathic surgery (n = 2) (124, 125), arthrocentesis (n = 2) (125, 126), NTI-tss devices (n = 1) (127), simple versus multimodal therapies (n = 1) (128), any intervention’s effect on quality of life (n = 1) (129), exercise and relaxation therapy (n = 1) (130), physical therapy (n = 1) (131), pharmacological therapy (n = 1) (132), total TMJ prosthesis (n = 1) (27) (Table 2).
Findings from systematic reviews on TMD treatment are hard to discuss and extrapolation of clinically useful information is complicated by the poor methodological quality of the reviewed studies. Nonetheless, two main lines of evidence can be drawn.
First, as an evidence coming from at least three qualitative systematic reviews (81, 83, 84), occlusal adjustment cannot be recommended for the management or prevention of TMD. Such data can be considered conclusive because of the consistency of findings from the three reviews, and thanks to the relatively high number of trials, mainly coming from works of the Scandinavian schools, in which occlusal adjustment had been tested against active controls, passive controls and placebo. Patients treated with occlusal adjustments did not show any superior improvement in clinical outcome variables with respect to any other comparison group, thus suggesting that irreversible occlusal interventions are not justified for TMD pain relief or jaw function improvement. These findings dismantled the old concept of ‘occlusal finalisation’, according to which occlusion of patients with TMD had to be re-equilibrated by means of extensive prosthodontic or orthodontic rehabilitations after a presumptive ‘therapeutic’ occlusal position had been recorded. Such information is surely useful at the individual level, because TMD practitioners have to be conscious that there is no reason to provide irreversible changes to dental occlusion with the sole scope to achieve TMD symptoms improvement.
Second, multimodal therapies incorporating behavioural and educational strategies seem to offer more benefit than a single-treatment approach. Such suggestion is mostly valid for patients with high psychological distress, who can take advantage from the available cognitive-behavioural techniques in their attempt to cope with pain (128). This information is also valid at the single individual level, because it helps clinicians remembering, for example, to spend time with their patients, listen carefully to their complaints and give them all the needed reassurances.
As for oral appliances, which are the most widely diffused therapeutic modality for TMD, evidence for their subjective effectiveness seems to be supported by the systematic reviews (45, 81, 83, 123), but they are not unequivocally superior to either treatments. Oral appliances have been also the subject of a recent comprehensive review (133), which suggested that many of the available types of splints and appliances may be reasonably efficacious in the clinical setting, even though the actual mechanism through which they provide pain relief are not well known. This observation introduces another paradoxical aspect of the literature on TMD treatment, that is, therapies give a high subjective improvement in the majority of patients, independently by the rationale for using a specific approach.
In summary, literature data seem to suggest that several treatment approaches share a good therapeutic effectiveness and allow symptoms’ control in the majority of cases. Nevertheless, the actual mechanisms of action are often unknown, especially at the single patient level, and the identification of the best treatment modality for each TMD group represents a main target for future researches. In view of these considerations, there is no doubt that the most suitable approach to the large majority of patients with TMD is represented by the adoption of conservative and reversible management strategies.
Table 2. Summary of findings from systematic reviews on TMD treatment (PubMed search, 9 November 2009)
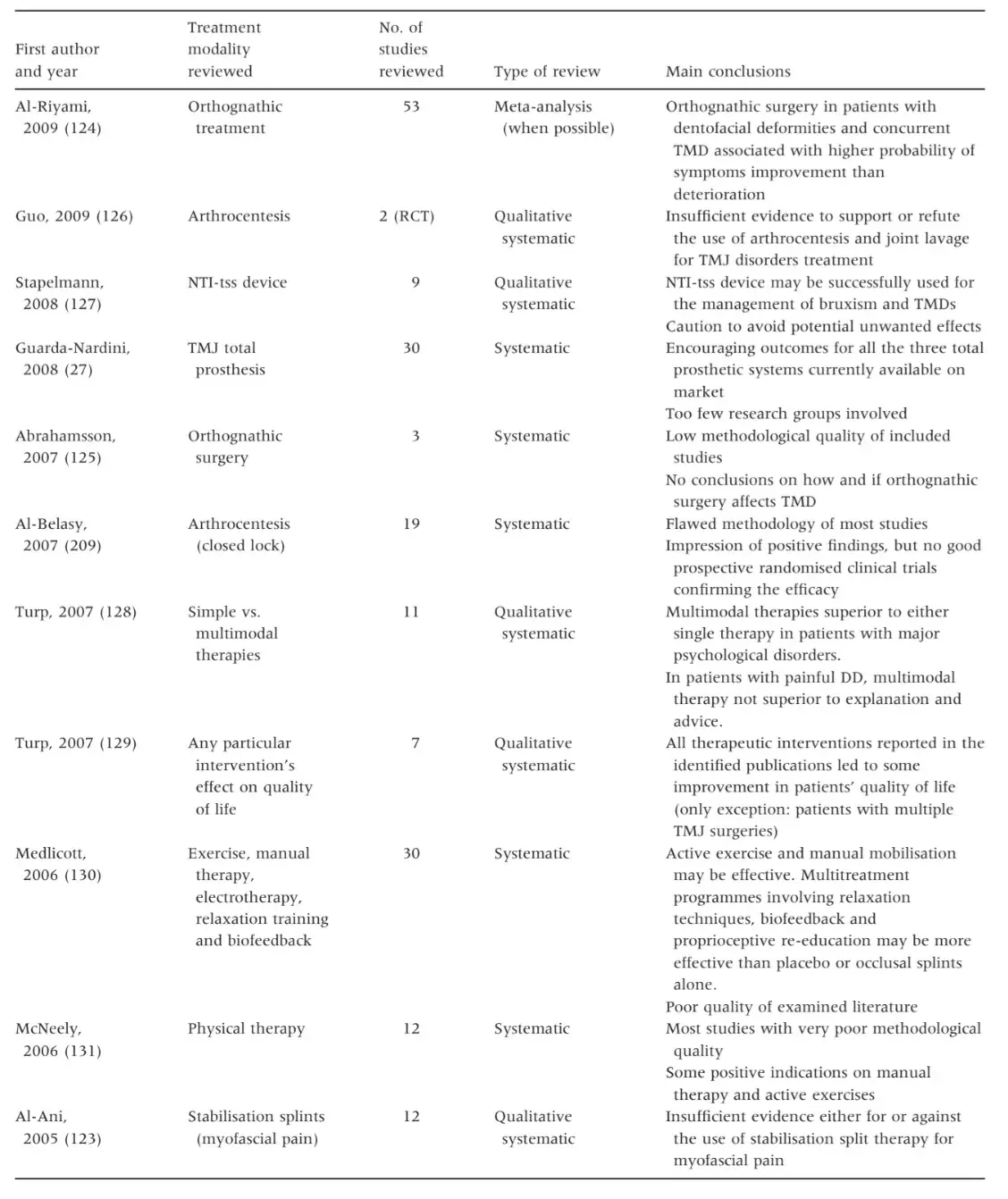
Table 2. (Continued)
Medicolegal considerations
The medicolegal approach to pathologies characterised by a multifactorial etiopathogenesis and a variety of symptoms, such as TMD, is more complex than in conditions for which a known causal factor can be recognised. The medical legal specialist has to work together with a TMD expert in the attempt to verify a cause-and-effect relationship according to the classical law medicine criteria. This consideration applies to cases of dental malpractice as well as traumatic injuries and affects both diagnostic and therapeutic aspects. This means that the decision of when a claim for malpractice or injury-related damage can be admitted and which treatments can be refunded is often a delicate task.
The need for the selection of high-qualified TMD experts contrasts with the absence of an academic TMD specialty in most countries of the world (55, 134). Thus, it is recommendable that TMD experts for legal advices are selected among recognised international personalities (international authors and editorial boards’ members) and academic or private practice professionals with demonstrable up-to-date knowledge (continued education) (55, 135).
The selection of a qualified advisor should be of invaluable help to keep the process of medicolegal assessment within the boundaries of evidence-based guidelines, which have a relative value at single subject’s level (disease versus patient) but are fundamental expressions of scientific synthesis and indicators of good practice (136). From a practical viewpoint, there are at least two main types of TMD-related legal issues: malpractice claims and trauma injuries.
Malpractice claims
Malpractice means failing to meet the accepted standard of practice, viz., the degree of skill and knowledge that would be expected by any reasonable provider in the profession under similar circumstances (55, 137, 138).
The standard of care for individual cases is decided by courts’ advisors, and there are different laws regulating the medical jurisprudence in the various countries, the discussion of which goes far beyond the scopes of this article, but it seems to be logical that the standards of practice in medicine and dentistry as well as legal medicine should ideally reflect scientific knowledge and science-based methods. For this reason, any practitioner who fails to follow the above-summarised principles in the management of patients with TMD has to be conscious of the potential legal consequences of his conduct.
Iatrogenic issues.
Research data provided very few information on the risk for iatrogenic onset of TMD symptoms during or after other dental treatments. The majority of helpful observations came from a series of review articles on the redefinition of some occlusal concepts in relation to orthodontics, prosthodontics and TMD (139–141). The transient occurrence of joint click sounds or TMJ ⁄ muscle pain in the course of orthodontic or prosthetic rehabilitations cannot be considered a pathological marker per se, and no increased risk for TMD in relation to orthodontics (142) or prosthetic treatments (143, 144) has been shown. Notwithstanding that, it needs to be pointed out that occlusion should be managed with care in all cases of extensive oral rehabilitations, and clinicians must be conscious that all positional changes of the interarch relationship have to be kept within reasonable limits (47). At present, there is no accurate method to predict an individual’s response to the demands for adaptation related with acute extensive occlusal changes (i.e. mandibular repositioning, increases of vertical dimension of occlusion) (145–147). Moreover, it should be remembered that the negative association which was shown between TMD and occlusion refers to natural occlusal features (44) or to small acute interferences introduced in healthy subjects (79, 80), while there is some experimental evidence that small acute changes might provoke transient symptoms in subjects with a history of past TMD (148). Clinically, this means that all techniques suggesting that mandibular repositioning or muscular deprogramming are required to restore an individual’s ideal occlusion are at risk for iatrogenic onset of TMD-like symptoms when the requested changes fall outside of the individually unknown range of adaptation (149). In spite of the above-mentioned considerations, the event of a TMD-like damage after oral rehabilitations in healthy individuals is unlikely because of the usually high accommodation skills of the stomatognathic system (150) and, consequently, prevalence of such cases in the medical legal literature on TMD is very Low (151).
Overtreatment of TMD with irreversible therapies. By contrast, an event to be taken into consideration for its potential legal consequences is the adoption of unnecessary and excessive therapies to treat these disorders, viz., overtreatment (55, 138). The TMD literature is plenty of studies reporting examples of unnecessary therapies, the most striking of which is represented by TMJ surgery performed without a rationale indication (i.e. disc repositioning surgery), which often lead to multiple failed interventions, as described by several reviews on the argument (26, 27).
Many studies showed beyond any reasonable doubt that the long-term course of the majority of TMD signs and symptoms is favourable, if treated conservatively or even untreated (152–154). A cognitive-behavioural treatment provided in the early stages of TMD onset reduces significantly the long-term use of medications and social costs for pain relief in patients with TMD (16, 17). There are also many suggestions that the tiveness of TMD treatments may be, at least to a certain degree, unspecific and independent by the kind of provided therapy and may be predicted only in part by clinical factors (155–157), thus pointing out the need to identify other predictors of treatment outcome among factors belonging to one individual’s psychosocial sphere. Such observations led to cautionary statements to improve the definition of treatment success in the field of TMD clinics, because an apparent success may be actually as a result of a number of reasons (fluctuation and self-limitations of symptoms, regression to the mean, placebo effect, psychosocial issues) which are not related with specific treatment effects (158, 159).
Positive outcomes achieved with the adoption of invasive and irreversible occlusal approaches are not related with a specific treatment effect and must be avoided. Unfortunately, clinicians pursuing definitive occlusal therapies and patients receiving such treatments may be in good faith when they attribute a successful outcome to their specific interventions on dental occlusion; thus, those practitioners’ actions are unlikely to have medicolegal consequences because of the potentially high rate of satisfaction reported by their patients. In view of that, it seems that ethical rather than medicolegal considerations should represent the focus for discussion. In the near future, a strong improvement in the science transfer process between the researchers and practitioners communities is the first necessary step to increase educational levels in the social and ethical principles associated with the art of health care supplying according to the currently available state-of-the art (42).
Treating minor or subclinical TMD phenomena with aggressive interventions. Notwithstanding the concern of over-treatment provided to patients with TMD, in the daily clinical practice, the most frequent example of over-treatment is represented by treatments provided to subjects who are not treatment-needing subjects. There is a quantity of subjects presenting mild signs (i.e. intermittent click sounds) or symptoms (i.e. single episode of mild tenderness in the TMJ area) who actually do not need active treatment but only need to be passively observed without performing any active interventions (30, 32, 158, 159). Examples of the potentially harmful consequences of such actions may be found in the surgical literature describing multiple interventions, often ending in the delivery of TMJ prostheses, to ‘non-patients’ with unspecified internal derangements which might have received benefit from a simple ‘wait and see’ approach (27).
Providing any treatment to such patients is an example of potential overtreatment and is, once again, a source of bias in the analysis of success rates in the clinical as well as the research settings caused by the mildness, self-limitation and often non-pathological nature of those symptoms. Negative examples of apparent ‘treatment success’ in populations of subjects with undefined symptoms are still a problem in the TMD literature (160–162). Moreover, some advocacies (163) still exist to suggest clinicians pursuing technologically guided ‘ideal’ occlusal rehabilitations to treat some so-called dysfunctional subjects who are clinically asymptomatics and are diagnosed as dysfunctionals based on instrumental examinations that in some cases give up to an 80% of false-positive results (164).
These considerations lend support to the importance of a well-documented clinically based diagnosis before starting any TMD treatment. There is much evidence to suggest caution with the management of patients with TMD (165), and the first cases of unnecessary (over)treatment coming to courts have been published in the international literature (166). In view of these observations, the medical legal specialist must be aware of the fact that overtreatment is a potential problem in the TMD clinics, and the ethical and legal implications related with the adoption of irreversible, expensive, unnecessary and often unsuccessful treatments should be discussed in future articles.
There are additional details about temporomandibular disorders treatment you can gain in our course "Treatment of severe forms of TMJ diseases" by David Angelo and Sylvain Chamberland.
TMD prevention.
The most unethical malpractice procedure in the TMD field concerns the proposal of interventions purported to prevent TMD. Some early orthodontic literature seemed to suggest that the elimination of supposed abnormalities of dental occlusion by occlusal adjustment or by orthodontic treatment may be of some benefit to reduce the risk for pain onset in the face and head region (167, 168), even if other orthodontic reports suggested caution in interpreting results because of the fluctuating nature of symptoms, which is even more evident in the growing patients (169). Notwithstanding that, studies over a two-decade follow-up (170) as well as systematic reviews of the literature excluded the existence of some beneficial effects of early irreversible occlusal changes on the late onset of TMD symptoms (84, 171). Thus, the current state-of-the-art position still states that occlusal adjustment and orthodontic treatment neither reduce nor increase the risk for TMD onset (139, 142, 172).
As a summary of the earlier considerations, it should be concluded that all invasive and irreversible occlusal treatments aiming at the sole scope to treat or even prevent TMD must be viewed as deflections from the present line of evidence in the field of TMD practice and must be firmly discouraged.
Trauma injuries
Diagnostic aspects are important in the case of traumatic injuries as well. Facial injuries may be directly (i.e. condylar fracture following a violent chin trauma) or indirectly (i.e. TMJ effusion following a car accident cervical whiplash) involved in the onset of TMD symptoms.
The effects of direct trauma on the TMJ are well documented in the literature and depend upon the intensity, direction and area of the impact (173, 174), ranging from mild contusions to severe and rarely described cases of condyle penetration into the middle cranial fossa (175). Contusions are provoked by direct trauma of low to moderate intensity and may affect the joint on the same side of the impact, the contralateral joint, or both, in accordance with force vectors which are described in the maxillofacial surgery literature (85). Contusions are characterised by post-traumatic phlogosis and intra-articular effusion; rarely, they can provoke blood effusion within the retrodiscal area that may hesitate in joint fibrosis and reduced mobility. The severity of damage because of contusive traumas is variable, and animal models showed that direct TMJ contusions can provoke histological changes in the disc as well as in the synovial fluid. These alterations may lead to an increased joint viscosity and to a partial loss of the viscoelastic properties of the disc, which may be pre-disposed to permanent damage (176, 177). Moreover, literature data reported that TMJ ankylosis recognises a traumatic aetiology in up to 98% of cases (178, 179). Thus, even trauma of a low intensity is worthy to be considered as potential risk factors for TMD. Temporal bone fractures with intra-cranial con- dylar dislocation are rare events; one single case of bilateral and 48 cases of monolateral condylar dislocation into the middle cranial fossa have been described in the literature so far (175). Such dramatic consequences are related to high-intensity trauma characterised by a co-axial force vector with respect to the mandibular ramus, which can bear strong axial loads without fracturing. Fractures of the TMJ condyle are responsible for up to 35% of mandibular fractures in the adults and 30% in the children, and the onset of TMD symptoms may appear within a variable time period after fractures (180). Condylar fractures require different treatment approaches in relation to the age of the patient and the type of the fracture (180–182), thus requiring much attention in a medical legal setting.
Iatrogenic trauma in the TMJ area includes rare events related to dental or TMJ surgery procedures, such as facial nerve paralysis because of an erroneous surgical approach to the TMJ; maxillary artery lesions during condylectomy; TMJ dysfunction because of an incorrect surgical reduction of mandibular fractures; trauma because of forced TMJ hyperextension during endotracheal intubation; trauma because of prolonged dental treatments performed with the jaw in a forced opening position. Such situations share a high degree of severity, but do not have the same medicolegal consequences and are a concrete matter of legal debate.
Indeed, damage in the TMJ area during high-risk interventions which are needed to safeguard the patient’s systemic health are unlikely to force a profile of professional liability, and the benefit-to-side effects ratio is positive even in the presence of some post-surgical complications. The only example of dentistry-related trauma to the TMJ is provided by the sometimes described long-lasting surgical or rehabilitation procedure with the jaw forced open, but they are actually hard to relate causally to a late-onset TMD.
Indirect trauma is often called into cause in claims for TMD damage, even though the existence of the so-called TMJ whiplash is still much debated (183). Some studies suggested the co-occurrence of a man- dibular whiplash with a car-accident cervical whiplash (184, 185). In case of such event, it was suggested that the extreme hypertranslation of the condyle out of the glenoid fossa might lengthen or even stretch the posterior attachment and the ligaments, both at the medial and lateral levels. This condition seems to be a predisposing factor for disc displacement and might be associated with post-traumatic joint tenderness and effusion, even though the frequency of the involvement of the stomatognathic system after an indirect trauma and the actual link of causality between whiplash and TMD have to be clarified yet (55, 183).
The literature seems to suggest that such a mechanism is not likely to provoke severe TMJ damage in healthy joints, while it may act as a triggering factor for preexisting underlying diseases which were asymptomatic prior to the car-accident whiplash (183).
Reflections on the medicolegal assessment
In the medical legal setting, efforts are directed towards the search for a cause-and-effect relationship between two events, by verifying the positive endorsement of a series of criteria of causality, viz., temporality, dose–response, strength and consistency of association, biological plausibility, experimental evidence, specificity, analogy, coherence (186, 187). Actually, positive endorsement of the majority of criteria is usually enough to prove a causal relationship beyond any reasonable doubt, and it is usually a clinicians’ duty to prove the absence of causal relationship between an intervention and the supposed negative consequences (85). These considerations justify the marked increase of claims for professional liability which characterised many medical specialties (151, 188–190).
In the field of TMD clinics, the trends which have been characterising the doctor–patient relationship in recent years, to the point that it may be viewed as a contract between a health provider and a health receiver (191), may have reflections in the everyday practice. At present, there is not a universally accepted position on the clinician’s duties in pain medicine, and laws regulating the different countries are an obstacle to the adoption and description of a internationally recognised position, but it seems to be logical to assume that clinicians who manage pain patients, such as those with TMD, are obliged to warrant any effort to pursue pain relief, viz., obligation to treat patients in accordance with the reference protocols, and not to warrant pain relief per se, viz., obligation to provide relief from pain.
Thus, clinicians practicing outside from the EBM boundaries and treating TMD patients with invasive protocols based on personal beliefs are at risk for malpractice claims and may be forced to justify their actions in courts. Such observation is mostly valid if one considers that the large majority of patients with TMD seen by general practitioners are represented by mildsymptomatic patients who have not the features of chronic pain sufferers attending tertiary centres (192). This means that the adoption of irreversible treatments to manage mild symptoms which have been shown to fluctuate and remit spontaneously in many cases (193–195) is a dangerous example of unnecessary overtreatment, and jurisprudence will likely be called into cause to regulate this issue in a near future.
The problem of overtreatment, and in particular those kinds of financially driven overtreatments related to conflicts of interests, is intrinsic in the medical profession per se, which is based upon the unselfish service to satisfy the interests of those served and not self-interest (196). Notwithstanding that, overtreatment is rarely perceived as a problem by the patients, thus failing to fulfil the pre-requisite for the onset of litigation claims. The field of TMD practice as well as other pain treatment areas is characterised by a high diffusion rate of quackery medicine (197), and the diffusion of state-of-the-art practices should surely benefit from more controlled laws and regulations on their use. Unfortunately, at present, the focus of discussion is a matter of ethical rather than legal or medicolegal concern, so professional liability claims for TMD malpractice are apparently reserved to a small minority of the total amount of cases which should actually deserve attention (151).
Trauma injuries are the only example of a TMD-related issue for which a classical process of medicolegal reasoning may be followed. Once established that a trauma or a practitioner’s act have a direct causal relation with TMD symptoms, the medical legal specialist is asked to rate one patient’s impairment and to suggest the needed (and refundable) therapies. This latter aspect is mainly related with the above-described standards of care for TMD management, while the former is actually open to several interpretations, because of the biopsychosocial nature of TMD. It is well recognised in the literature that TMD involve the biopsychosocial sphere as well, with chronic pain and functional limitation representing possible sources of interference with daily activities (198–200). In the research setting, pain-related impairment is rated by means of validated scales which rely on subjective parameters of evaluation (201, 202). In the medical legal setting, a psychosocial assessment is not easily acceptable and often ignored, even though interferences with daily activities represent patients’ chief complaint in the majority of severe painful TMD cases (203–206). For this reason, impairment evaluation in the medical legal setting is preferably based on objective parameters, such as jaw range of motion (29, 55, 135). Recent works describing the properties of measures to assess disablement and the present evidence to support their use in both the research and clinical setting (207, 208) will contribute to the introduction of dedicated measures as part of routine medicolegal assessments as well. On the way towards this achievement, the recent validation articles on the RDC ⁄ TMD axis II instruments provide interesting demonstrations of construct validity to detect the amount of disability related to psychosocial, and not physical, issues. Indeed, despite being advocated in some legal settings as the only objective measurement of stomatognathic function, measurement of jaw range of motion in millimetres are hard to accept as the standard of reference for the evaluation of the levels of jaw function impairment in the legal setting, as it represents a forced interpretation of the biological model.
Thus, efforts should be made to design medical legal classifications taking into account for the complex biopsychosocial aspects of TMD assessment.
If you enjoyed reading the article, you can also find more in-depth information about TMJ disease and their treatment in our course "Evidence-based treatment of TMJ dysfunction".
CONCLUSIONS
Temporomandibular disorders are a frequent finding in cases of facial trauma or dental malpractice, and legal claims for TMD damage have been increased over the years. TMD assessment in the medical legal setting is complicated by the peculiarities of these disorders, whose symptoms are heterogeneous, fluctuant and recognise a multifactorial origin. Despite the legal aspects of the dental profession are gaining a growing attention, there is a paucity of literature dealing with patients with TMD assessment, so this article was intended to summarise up-to-date evidence-based knowledge in this field and to give some possible suggestions for the TMD-related legal profession.
The following observations can be drawn:
The medicolegal approach to TMD should be based on a thorough examination of the peer-reviewed TMD literature, and, in the absence of a worldwide recognised academic TMD specialty, TMD experts should be selected among qualified professionals (international authors; academic personalities; members of peer-reviewed journals editorial boards; private practitioners with recognised experience and continued education).
Some basic diagnostic and therapeutic concepts have been well demonstrated in the TMD literature and must be applied to both the clinical and medical legal settings: (i) TMD diagnosis must be clinical (currently available standardised classification schemes) and ⁄ or radiological (magnetic resonance and, when needed, computerised tomography); (ii) TMD treatment should be directed to symptoms management, and be as reversible, conservative and non-invasive as possible; (iii) electronic instruments and devices have no utility at either diagnostic or therapeutic level, so they should have poor value in the medical legal setting as well.
A comprehensive medicolegal approach should take into account for the complex biopsychosocial nature of TMD and strategies for standardising rates of TMD-related impairment which comprehend an evaluation of pain interference on daily activities should be studied in future researches.
Author's information
D. MANFREDINI
M. B. BUCCI
F. MONTAGNA
L. GUARDA-NARDINI
Acknowledgments
This manuscript was prepared with the help and on behalf of the Executive Board of the Italian Society of Legal Medicine and Dentistry (SIOLA).
References
Okeson JP. The classification of orofacial pains. Oral Maxillofac Surg Clin N Am. 2008;20:133–144.
Laskin DM. Etiology of the pain-dysfunction syndrome. J Am Dent Assoc. 1969;79:147–153.
Dworkin SF. Perspectives on the interaction of biological, psychological and social factors in TMD. J Am Dent Assoc. 1994;125:856–863.
McNeill C. History and evolution of TMD concepts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:51–60.
Greene C. Concepts of TMD etiology: effects on diagnosis and treatment. In: Laskin DM, Greene CS, Hylander WL, eds. TMDs. An evidence-based approach to diagnosis and treatment. Chicago: Quintessence Publishing, 2006:219–228.
Schiffmann E, Fricton JR, Harley D, Shapiro BL. The prevalence and treatment needs of subjects with temporo- mandibular disorders. J Am Dent Assoc. 1990;120:295–304.
List T, Dworkin SF. Comparing TMD diagnoses and clinical findings at Swedish and US TMD center using Research Diagnostic Criteria for Temporomandibular Disorders. J Orofac Pain. 1996;10:240–253.
Lobbezoo F, Drangsholt M, Peck C, Sato H, Kopp S, Svensson P. Topical review: new insights into the pathology and diagnosis of disorders of the temporomandibular joint. J Orofac Pain. 2004;18:181–191.
Manfredini D, Chiappe G, Bosco M. Research Diagnostic Criteria for Temporomandibular Disorders (RDC ⁄ TMD) axis I diagnosis in an Italian patients population. J Oral Rehabil. 2006;33:551–558.
Al-Jundi MA, John MT, Setz JM, Szentperry A, Kuss O. Meta-analysis of treatment need for temporomandibular disorders in adult nonpatients. J Orofac Pain. 2008;22:97–107.
Manfredini D, Guarda-Nardini L. TMD classification and epidemiology. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:25–40.
Dao TT, Lavigne GJ. Oral splints: the crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med. 1998;9:345–361.
Raphael K, Marbach JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc. 2001;132:305–316.
Nicolakis P, Erdogmus B, Kopf A, Nicolakis M, Piehslinger E, Fialka-Moser V. Effectiveness of exercise therapy in patients with myofascial pain dysfunction syndrome. J Oral Rehabil. 2002;29:362–368.
Gavish A, Winocur E, Astandzelov-Nachmias T, Gazit E. Effect of controlled masticatory exercise on pain and muscle performance in myofascial pain patients: a pilot study. Cranio. 2006;24:184–190.
Gardea MA, Gatchel RJ, Mishra KD. Long-term efficacy of biobehavioral treatment of temporomandibular disorders. J Behav Med. 2001;24:341–359.
Gatchel RJ, Stowell AW, Wildenstein L, Riggs R, Ellis E. Efficacy of an early intervention for patients with acute TMD-related pain: a one-year outcome study. J Am Dent Assoc. 2006;137:339–347.
De Laat A, Stappaers K, Papy S. Counseling and physical therapy as treatment for myofascial pain of the masticatory system. J Orofac Pain. 2003;17:42–49.
Dionne RA. Pharmacologic treatment of acute and chronic orofacial pain. Oral Maxillofac Surg Clin North Am. 2000;12:309–320.
Plesh O, Curtis D, Levine J, Mccall WD. Amitriptyline treatment of chronic pain in patients with temporomandibular disorders. J Oral Rehabil. 2000;27:834–841.
Manfredini D, Romagnoli M, Cantini E, Bosco M. Efficacy of tizanidine hydrochloride in the treatment of myofascial face pain. Minerva Med. 2004;95:165–171.
Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49: 1163–1167.
Guarda-Nardini L, Stifano M, Brombin C, Salmaso L, Manfredini D. A one-year case series of arthrocentesis with hyaluronic acid injections for temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e14–e22.
Manfredini D, Bonnini S, Arboretti R, Salmaso L. Temporomandibular joint osteoarthritis: an open label trial of 76 patients treated with arthrocentesis plus hyaluronic acid injections. Int J Oral Maxillofac Surg. 2009;38:827–834.
Dolwick MF, Dimitroulis G. Is there a role for temporomandibular joint surgery? Brit J Oral Maxillofac Surg. 1994;32: 307–313.
Dimitroulis G. The role of surgery in the management of disorders of the temporomandibular joint: a critical review of the literature. Part 1. Int J Oral Maxillofac Surg. 2005;34: 107–113.
Guarda-Nardini L, Manfredini D, Ferronato G. Temporomandibular joint total replacement prosthesis: current knowledge and considerations for the future. Int J Oral Maxillofac Surg. 2008;37:103–110.
National Institute of Health Technology Assessment Conference Statement. Management of temporomandibular disorders. J Am Dent Assoc. 1996;127:1595–1603.
Phillips DJ, Gelb M, Brown CR, Kinderknecht KE, Neff PA, Kirk WS et al. American Association of Temporomandibular Joint Surgeons. Guide to evaluation of permanent impairment of the temporomandibular joint. Cranio. 1997;15:170–176.
De Boever JA, Nilner M, Orthlieb JD, Steenks MH. Recommendations by the EACD for examination, diagnosis, and management of patients with temporomandibular disorders and orofacial pain by the general dental practitioner. J Orofac Pain. 2008;22:268–278.
Davies S. EACD GDP guidelines. Dent Update. 2008;35: 210–211.
De Leeuw R. The American Academy of Orofacial Pain. Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence Publishing, 2008.
Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6: 301–355.
Lobbezoo F, van Selms MK, John MT, Huggins K, Ohrbach R, Visscher CM. Use of the Research Diagnostic Criteria for Temporomandibular Disorders for multinational research: translation efforts and reliability assessments in The Netherlands. J Orofac Pain. 2005;19:301–308.
John MT, Hirsch C, Reiber T, Dworkin SF. Translating the Research Diagnostic Criteria for Temporomandibular Disorders into German: evaluation of content and process. J Orofac Pain. 2006;20:43–52.
Khoo SP, Yap AUJ, Chan YH, Bulgiba AM. Translating the Research Diagnostic Criteria for Temporomandibular Disorders into Malay: evaluation of content and process. J Orofac Pain. 2008;22:131–138.
McNeill C. Management of temporomandibular disorders: concepts and controversies. J Prosthet Dent. 1997;77: 510–522.
Stohler C, Zarb G. On the management of temporomandibular disorders: a plea for low-tech, high-prudence therapeutic approach. J Orofac Pain. 1999;13:255–261.
Greene C. The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain. 2001;15:93–105.
Shankland WE. Temporomandibular disorders: standard treatment options. Gen Dent. 2003;51:349–355.
Pierce CJ, Weyant RJ, Block HM, Nemir DC. Dental splints prescription patterns: a survey. J Am Dent Assoc. 1995;126: 248–254.
Greene CS. Science transfer in orofacial pain. In: Lund JP, Lavigne GJ, Dubner R, Sessle BJ, eds. Orofacial pain. From basic science to clinical management. Chicago: Quintessence Publishing, 2006:281–286.
Manfredini D. Integration of research into the clinical practice. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:459–468.
Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. Cochrane Database Syst Rev. 2003;1:CD003812.
Turp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig. 2004;8:179–195.
Stohler CS. Temporomandibular joint disorders – the view widens while therapies are constrained. J Orofac Pain. 2007;21:261.
Turp JC, Greene CS, Strub JR. Dental occlusion: a critical reflection on past, present and future concepts. J Oral Rehabil. 2008;35:446–453.
Klasser GD, Greene CS. The changing field of temporomandibular disorders: what dentists need to know. J Can Dent Assoc. 2009;75:49–53.
Turp JC, Schindler HJ. Occlusal therapy of temporomandibular pain. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:359–382.
Talley RL. Assessment of temporomandibular injury and orofacial pain. J Okla Dent Assoc. 1995;86:38–41.
Stack BC. TM therapy: avoiding legal pitfalls. J Macomb Dent Soc. 1989;26:38.
Machen DE. Legal aspects of orthodontic practice: risk management concepts. Update on TMJ litigation. Part 2. Am J Orthod Dentofacial Orthop. 1989;96:524–525.
Machen DE. Legal aspects of orthodontic practice: risk management concepts. Update on TMJ litigation. Part 3. Am J Orthod Dentofacial Orthop. 1990;97:88–89.
Dobbs D. The medical legal aspects of TMD. Cranio. 1994;12:65–70.
Goldstein BH. Medical legal considerations in temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:395–399.
Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–72.
Greene CS. Orofacial pain: past and future. In: Turp JC, Sommer C, Hugger A, eds. The puzzle of orofacial pain. Integrating research into clinical management. Pain Headache, vol 15. Basel: Karger, 2007:223–235.
Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol. 1934;43:1–15.
Molin C. From bite to mind: TMD – a personal and literature review. Int J Prosthodnt. 1999;12:279–288.
Suvinen TI, Reade PC, Kemppainen P, Kononen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9:613–633.
Frost R. Applied Kinesiology: a training manual and reference book of basic principles and practices. Berkeley: North Atlantic Books, 2002:4.
Jankelson B. Neuromuscular aspects of occlusion. Effects of occlusal position on the physiology and dysfunction of the mandibular musculature. Dent Clin North Am. 1979;23: 157–168.
Nashner LM, Black FO, Wall C 3rd. Adaptation to altered support and visual conditions during stance: patients with vestibular deficits. J Neurosci. 1982;2:536–544.
Lund JP, Lavigne G, Feine JS, Goulet JP, Chaytor DV, Sessle BJ et al. The use of electronic devices in the diagnosis and treatment of temporomandibular disorders. J Can Dent Assoc. 1989;55:749–750.
Baba K, Tsukiyama Y, Yamazaki M, Clark GT. A review of temporomandibular disorder diagnostic techniques. J Prosthet Dent. 2001;86:184–194.
Armijo Olivo S, Bravo J, Magee DJ, Thie NMR, Major PW, Flores-Mir C. The association between head and cervical posture and temporomandibular disorders: a systematic review. J Orofac Pain. 2006;20:9–23.
Armijo Olivo S, Magee DJ, Parfitt M, Major P, Thie NMR. The association between the cervical spine, the stomatognathic system, and craniofacial pain: a critical review. J Orofac Pain. 2006;20:271–287.
Suvinen TI, Kemppainen P. Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J Oral Rehabil. 2007;34:631–644.
Perinetti G, Contardo L. Posturography as a diagnostic aid in dentistry: a systematic review. J Oral Rehabil. 2009;36: 922–936.
Michelotti A, Farella M. Malocclusion and body posture. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:283–294.
Stohler CS. Taking stock: from chasing occlusal contacts to vulnerability alleles. Orthod Craniofac Res. 2004;7: 157–161.
Stohler CS. The end of an era: orofacial pain enters the genomic age. In: Tu¨rp JC, Sommer C, Hugger A, eds. The puzzle of orofacial pain. Integrating research into clinical management. Pain headache, vol 15. Basel: Karger, 2007:236–247.
Merskey H. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Pain. 1986;3:1–8.
Dworkin SF, Massoth DL. Temporomandibular disorders and chronic pain: disease or illness? J Prosthet Dent. 1994;72: 29–38.
Von Korff M, Dunn KM. Chronic pain reconsidered. Pain. 2008;13:267–276.
De Laat A. TMD as a source of orofacial pain. Acta Neurol Belg. 2001;101:26–31.
Pullinger AG, Seligman DA. Quantification and validation of predictive values of occlusal variables in temporomandibular disorders using a multifactorial analysis. J Prosthet Dent. 2000;83:66–75.
Landi N, Manfredini D, Tognini F, Romagnoli M, Bosco M. Quantification of the relative risk of multiple occlusal variables for muscle disorders of the stomatognathic system. J Prosthet Dent. 2004;92:190–195.
Michelotti A, Farella M, Gallo LM, Veltri A, Palla S, Martina R. Effect of occlusal interference on habitual activity of human masseter. J Dent Res. 2005;84:644–648.
Michelotti A, Farella M, Steenks MH, Gallo LM, Palla S. No effect of experimental occlusal interferences on pressure pain thresholds of the masseter muscles in healthy women. Eur J Oral Sci. 2006;114:167–170.
Forssell H, Kalso E, Koskela P, Vehmanen R, Puukka P, Alanen P. Occlusal treatments in temporomandibular disorders: a qualitative systematic review of randomized controlled trials. Pain. 1999;83:549–560.
Clark GT, Tsukiyama Y, Baba K, Watanabe T. Sixty-eight years of experimental occlusal interference studies: what have we learned? J Prosthet Dent. 1999;82:704–713.
Forssell H, Kalso E. Application of principles of evidence-based medicine to occlusal treatment for temporomandibular disorders: are there lessons to be learned? J Orofac Pain. 2004;18:9–22.
Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. J Oral Rehabil. 2004;31:287–292.
Bucci MB. Ethical and legal considerations. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:469–482.
Limchachaina N, Petersson A, Rohlin M. The efficacy of magnetic resonance imaging in the diagnosis of degenerative and inflammatory temporomandibular joint disorders: a systematic review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:521–536.
Koh KJ, List T, Petersson A, Rohlin M. Relationship between clinical and magnetic resonance imaging diagnoses and findings in degenerative and inflammatory temporomandibular joint diseases: a systematic literature review. J Orofac Pain. 2009;23:123–139.
Hussain AM, Packota G, Major PW, Flores-Mir C. Role of different imaging modalities in assessment of temporomandibular joint erosions and osteophytes: a systematic review. Dentomaxillofac Radiol. 2008;37:63–71.
Manfredini D, Guarda-Nardini L. Ultrasonography of the temporomandibular joint: a literature review. Int J Oral Maxillofac Surg. 2009;38:1229–1236.
Turp JC, Arima T, Minagi S. Is the posterior belly of the digastrics muscle palpable? A qualitative systematic review of the literature. Clin Anat. 2005;18:315–322.
Turp JC, Minagi S. Palpation of the lateral pterygoid region in TMD – where is the evidence? J Dent. 2001;29:475–483.
Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359:2693–2705.
Farella M, Michelotti A, Steenks MH, Romeo R. The diagnostic value of pressure algometry in myofascial pain of jaw muscles. J Oral Rehabil. 2000;27:9–14.
Mohl ND. Reliability and validity of diagnostic modalities for temporomandibular disorders. Adv Dent Res. 1993;7: 113–119.
Klasser GD, Okeson J. The clinical usefulness of surface electromyography in the diagnosis and treatment of temporomandibular disorders. J Am Dent Assoc. 2006;137:763–771.
Baba K, Ono Y. Instrumental approach. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:223–236.
Perinetti G. Dental occlusion and body posture: no detectable correlation. Gait Posture. 2006;24:165–168.
Perinetti G. Temporomandibular disorders do not correlate with detectable alterations in body posture. J Contemp Dent Pract. 2007;8:60–67.
Emshoff R, Puffer P, Rudisch A, Gassner R. Temporomandibular joint pain: relationship to internal derangement type, osteoarthrosis, and synovial fluid mediator level of tumor necrosis factor-a. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:442–449.
Manfredini D, Tognini F, Zampa V, Bosco M. Predictive value of clinical findings for temporomandibular joint effusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:521–526.
Stegenga B. Osteoarthritis of the temporomandibular joint organ and its relationship to disc displacement. J Orofac Pain. 2001;15:193–205.
Nitzan D, Benoliel R, Heir G, Dolwick F. Pain and dysfunction of the temporomandibular joint. In: Sharav Y, Benoliel R, eds. Orofacial pain and headache. Philadelphia: Mosby-Elsevier, 2008:149–192.
Manfredini D, Basso D, Arboretti R, Guarda-Nardini L. Association between magnetic resonance signs of temporomandibular joint effusion and disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:266–271.
Stegenga B, De Bont LGM, Boering G, van Willigen JD. Tissue responses to degenerative changes in the temporomandibular joint: a review. J Oral Maxillofac Surg. 1991;49:1079–1088.
Tasaki MM, Westesson PL. Temporomandibular joint: diagnostic accuracy with sagittal and coronal MR imaging. Radiology. 1993;186:723–729.
Westesson PL. Reliability and validity of imaging diagnosis of temporomandibular joint disorders. Adv Dent Res. 1993;7: 137–151.
Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson A. CT and MR of the temporomandibular joint: comparison with autopsy specimens. Am J Roentgenol. 1987;148:1165–1171.
Nebbe B, Brooks SL, Hatcher D, Hollender LG, Prasad NGN, Major PW. Magnetic resonance imaging of the temporomandibular joint: interobserver agreement in subjective classification of disk status. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:102–107.
Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol. 2007;36:192–197.
Pullinger AG, Hollender L, Solberg WK, Petersson A. A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent. 1985;53:706–713.
Epstein JB, Caldwell J, Black G. The utility of panoramic imaging of the temporomandibular joint in patients with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:236–239
Petersson A. Imaging techniques. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:207–222.
Orsini MG, Kuboki T, Terada S, Matsuka Y, Yatani H, Yamashita A. Clinical predictability of temporomandibular joint disc displacement. J Dent Res. 1999;78:650–660.
Yatani H, Suzuki K, Kuboki T, Matsuka Y, Maekawa K, Yamashita A. The validity of clinical examination for diagnosing anterior disk displacement without reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85: 654–660.
Manfredini D, Guarda-Nardini L. Agreement between Research Diagnostic Criteria for Temporomandibular Disorders and magnetic resonance diagnoses of temporomandibular disc displacement in a patient population. Int J Oral Maxillofac Surg. 2008;37:612–616.
Yatani H, Suzuki K, Kuboki T, Matsuka Y, Maekawa K, Yamashita A. The validity of clinical examination for diagnosing anterior disk displacement with reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85: 647–653.
Paesani D, Westesson PL, Hatala MP, Tallents RH, Brooks SL. Accuracy of clinical diagnosis for TMJ internal derangement and arthrosis. Oral Surg Oral Med Oral Pathol. 1992;73: 360–363.
John MT, Dworkin SF, Mancl LA. Reliability of clinical temporomandibular disorder diagnoses. Pain. 2005;118: 61–69.
Schmitter M, Kress B, Leckel M, Henschel V, Ohlmann B, Rammelsberg P. Validity of temporomandibular disorder examination procedures for assessment of temporomandibular joint status. Am J Orthod Dentofac Orthop. 2008;133: 796–803.
Leher A, Graf K, PhoDuc JM, Rammelsberg P. Is there a difference in the reliable measurement of temporomandibular disorder signs between experienced and inexperienced examiners? J Orofac Pain. 2005;18:58–64.
List T, John MT, Dworkin SF, Svensson P. Recalibration improves inter-examiner reliability of TMD examination. Acta Odontol Scand. 2006;64:146–152.
Schiffman EL, Ohrbach R, Truelove EL, Tai F, Anderson GC, Pan W et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: Methods used to establish and validate revised axis I diagnostic algorithms. J Orofac Pain. 2010;24:63–78.
Al-Ani Z, Gray RJ, Davies SJ, Sloan P, Glenny AM. Stabilization splint therapy for the treatment of temporomandibular myofascial pain: a systematic review. J Dent Educ. 2005;69:1242–1250.
Al-Riyami S, Cunningham SJ, Moles DR. Orthognathic treatment and temporomandibular disorders: a systematic review. Part 2. Signs and symptoms and meta-analyses. Am J Dentofac Orthod Dentofacial Orthop. 2009;136:626.
Abrahamsson C, Ekberg E, Henrikson T, Bondemark L. Alterations of temporomandibular disorders before and after orthognathic surgery: a systematic review. Angle Orthod. 2007;77:729–734.
Guo C, Shi Z, Revington P. Arthrocentesis and lavage for treating temporomandibular joint disorders. Cochrane Data-base Syst Rev. 2009;4:CD004973.
Stapelmann H, Turp JC. The NTI-tss device for the therapy of bruxism, temporomandibular disorders and headache – where do we stand? A qualitative systematic review of the literature. BMC Oral Health. 2008;8:22.
Turp JC, Jokstad A, Motschall E, Schindler HJ, Windecker-Getaz I, Ettlin DA. Is there a superiority of multimodal as opposed to simple therapy in patients with temporomandibular disorders? A qualitative systematic review of the literature. Clin Oral Implants Res. 2007;18(Suppl 3): 138–150.
Turp JC, Motschall E, Schindler HJ, Heydecke G. In patients with temporomandibular disorders, do particular interventions influence oral health-related quality of life? A qualitative systematic review of the literature. Clin Oral Implants Res. 2007;18(Suppl 3):127–137.
Medlicott MS, Harris SR. A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorders. Phys Ther. 2006;86:955–973.
McNeely ML, Armijo-Olivo S, Magee DJ. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86:710–725.
List T, Axelsson S, Leijon G. Pharmacologic interventions in the treatment of temporomandibular disorders, atypical facial pain, and burning mouth syndrome. A qualitative systematic review. J Orofac Pain. 2003;17:301–310.
Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:212–223.
Simmons HC, Kilpatrick SR. A survey of dentists in the United States regarding a specialty in craniofacial pain. Cranio. 2004;22:72–76.
Manfredini D, Guarda-Nardini L. Temporomandibular joint injury assessment: traumatic and iatrogenic lesions. Guidelines of the Italian Society of Legal Medicine and Dentistry. Tagete – Arch Legal Med Dent. 2008;1:1–20.
Ismail AI, Bader JD. Evidence-based dentistry in clinical practice. J Am Dent Assoc. 2004;135:78–83.
FDI. Dental ethics manual. France: FDI World Dental Federation, 2007.
Goldstein BH. Unconventional dentistry. Part III. Legal and regulatory issues. J Can Dent Assoc. 2000;66:503–506.
Rinchuse DJ, Kandasamy S. Centric relation: a historical and contemporary orthodontic perspective. J Am Dent Assoc. 2006;130:494–501.
Rinchuse DJ, McMinn J. Summary of evidence-based systematic reviews of temporomandibular disorders. Am J Orthod Dentofacial Orthop. 2006;130:715–720.
Rinchuse DJ, Kandasamy S, Sciote J. A contemporary and evidence-based view of canine protected occlusion. Am J Orthod Dentofac Orthop. 2007;132:90–102.
McNamara JA, Seligman DA, Okeson JP. Occlusion, orthodontic treatment, and temporomandibular disorders: a review. J Orofac Pain. 1995;9:73–90.
Wolfart S, Heydecke G, Luthardt RG, Marre´ B. Effects of prosthetic treatment for shortened dental arches on oral health related quality of life, self reports of pain and jaw disability: results from the pilot-phase of a randomized multicentre trial. J Oral Rehabil. 2005;32:815–822.
De Boever JA, Carlsson GE, Klineberg IJ. Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part II: tooth loss and prosthodontic treatment. J Oral Rehabil. 2000;27:647–659.
Sessle BJ. Biological adaptation and normative values. Int J Prosthodont. 2003;16(Suppl):72–73.
Klineber I, Stohler CS. Interface of occlusion. Int J Prosthodont. 2003;16(Suppl):89–90.
Stohler CS. Management of dental occlusion. In: Laskin DM, Greene CS, Hylander WL, eds. TMDs. An evidence-based approach to diagnosis and treatment. Chicago: Quintessence, 2006:403–411.
Le Bell Y, Ja¨msa¨ T, Korri S, Niemi PM, Alanen P. Effect of artificial occlusal interferences depends on previous experience of temporomandibular disorders. Acta Odontol Scand. 2002;60:219–222.
Bucci MB, Manfredini D. Is there an ideal occlusal scheme for implant-retained prosthesis? Tagete – Arch Legal Med Dent. 2009;15:768–777.
Sessle BJ. Mechanisms of oral somatosensory and motor functions and their clinical correlates. J Oral Rehabil. 2006;33:243–261.
Montagna F, Manfredini D, Nuzzolese E. Professional liability and structure of litigation in dentistry. Minerva Stomatol. 2008;57:349–357.
De Leeuw R, Boering G, van der Kuijl B, Stegenga B. Hard and soft tissue imaging of the temporomandibular joint 30 years after diagnosis of osteoarthrosis and internal derangement. J Oral Maxillofac Surg. 1996;54:1270–1280 discussion 1280–1.
Ko¨no¨nen M, Waltimo A, Nystro¨m M. Does clicking in adolescence lead to painful temporomandibular joint locking? Lancet. 1996;347:1080–1081.
Rammelsberg P, LeResche L, Dworkin S, Mancl L. Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 2003;17:9–20.
Sundqvist B. Individual prediction of treatment outcome in patients with temporomandibular disorders. A quality improvement model. Swed Dent J Suppl. 2007;186: 8–42.
Emshoff R, Rudisch A. Likelihood ratio methodology to identify predictors of treatment outcome in temporomandibular joint arthralgia patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:525–533.
Clark GT, Baba K, McCreary CP. Predicting the outcome of a physical medicine treatment for temporomandibular disorder patients. J Orofac Pain. 2009;23:221–229.
Manfredini D. Fundamentals of TMD management. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:305–318.
McNeill C. Fundamental treatment goals. In: McNeill C, ed. Science and practice of occlusion. Chicago: Quintessence Publishing, 1997:306–322.
Cooper BC, Kleinberg I. Examination of a large patient population for presence of symptoms and signs of temporomandibular disorders. Cranio. 2007;25:114–126.
Bergamini M, Pierleoni F, Gizdulich A, Bergamini C. Dental occlusion and body posture: a surface EMG study. Cranio. 2008;26:25–32.
Cooper BC, Kleinberg I. Establishment of temporomandibular physiological state with neuromuscular orthosis treatment affects reduction of TMD symptoms in 313 patients. Cranio. 2008;26:104–117.
Moses AJ. Book review: TMDs, and evidence-based approach to diagnosis and treatment. Cranio. 2007;25: 5–7.
Greene CS. The role of biotechnology in TMD diagnosis. In: Laskin DM, Greene CS, Hylander WL, eds. TMDs. An evidence-based approach to diagnosis and treatment. Chicago: Quintessence Publishing, 2006:193–202.
Lobbezoo F, Visscher C, Naeije M. Treatment of TMD: think twice!. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:483–486.
Bucci MB, Aversa M, Guarda-Nardini L, Manfredini D. Occlusion and temporomandibular disorders: a malpractice case with medical legal considerations. Minerva Stomatol, in press.
Karjalainen M, Le Bell Y, Ja¨msa¨ T, Karjalainen S. Prevention of temporomandibular disorder-related signs and symptoms in orthodontically treated adolescents. A 3-year follow-up of a prospective randomized trial. Acta Odontol Scand. 1997;55:319–324.
Kirveskari P, Jamsa T. Health risk from occlusal interferences in females. Eur J Orthod. 2009;31:490–495.
Henrikson T, Nilner M. Temporomandibular disorders, occlusion and orthodontic treatment. J Orthod. 2003;30: 129–137.
Egermark I, Magnusson T, Carlsson GE. A 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. Angle Orthod. 2003;73:109–115.
Mohlin B, Axelsson S, Paulin G, Pietila¨ T, Bondemark L, Brattstro¨m V et al. TMD in relation to malocclusion and orthodontic treatment. Angle Orthod. 2007;77:542–548.
Michelotti A, Iodice G. The role of orthodontics in temporomandibular disorders. J Oral Rehabil 2010;37:411–429.
Ellis E, Throckmorton GS. Treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg. 2005;63:115–134.
Goldberg MB. Posttraumatic temporomandibular disorders. J Orofac Pain. 1999;13:291–294.
Ohura N, Ichioka S, Sudo T, Nakagawa M, Kumaido K, Nakatsuka T. Dislocation of the bilateral mandibular condyle into the middle cranial fossa: review of the literature and clinical experience. J Oral Maxillofac Surg. 2006;64: 1165–1172.
Yucel E, Borkan U, Mollaoglu N, Erkmen E, Gunhan O. Histological evaluation of changes in the temporomandibular joint after direct and indirect trauma: an experimental study. Dental Traumatology. 2002;18:212–216.
Tanaka E, Kawai N, Van Eijden T, Watanabe M, Hanaoka K, Nishi M et al. Impulsive compression influences the viscous behavior of porcine temporomandibular joint disc. Eur J Oral Sci. 2003;111:353–358.
Toyama M, Kurita K, Koga K, Ogi N. Ankylosis of the temporomandibular joint developing shortly after multiple facial fractures. Int J Oral Maxillofac Surg. 2003;32:360–362.
Ferretti C, Bryant R, Becker P, Lawrence C. Temporomandibular joint morphology following post-traumatic ankylosis in 26 patients. Int J Oral Maxillofac Surg. 2005;34:376–381.
Cascone P, Leopardi R, Marino S, Carnemolla ME. Intracapsular fractures of mandibular condyle: diagnosis, treatment, and anatomical and pathological evaluations. J Craniofac Surg. 2003;14:184–191.
Kempers KG, Quinn PD, Silverstein K. Surgical approaches to mandibular condylar fractures: a review. J Craniomaxillofac Trauma. 1999;5:25–30.
Defabianis P. TMJ fractures in children and adolescents: treatment guidelines. J Clin Pediatr Dent. 2003;27:191–199.
McKay DC, Christensen LV. Whiplash injuries of the temporomandibular joint in motor vehicle accidents: speculations and facts. J Oral Rehabil. 1998;25:731–746.
Friedman MH, Weisberg J. The craniocervical connection: a retrospective analysis of 300 whiplash patients with cervical and temporomandibular disorders. Cranio. 2000;18:163–167.
Kronn E. The incidence of TMJ dysfunction in patients who have suffered a cervical whiplash injury following a traffic accident. J Orofac Pain. 1993;7:234–239.
Hill BA. The environment and disease: association or causation? Proceed Royal Soc Med. 1965;58:295–300.
Susser M. Judgement and causal inference: criteria in epidemiologic studies. Am J Epidemiol. 1977;105:1–5.
Nepps ME. The basics of medical malpractice: a primer on navigating the system. Chest. 2008;134:1051–1055.
Kapp B. The interface of law and medical ethics in medical intensive care. Chest. 2009;136:904–909.
Szalados BJ. Anesthesia in remote locations: medicolegal risks and strategies for minimizing liability. Int Anesthesiol Clin. 2009;47:105–131.
Zinman EJ. Ethics versus legal informed consent – a distinction with little difference. J hist Dent. 2007;55:134–138.
Steenks MH, Hugger A, De Wijer A. Painful arthrogenous temporomandibular disorders. Pathophysiology, diagnosis, management and prognosis. In:
Tu¨rp JC, Sommer C, Hugger A, eds. The puzzle of orofacial pain. Integrating research into clinical management. Pain headache, vol 15. Basel: Karger, 2007:124–152.
De Bont LGM, Dijkgraaf LC, Stegenga B. Epidemiology and natural progression of articular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:72–76.
Stohler CS. Phenomenology, epidemiology, and natural progression of the muscular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:77–81.
De Leeuw R. Internal derangements of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 2008;20: 159–168.
Speece R, Shimm D, Buchanan A. Conflicts of interest in clinical practice and research. New York: Oxford University Press, 1996.
Brunette DM. Critical thinking: understanding and evaluating dental research, 2nd edn. Chicago: Quintessence Publishing, 2007.
Suvinen TI, Hanes KR, Gerschman JA, Reade PC. Psychophysical subtypes of temporomandibular disorders. J Orofac Pain. 1997;11:200–205.
Rollman GB, Gillespie JM. The role of psychosocial factors in temporomandibular disorders. Curr Rev Pain. 2000;4: 71–81.
Dworkin SF. Psychological and psychosocial assessment. In: Laskin DM, Greene CS, Hylander WL, eds. TMDs. An evidence-based approach to diagnosis and treatment. Chicago: Quintessence Publishing, 2006:203–218.
Goulet JP, Palla S. The path to diagnosis. In: Sessle BJ, Lavigne GJ, Lund JP, Dubner R, eds. Orofacial pain From basic science to clinical management, 2nd edn. Chicago, USA: Quintessence Publishing, 2008:135–143.
Kafas P, Leeson R. Assessment of pain in temporomandibular disorders: the bio-psychosocial complexity. Int J Oral Maxillofac Surg. 2006;35:145–149.
Turner JA, Dworkin SF, Mancl L, Huggins K, Truelove E. The roles of beliefs, catastrophizing, and coping in the functioning of patients with temporomandibular disorders. Pain. 2001;92:41–51.
Reissmann DR, John MT, Wassell RW, Hinz A. Psychosocial profiles of diagnostic subgroups of temporomandibular disorder patients. Eur J Oral Sci. 2008;116:237–244.
Baad-Hansen L, Leijon G, Svensson P, List T. Comparison of clinical findings and psychosocial factors in patients with atypical odontalgia and temporomandibular disorders. J Orofac Pain. 2008;22:7–14.
Manfredini D, Marini M, Pavan C, Pavan L, Guarda-Nardini L. Psychosocial profiles of TMD patients. J Oral Rehabil. 2009;36:193–198.
Ohrbach R. Disability assessment in temporomandibular disorders and masticatory system rehabilitation. J Oral Rehabil 2010;37:452–480.
Ohrbach R, Turner JA, Sherman JJ, Mancl LA, Truelove EL, Schiffman EL et al. The Research Diagnostic Criteria for Temporomandibular Disorders. IV: evaluation of psychometric properties of the Axis II measures. J Orofac Pain. 2010;24: 48–62.
Al-Belasy FA, Dolwick MF. Arthrocentesis for the treatment of temporomandibular joint closet lock: a review article. Int J Oral Maxillofac Surg. 2007;36:773–782.