Taper 0.06 Versus Taper 0.04: The Impact on the Danger Zone
ABSTRACT
Introduction: This study aimed to evaluate the effects of root canal enlargement on the danger zone (DZ) of mandibular molars. Further details about root canal preparation and filling are accessible for you to learn on our website in Endodontics section.
Methods: Thirty mesial roots of mandibular first molars were scanned in micro-computed tomography (S1). Canals were sequentially enlarged with rotary instruments up to sizes 30/0.04 (S2) and 30/0.06 (S3). The dentin thickness was measured at 0.1-mm intervals after each preparation step (n = 2964 slices). Root level and position of the DZ were also recorded. Data were compared using analysis of variance with Bonferroni pairwise comparison, Cochran’s Q method, and Pearson’s test (a = 5%).
Results: Comparing the specimens before (S1) and after (S2 and S3) preparations showed A significant reduction in the thickness of the DZ (P < .05), as well as between S2 and S3 steps (P < .05). At S1, the DZ was mostly located in the middle third of the root, but after preparation, it shifted toward the coronal direction (P < .05). Both S2 (P = .004, r = 0.508) and S3 (P = .004, r = 0.506) preparation steps showed a positive correlation between canal length and the root level of the DZ. At S1, the DZ was positioned toward the distal and mesial in 73.4% (n = 22) and 26.6% (n = 8) of the specimens, respectively. After S3, the number of specimens with DZ positioned toward the mesial aspect of the root significantly reduced to 3.3% (n = 1), whereas none of the specimens with DZ positioned toward the distal changed its position after root canal enlargements (P > .05).
Conclusion: Overall, the enlargement of mesial canals of mandibular first molars with final instruments sizes 30/0.04 and 30/0.06 affected the thickness, root level, and position of the DZ.
INTRODUCTION
Root canal enlargement has long been a topic of discussion in the field of endodontics, but there is still a lack of formal evidence regarding the optimal extent of canal enlargement. The introduction of nickel-titanium (NiTi) instruments in the early 1990s led to the mechanization of canal preparation, with manufacturers primarily offering an instrumentation sequence that produced a 0.06 taper preparation(1,2).
This proposal was based on the known advantages of a tapered shape(3,4), as well as on the description reported in the classical article of Schilder(5), which recommended a uniform and continuous taper progressively smaller in diameter from coronal to apex for a well-shaped canal. In addition, this enlargement size adequately encompasses the main canal anatomy when viewed through radiographs.
Despite the initial excitement, the use of NiTi systems became marketed based on their ability to "machine preparations with specific tapers,”(6) and as a result, the endodontic community largely embraced the preparation of root canals with large-tapered instruments. The emphasis on large-tapered instruments for root canal preparation was primarily motivated by the marketability of NiTi systems and their capacity to generate precise tapers, rather than scientific evidence. While this approach was initially adopted by the endodontic community, there is still a lack of conclusive research on the most suitable size and shape of root canal preparations.
Although the ideal enlargement of the root canal space should be based on preoperative anatomic dimensions(7-9), there is a growing emphasis on a technical strategy that achieves efficient shaping, cleaning, and disinfection while minimizing unnecessary dentin removal to prevent catastrophic root fracture(10). This approach is especially important in the context of the danger zone (DZ), given the potential risk of strip perforation associated with larger preparation sizes, which raises concerns about the suitability of using taper 0.06 instruments as master apical files.
Conventionally, the DZ is defined as the distal region between the main canal space and the root bifurcation, which is characterized by the thinnest dentin that is more susceptible to the development of strip perforations11. Although the DZ concept was introduced more than 4 decades ago11, its impact on the root morphology as a result of canal shaping remains inconsistent, sparse, and at times, controversial. This is mainly due to the lack of systematic exploration using nondestructive and reliable longitudinal methods. Therefore, the primary objectives of this investigation arose from the current lack of knowledge regarding the optimal canal enlargement size and the potential role of the DZ as a prognostic marker in strip perforations(12,13), and sought to compare the effects of continuous tapered NiTi rotary instruments (sizes 30/0.04 and 30/0.06) for final enlargement of mesial canals of mandibular first molars on the DZ (thickness, root level, and position), as well as the influence of root length on the DZ level following preparation. Nondestructive micro-computed tomography (micro-CT) technology was used as the analytical tool. The null hypothesis that was tested posited that final canal enlargement with instruments 30/0.04 and 30/0.06 would have no significant impact on the thickness, root level, and position of the DZ.
MATERIAL AND METHODS
Sample Size Calculation
Sample size was estimated based on an effect size of 0.35 calculated from the results of a previous study in which authors found a significant impact on the remaining dentin thickness at the DZ after the enlargement of root canals with NiTi instruments using computed tomography(14). Following the F family and analysis of variance repeated measures within factors model, with an alpha-type error of 0.05, power beta of 0.95, correlation among repeated measures of 0.7, and nonsphericity correction (Epsilon) of 0.5, the minimum sample size for the present study was calculated as 24 specimens (G*Power 3.1 for Macintosh; Heinrich Heine, Universitat Dusseldorf, Dusseldorf, Germany).
Sample Selection and Imaging
After the approval of this research project by the local Ethics Research Committee of Fluminense Federal University (Protocol 06701319.8.0000.0053), 120 2-rootedmandibular first molars, extracted for reasonsnot related to this study, were scanned in amicro-CT device (SkyScan 1173; Bruker-microCT, Kontich, Belgium) set at 14.25 mm (pixel size), 70 kV, 114 mA, 180 of rotation with steps of 0.5, frame average of 4, using a 1-mm-thick aluminum filter. The acquired images were reconstructed (NRecon v. 1.7.1.6; Bruker-microCT) with similar parameters for beam hardening (30%–40%), ring artifact correction (5), and contrast limits (0–0.05). Then, mesial roots were evaluated regarding canal configuration and length using DataViewer v.1.5.6 software (Bruker-microCT). The determination of root length was conducted by measuring the vertical extent from a horizontal plane that intersected the anatomic apex at a right angle along the long axis, to a second horizontal plane that crossed the lowest point of the cemento-enamel junction on the buccal surface of the crown, parallel to the first plane. Then, 30 moderately curved mesial roots (10–20) measuring 10 to 12 mm in length and presenting 2 independent canals in the coronal and middle thirds were selected. Exclusion criteria included teeth with deep caries or restoration, severe abrasion, previous root canal treatment, incomplete root formation, fracture, resorption, or root fusion.
Root Canal Preparation
After access cavity preparation, apical patency was confirmed with a size 10 K-file (Dentsply Sirona Endodontics, Ballaigues, Switzerland) and glide path was performed with a size 15 K-file (Dentsply Sirona Endodontics) up to the working length (WL), established 1 mm from the apical foramen. The apical third of each root was covered with hot glue and embedded into a polyvinyl siloxane (Speedex; Coltene, Cuyahoga Falls, OH) to simulate a closed-end system and provide mechanical stability during the experimental procedures. Then, the mesiobuccal and mesiolingual canals were prepared using an in-and-out motion with Hero 642 rotary instruments (MicroMega, Besaçon, France) adapted to the VDW Silver motor (VDW, Munich, Germany) set at 350 rpm and 2 N cm. Initially, canals were enlarged up to the WL with the sequential use of instruments sizes 25/0.02, 25/0.04, and 30/0.04. After performing a new scan of the samples, root canals were additionally enlarged to the WL using instruments sizes 25/0.06 and 30/0.06, and all teeth were imaged again. One instrument was used per root and then discarded. Patency was checked with a size 10 K-file (Dentsply Sirona Endodontics) throughout the preparation procedures.
Irrigation was carried out using a 31-G NaviTip double-side port needle (Ultradent Inc, South Jordan, UT) positioned 1 mm short of the WL. Each canal was irrigated with 2 mL of 2.5% NaOCl after access preparation and glide path procedures, 2 mL of 2.5% NaOCl after each instrument, and 1 mL of 2.5% NaOCl after recapitulation with the patency file, followed by a final flush with 3 mL of 17% EDTA and 2 mL of bi-distilled water. A single and experienced endodontist, who was blinded to the internal morphology of the specimens, performed all preparation procedures.
Imaging Analyses
Three high-resolution scans were accomplished per tooth: before preparation (S1) and after preparation with instruments sizes 30/0.04 (S2) and 30/0.06 (S3). The acquired projections were reconstructed and coregistered using the affine algorithm implemented on the 3-dimensional (3D) Slicer v.4.11 software.
Then, transaxial cross-sections related to the trunk of dentin from the pulp chamber floor to the root furcation were discarded and the mesial canals were divided into thirds from this point to the major foramen. Considering the anatomic complexities usually observed at the apical third of the mesial root, the volume of interest included the coronal and middle thirds (Fig. 1A). Based on 3D models of root surfaces and canals, the central axis was obtained for each root canal (V-works 4.0 software; Cybermed Inc, Seoul, Republic of Korea) and the dentin thickness (in mm) was measured automatically on re-sliced planes made perpendicular to the central axis of each canal at 0.1-mm intervals using Kappa 2 software(12) (Fig. 1B). The level of the minimal dentin thickness (DZ) in relation to the furcation was recorded, and its position (mesial or distal) identified on the cutting plane (Fig. 1C–E). These variables were obtained by screening 2964 cross-sectional slices from datasets acquired at S1, S2, and S3 steps and plotted for statistical comparison. In addition, a 3D mapping of the dentin thickness throughout the root was created (CTAn v.1.14.4 software; Bruker-microCT) and qualitatively evaluated (CTVox v.3.3.0 software; Bruker-microCT). All analyses were performed by an experienced researcher in micro-CT images blinded to the experimental procedures.
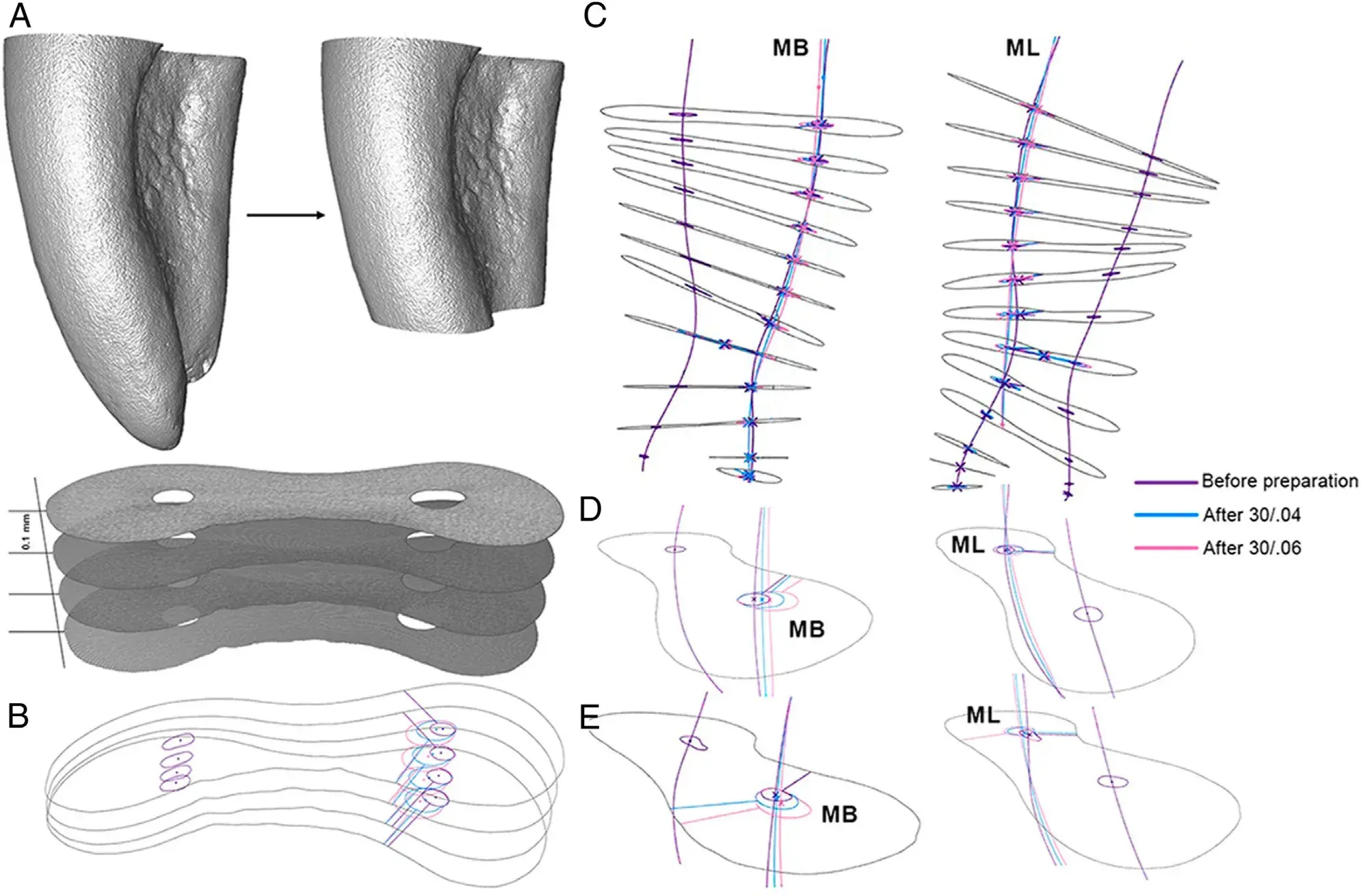 FIGURE 1 – Imaging analyses. (A ) After dividing the mesial roots into thirds, the apical part was discarded because of anatomic complexities that could compromise the analyses. So, volume of interest included coronal and middle thirds. (B ) Re-sliced planes made perpendicular to the central axis of each canal were obtained at 0.1-mm intervals. (C ) Minimal dentin thicknesses were automatically measured and recorded its position (mesial or distal) on each cutting plane by using Kappa 2 software. (C ) Automatic computational routine for digital image analyses and processing based on micro-computed tomography datasets obtained to evaluate the danger and safety zones in mesial roots of mandibular molars. This robust methodology allows calculation of the minimal dentin thicknesses using precise root sectionsobtained perpendicularly to the long axis of both (D ) mesiobuccal (MB) and (E ) mesiolingual (ML) canals.
FIGURE 1 – Imaging analyses. (A ) After dividing the mesial roots into thirds, the apical part was discarded because of anatomic complexities that could compromise the analyses. So, volume of interest included coronal and middle thirds. (B ) Re-sliced planes made perpendicular to the central axis of each canal were obtained at 0.1-mm intervals. (C ) Minimal dentin thicknesses were automatically measured and recorded its position (mesial or distal) on each cutting plane by using Kappa 2 software. (C ) Automatic computational routine for digital image analyses and processing based on micro-computed tomography datasets obtained to evaluate the danger and safety zones in mesial roots of mandibular molars. This robust methodology allows calculation of the minimal dentin thicknesses using precise root sectionsobtained perpendicularly to the long axis of both (D ) mesiobuccal (MB) and (E ) mesiolingual (ML) canals.
There are additional information about endodontic treatment in complex cases that you can obtain in our course "Endodontics 3.0".
Statistical Analyses
Results were a priori evaluated with the Shapiro-Wilk test, which confirmed the normal distribution of the data (P > .05). Then, parametric data (minimal dentin thickness and root level) were compared among different preparation steps (S1, S2, and S3) using the repeated measures analysis of variance general linear model test with Bonferroni pairwise comparison. Mauch’s sphericity test disclosed an unequal variance of the differences between the pairs of within-subject (lack of sphericity) for both parameters (P = .000), but with acceptable Epsilon values of 0.633 (minimal dentin thickness) and 0.704 (root level) (Greenhouse-Geisser correction).
Modifications on the position (mesial or distal) of the original DZ after canal preparation were compared using the Cochran’s Q method. Differences at the root level of the DZ after S2 and S3 steps were correlated with the canal length to test the hypothesis of whether longer canals would result in greater shift of the DZ toward the coronal direction after canal enlargement using Pearson’s correlation test.
All analyses were performed using the SPSS v.21.0 software (SPSS Inc, Chicago, IL) with a significance level set at 5%.
RESULTS
Table 1 depicts the DZ parameters regarding its thickness, root level, and position after S1 (before preparation), S2 (after instrument size 30/0.04), and S3 (after instrument size 30/0.06) preparation steps. The thickness of the DZ significantly reduced not only when comparing the specimens before (S1) and after (S2 and S3) preparations (P = .000, Greenhouse-Geisser), but also between S2 and S3 (P = .000, Bonferroni) (Table 1, Fig. 2).
At S1, the DZ was located mostly at the middle third (27 of 30 canals). After preparation, the DZ changed its original position to more coronal, being statistically significant in S2 (P = .000, Bonferroni) and S3 (P = .000, Bonferroni), but not when comparing them (P = 1.000, Bonferroni) (Table 1, Fig. 3). A positive correlation was verified between the canal length and the level of DZ, meaning that as longer the canal, more coronal DZ was located in both S2 (P = .004, r = 0.508, r 2 = 0.258) and S3 (P = .004, r = 0.506, r2 = 0.256) steps (Supplemental Fig. S1).
Before preparation, 26.6% of the specimens (n = 8) had the DZ positioned toward the mesial aspect of the root, significantly reducing to 3.3% (n 5 1) at S3 (P = .005, Cochran’s Q test). On the other hand, all specimens with DZ located toward distal in S1 (n = 22) did not change its position after the final enlargement of root canals with instrument sizes 30/0.04 (S2) or 30/0.06 (S3) (P = 1.000, Cochran’s Q test).
TABLE 1 - Mean, Standard Deviation, and Interval Range of Minimal Dentine Thickness (in mm) and Root Level of the Danger Zone (DZ), as Well as the Number (n) and Percentage Frequency (%) of Slices in Which the DZ Was Positioned to the Mesial or Distal Aspects of the Root Before and After Each Preparation Step.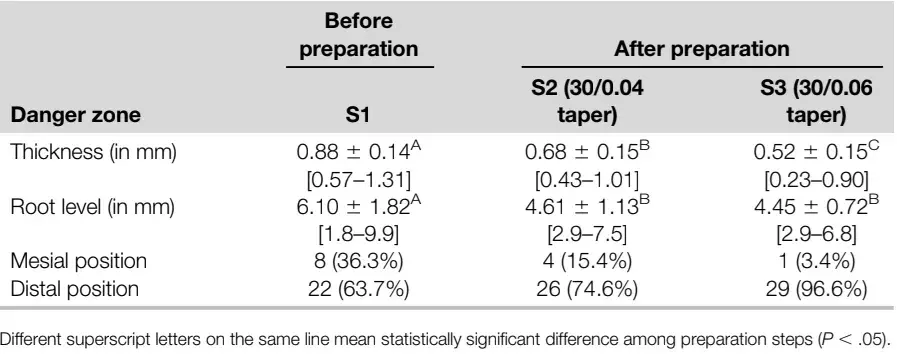
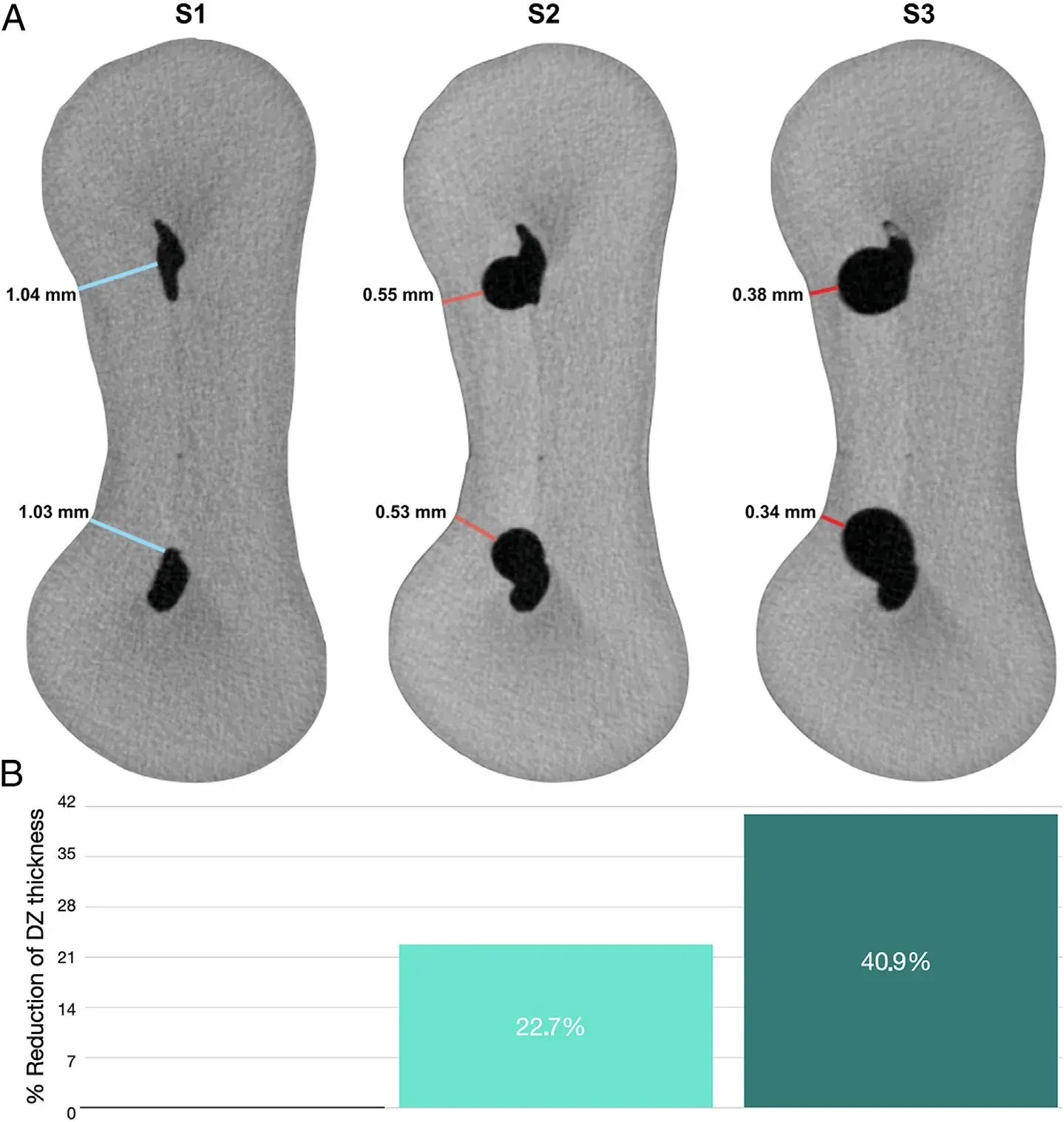 FIGURE 2 – (A ) Representative cross-section of a mandibular molar mesial root before (S1) and after preparation with instruments sizes 30/0.04 (S2) and 30/0.06 (S3) demonstrating the significant reduction on dentin thickness toward the distal aspect of the root after preparation procedures. (B ) Percentage reduction of the danger zone (DZ) thickness after S2 (22.7%) and S3 (40.9%) steps.
FIGURE 2 – (A ) Representative cross-section of a mandibular molar mesial root before (S1) and after preparation with instruments sizes 30/0.04 (S2) and 30/0.06 (S3) demonstrating the significant reduction on dentin thickness toward the distal aspect of the root after preparation procedures. (B ) Percentage reduction of the danger zone (DZ) thickness after S2 (22.7%) and S3 (40.9%) steps.
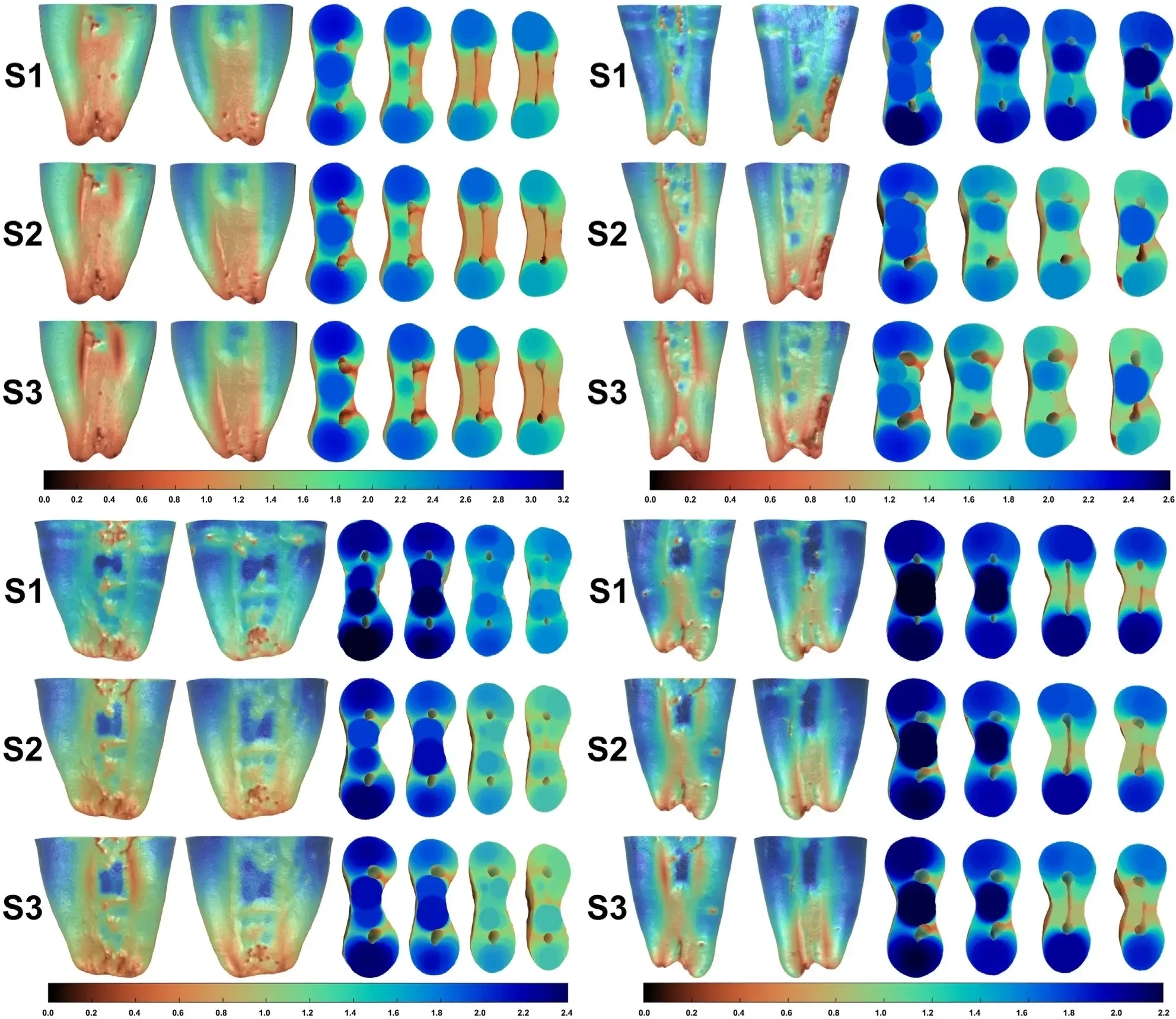 FIGURE 3 – Representative 3-dimensional colored models of 4 mesial roots of mandibular molars at 3 different preparation steps: before preparation (S1), and after preparation with instruments sizes 30/0.04 (S2) and 30/0.06 (S3).
FIGURE 3 – Representative 3-dimensional colored models of 4 mesial roots of mandibular molars at 3 different preparation steps: before preparation (S1), and after preparation with instruments sizes 30/0.04 (S2) and 30/0.06 (S3).
The models showcase the distal and mesial aspects of the roots on the left and 4 cross-sections of each root obtained from the coronal and middle thirds on the right. The colors in each model indicate the depth of the dentin, with thick structures shown in blue and green, and thin areas in red. Notably, there is a significant reduction in dentin thickness in the representative cross-sections of coronal and middle thirds related to the mesial canals following the preparation procedures.
DISCUSSION
The mesial root of mandibular molars has been extensively studied regarding the morphology of the DZ. Although previous studies have primarily focused on the coronal third(13,15-19), where strip perforation is commonly reported at the furcation level(20), the present study examined mean dentin thickness at the coronal and middle levels of both mesiobuccal and mesiolingual canals. Mean thickness values in the range of 0.67 to 1.25 mm have been reported in previous studies(12,15-19,21-24), which is consistent with the mean preoperative thickness (0.88 mm) observed in this study (Table 1). Notably, the mean preoperative thickness in the present study was lower than that reported in most studies, which typically report mean values higher than 1 mm(16-19,22).
The use of nondestructive micro-CT technology and an automatic computational routine for digital image analyses and processing may have contributed to the observed differences, as previous studies have relied on destructive methods and direct observation of only a few root sections per tooth. These findings highlight the importance of considering the potential impact of methodological factors on DZ measurements and further emphasize the need for continued research in this area.
A recent study by De-Deus and colleagues(12,25) reexamined the location of the DZ in nonprepared mesial roots of mandibular molars, finding that it was predominantly located in the middle third (4 to 7 mm below the furcation), which is consistent with the findings of the present study (Table 1). In addition, the study revealed that 36.3% of evaluated specimens before preparation had the DZ located toward the mesial aspect of the root (Table 1), which is in line with previous reports using micro-CT technology (33%26 and 40%25). Despite the expected decrease in dentin thickness with successive enlargement of root canals using instrument sizes 30/0.04 (S2) and 30/0.06 (S3) (Table 1), a notable finding was that the position of the DZ shifted from the middle to the coronal third (Table 1, Fig. 3), concurrent with canal enlargement. Furthermore, almost all DZs that were located at the mesial aspect of the root moved toward the distal direction after preparation, whereas no changes were observed in the DZ located toward the distal in S1 (Table 1). These results provide important insights into the effect of root canal preparation on the location of the DZ in mandibular molars, which could have implications for clinical practice. As coronal flaring was not performed in this study, it is likely that the dentinal projection that partially covers the mesiobuccal and mesiolingual canal orifices caused the rotary instruments to deflect toward the distal direction at the coronal third, which may explain these results. In addition, this effect may have been more significant in this study because of the rotary system used to prepare the root canals.
Notwithstanding Hero 642 instruments present noncutting tips, alternating cutting edges, and a triangular cross-section, intended to help the instrument navigate the canal smoothly while reducing the risk of instrument separation or canal transportation, they have progressive (not regressive) tapers, which means that the diameter of the file increases gradually from the tip to the handle. The current findings, which demonstrate that the DZ shifted toward the distal aspect of the coronal third of the mesial root during preparation, provide insight into the numerous reports of strip perforation in this area(20), although no perforation was observed in this study.
Thus, these findings support the use of less tapered or regressive tapered instruments for the preparation of mesial canals of mandibular molars, particularly in long roots. This statement is in agreement with the anatomic study of Dwivedi et al.(27), who reported that long mesial roots are more prone to strip perforation because they are thinner and more concave at their distal aspect than in short molars.
The mechanical preparation of root canals is an invasive process that may result in varying degrees of dentin removal, depending on the instrumentation techniques and systems used. This can affect the biomechanical response of teeth and weaken their ability to withstand occlusal loads over the long term. Although there is currently limited scientific evidence on this topic(10,28), logical reasoning suggests that reducing the mass of dentin may compromise the strength of the tooth to resist occlusal loads in the long term.
Thus, there is a need to strike a balance between removing enough tissue to adequately clean the root canal while preserving enough to maintain the tooth’s strength. Previous studies have questioned the necessity of using instruments with a 0.06 taper, suggesting that smaller tapered instruments may be just as effective at cleaning the root canal(29-31); however, these studies relied on scanning electron microscopy, which is not a reliable or reproducible analytical method for this purpose(32) . Recently, there have been several studies investigating the impact of different NiTi instruments on the dentin removal and the untouched canal walls. Using micro-CT imaging, Lima et al.(33) demonstrated that small-tapered instruments (0.03) resulted in a higher percentage of untouched canal walls, but the same percentage of removed dentin compared with large-tapered systems (0.04v and 0.08v).
Similarly, Silva et al.34 found no differences in the unprepared areas or reduction in dentin thickness between TruNatomy (size 26/0.04v) and ProTaper Gold (size 25/0.08v) systems in the enlargement of mesial root canals of mandibular molars. Augusto et al.(35) evaluated the percentage of dentin removed from mesial root canals enlarged by instruments with different tapers (0.03 or 0.05) and tip diameters (25 or 40) and found no significant differences between instruments of different tapers.
Despite these findings, the methodological variations and baseline anatomic landmarks among the mentioned studies might justify the observed differences and thus, further studies are still necessary to better understand the impact of the design and dimensions of NiTi instruments on the DZ. In addition, similar studies are required to assess the DZ after instrumentation of other types of teeth, including those presenting 2 canals in the same root, such as mandibular incisors, mandibular premolars, and the mesiobuccal root of maxillary molars.
In the current investigation, the impact of using final instrument sizes 30/0.04 and 30/0.06 on the thickness, location, and level of the DZ during mesial canal enlargement of mandibular first molars was examined, leading to the rejection of the null hypothesis. As Abou-Rass et al.(11) have highlighted the significance of the DZ during canal shaping, several studies have been conducted to assess the DZ anatomy and the effect of various preparation techniques and instruments on its thickness. However, most of these studies used destructive methods(13,15-17,19), which limited the experiment’s credibility, as only a few slices were analyzed per root. Furthermore, invasive techniques are incapable of obtaining accurate root sections perpendicular to the canal’s long axis, as in the present study (Supplemental Video S1). By using high-resolution micro-CT technology and a dedicated software, these limitations can be overcome.
Lee et al.(26) were the pioneers in using an automated and robust computational algorithm for digital image analysis and processing based on micro-CT datasets acquired from actual teeth to perform a thorough anatomic investigation of DZs and safety zones in mesial roots of mandibular molars, which was followed by De-Deus et al.(12,25) This technique enables the acquisition of a complete 3D map of dentin thickness throughout the entire root and analysis of hundreds of cross-sections per root, resulting in a less time-consuming and labor-intensive experiment. However, the present study is limited by the use of stored teeth with unknown age, which may have influenced the results because of the presence of physiological and pathological hard tissue deposits within the root canal space that may have increased overall dentin thickness and hardness. Future investigations should use the same analytical approach as our study to compare the effect of different preparation systems on the DZ. In addition, it is important to use teeth from patients with documented age to account for the potential influence of physiological and pathological alterations in dentin deposition within the root canal space throughout the individual’s life.
CONCLUSIONS
Based on the findings of this study, it was possible to conclude that the mechanical preparation of mesial canals in mandibular first molars using final instrument sizes of 30/0.04 and 30/0.06 resulted in a significant reduction in dentin thickness, relocation of the original level of the DZ from the middle to the coronal third, and a shift of most of the DZ from the mesial aspect of the root to the distal direction.
If you enjoyed reading this article and would like to explore the nuances of endodontic treatment further, we encourage you to enroll our course "Evidence-based endodontics: complex histo-analysis and treatment protocols".
List of authors:
Gustavo De-Deus, Evaldo A. Rodrigues, Jong-Ki Lee, J. Kim, Emmanuel J. N. L. Silva, Felipe G. Belladonna, Marco Simoes-Carvalho, Erick M. Souza, Marco A. Versiani
References
Hulsmann M, Peters OA, Dummer PMH. Mechanical preparation of root canals: shaping goals, techniques and means. Endod Topics 2005;10:30–76.
Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod 2004;30:559–67.
Boutsioukis C, Gogos C, Verhaagen B, et al. The effect of root canal taper on the irrigant flow: evaluation using an unsteady Computational Fluid Dynamics model. Int Endod J 2010;43:909–16.
De-Deus G, Marins J, Silva EJ, et al. Accumulated hard tissue debris produced during reciprocating and rotary nickel-titanium canal preparation. J Endod 2015;41:676–81.
Schilder H. Cleaning and shaping the root canal. Dent Clin North Am 1974;18:269–96.
McSpadden JT. Mastering Endodontic Instrumentation. Ramsey. Arbor Books, Inc; 2007.
Fornari VJ, Silva-Sousa YT, Vanni JR, et al. Histological evaluation of the effectiveness of increased apical enlargement for cleaning the apical third of curved canals. Int Endod J 2010;43:988–94.
Saini HR, Tewari S, Sangwan P, et al. Effect of different apical preparation sizes on outcome of primary endodontic treatment: a randomized controlled trial. J Endod 2012;38:1309–15.
Tan BT, Messer HH. The quality of apical canal preparation using hand and rotary instruments with specific criteria for enlargement based on initial apical file size. J Endod 2002;28:658–64.
Silva EJNL, De-Deus G, Souza EM, et al. Present status and future directions–Minimal endodontic access cavities. Int Endod J 2022;55(Suppl 3):531–87.
Abou-Rass M, Frank AL, Glick DH. The anticurvature filing method to prepare the curved root canal. J Am Dent Assoc 1980;101:792–4.
De-Deus G, Rodrigues EA, Lee JK, et al. Root groove depth and inter-orifice canal distance as anatomical predictive factors for danger zone in the mesial root of mandibular first molars. Clin Oral Investig 2021;25:3641–9.
Sauaia TS, Gomes BP, Pinheiro ET, et al. Thickness of dentine in mesial roots of mandibular molars with different lengths. Int Endod J 2010;43:555–9.
Olivier JG, Garcia-Font M, Gonzalez-Sanchez JA, et al. Danger zone analysis using cone beam computed tomography after apical enlargement with K3 and K3XF in a manikin model. J Clin Exp Dent 2016;8:e361–7.
Garcia Filho PF, Letra A, Menezes R, Carmo AM. Danger zone in mandibular molars before instrumentation: an in vitro study. J Appl Oral Sci 2003;11:324–6.
Kessler JR, Peters DD, Lorton L. Comparison of the relative risk of molar root perforations using various endodontic instrumentation techniques. J Endod 1983;9:439–47.
Tabrizizadeh M, Reuben J, Khalesi M, et al. Evaluation of radicular dentin thickness of danger zone in mandibular first molars. J Dent (Tehran) 2010;7:196–9.
Akhlaghi NM, Bajgiran LM, Naghdi A, et al. The minimum residual root thickness after using ProTaper, RaCe and Gates-Glidden drills: a cone beam computerized tomography study. Eur J Dent 2015;9:228–33.
Berutti E, Fedon G. Thickness of cementum/dentin in mesial roots of mandibular first molars. J Endod 1992;18:545–8.
Tsesis I, Rosenberg E, Faivishevsky V, et al. Prevalence and associated periodontal status of teeth with root perforation: a retrospective study of 2,002 patients’ medical records. J Endod 2010;36:797–800.
Kelesx A, Keskin C, Alqawasmi R, Versiani MA. Evaluation of dentine thickness of middle mesial canals of mandibular molars prepared with rotary instruments: a micro-CT study. Int Endod J 2020;53:519–28.
Lim SS, Stock CJ. The risk of perforation in the curved canal: anticurvature filing compared with the stepback technique. Int Endod J 1987;20:33–9.
Montgomery S. Root canal wall thickness of mandibular molars after biomechanical preparation. J Endod 1985;11:257–63.
Harris SP, Bowles WR, Fok A, McClanahan SB. An anatomic investigation of the mandibular first molar using micro-computed tomography. J Endod 2013;39:1374–8.
De-Deus G, Rodrigues EA, Belladonna FG, et al. Anatomical danger zone reconsidered: a micro-CT study on dentine thickness in mandibular molars. Int Endod J 2019;52:1501–7.
Lee JK, Yoo YJ, Perinpanayagam H, et al. Three-dimensional modelling and concurrent measurements of root anatomy in mandibular first molar mesial roots using micro-computed tomography. Int Endod J 2015;48:380–9.
Dwivedi S, Dwivedi CD, Mittal N. Correlation of root dentin thickness and length of roots in mesial roots of mandibular molars. J Endod 2014;40:1435–8.
Silva EJNL, Pinto KP, Ferreira CM, et al. Current status on minimal access cavity preparations: a critical analysis and a proposal for a universal nomenclature. Int Endod J 2020;53:1618–35.
Plotino G, Ozyurek T, Grande NM, Gundogar M. Influence of size and taper of basic root canal preparation on root canal cleanliness: a scanning electron microscopy study. Int Endod J 2019;52:343–51.
van der Sluis LW, Wu MK, Wesselink PR. The efficacy of ultrasonic irrigation to remove artificially placed dentine debris from human root canals prepared using instruments of varying taper. Int Endod J 2005;38:764–8.
Paraskevopoulou MT, Khabbaz MG. Influence of taper of root canal shape on the intracanal bacterial reduction. Open Dent J 2016;10:568–74.
De-Deus G, Reis C, Paciornik S. Critical appraisal of published smear layer-removal studies: methodological issues. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:531–43.
Lima CO, Barbosa AFA, Ferreira CM, et al. The impact of minimally invasive root canal preparation strategies on the shaping ability of mandibular molars. Int Endod J 2020;53:1680–8.
Silva EJNL, Lima CO, Barbosa AFA, et al. The impact of TruNatomy and ProTaper gold instruments on the preservation of the periradicular dentin and on the enlargement of the apical canal of mandibular molars. J Endod 2022;48:650–8.
Augusto CM, Barbosa AFA, Guimaraes CC, et al. A laboratory study of the impact of ultraconservative access cavities and minimal root canal tapers on the ability to shape canals in extracted mandibular molars and their fracture resistance. Int Endod J 2020;53:1516–29.

