Resolution of apical periodontitis-induced mental nerve paresthesia through non-surgical endodontic retreatment: a case report
Abstract
Introduction: Paresthesia is a potential consequence of unsuccessful root canal treatment. Persistent infection resulting in apical periodontitis may enlarge sufficiently to involve the mental neurovascular bundle. There are additional details about complex cases treatment that you can obtain in our course "Saving hopeless teeth: surgical and conservative protocols".
Methods: The case presented in this report was referred for endodontic evaluation with a chief complaint of discomfort on mastication and persistent numbness of the lower left lip. Clinical and radiographic evaluation revealed incomplete primary endodontic treatment of the left mandibular second premolar with complex internal anatomy. The untreated root canal system resulted in the progression of apical periodontitis involving the left mental neurovascular bundle as confirmed by CBCT imaging.
Results: Non-surgical root canal retreatment was performed over two visits. At the 3-year follow-up visit, the paresthesia had resolved with return of normal sensation.
Conclusion: Non-surgical endodontic retreatment may be sufficient to allow healing of large periapical lesions and resolve complications including paresthesia without the need for surgical intervention.
Introduction
The presence of bacteria within the root canal system, organized into intra-radicular biofilms, is known to cause apical periodontitis(1). In approximately 80% of failed primary endodontic treatments, bacterial biofilms can be found in the apical third of the root canal system. Successful endodontic treatment aims to resolve apical periodontitis by removing intraradicular biofilms by means of thorough chemo-mechanical preparation and obturation of the entire root canal system(2). Bacteria surviving canal disinfection procedures may result in the persistence of apical periodontitis and possible progression of these lesions(1). Whilst the majority of apical periodontitis lesions are asymptomatic(2), some may progress to involve nearby anatomical structures, including the maxillary sinus or mental neuro-vascular bundle.
This may cause complications in the form of either sinusitis or neuro-sensory alterations or, in other instances, the symptoms of apical periodontitis may exacerbate, resulting in clinical picture of an acute apical abscess. In many clinical situations, apical periodontitis and its associated complications, including neuro-sensory impairment, can be successfully treated through surgical or non-surgical endodontic treatment(1). The following report documents a case of paresthesia in the area innervated by the mental nerve, which occurred secondary to persistent apical periodontitis in a previously treated left mandibular second premolar. The case was successfully managed by means of non-surgical endodontic retreatment without the need for surgical intervention.
Case Report
This report was granted ethical approval from the Research Ethics Committee of the Faculty of Health Sciences, University of XX (Protocol number: 20/2023).
A 59-year-old man was referred to the Division of Endodontics, University of XX, in May 2018 with a complaint of tenderness to mastication on the left mandibular premolar region and paresthesia of the lower left lip of approximately two-month’s duration. The medical history revealed well-controlled hypertension.
Clinical Examination:
Upon clinical examination, the left mandibular second premolar displayed a large amalgam restoration with evidence of a previous endodontic access cavity sealed with composite resin. The examined area demonstrated a normal soft tissue appearance as well as normal periodontal probing around the tooth. The tooth showed mild tenderness to vertical percussion and no tenderness to lateral percussion or palpation.
Clinical evaluation of the neural injury:
The patient’s self-evaluation was recorded. The patient reported reduced/altered sensation in the area of the left lip and a history of root canal treatment performed many years previously. No interferences with daily activities, such as eating or speaking were noted. Further neurosensory evaluation using standardized tests as recommended by Robinson et al. (3) were performed and included the following:
Mapping the injury area: the skin of the lower left lip and chin in the area supplied by the left mental nerve demonstrated no response to sensory testing. The neuropathic area was mapped and recorded using a ball-point pen on the patient’s face (Fig. 1).
Function scoring: the patient was asked to assess his overall level of sensory function on the affected side, as compared to the contralateral (normal) side, using a scale ranging from 0 to 10 [0 = no perception of touch and 10 = normal perception]. The patient reported 0 on the left side in relation to the lip and chin area.
Light touch test: the corner of a paper was moved over the injured area, and repeated five times. The patient reported lack of light touch perception.
Sharp/blunt discrimination test: the patient reported inability to differentiate between the sharp pricks and the blunt pressure made by both ends of a dental explorer.
Two-point discrimination test: the patient was unable to discriminate the between two pressure points (open-beak tweezer) and a single pressure point (closed-beak tweezer).
Radiographic examination:
Digital intra-oral radiography revealed incomplete root canal treatment of the left mandibular second premolar, with evidence of missed canal anatomy. A well-defined radiolucency surrounding the apex of the tooth was also observed (Fig. 2A). The patient was referred for a small field-of-view cone-beam computed tomography (CBCT) scan, with a resolution of 200 µm (Planmeca Promax 3D Max, Planmeca OY, Helsingfors, Finland). The pre-operative CBCT scan assisted in the mapping of the complex canal anatomy, confirmed the extent of the periapical lesion and possible communication of the pathosis with the mental foramen (Figs. 3A, 3B and 3C).
Clinical procedures:
Treatment options offered to the patient included either non-surgical endodontic retreatment (with or without periapical surgery following a period of assessment), or extraction with replacement of the missing tooth. Being motivated to retain the tooth, the patient provided informed consent and non-surgical endodontic retreatment was initiated.
Following local anaesthesia (Xylotox E80, Adcock Ingram, Johannesburg, South Africa), the tooth was re-accessed under dental dam isolation. Magnification by means of a dental operating microscope (Global Surgical Corporation, St. Louis, MO, USA) was used for all clinical procedures. The majority of existing gutta percha (GP) and sealer were removed using a combination of Gates-glidden #2 and #3, rotary retreatment files (ProTaper D files, DentsplyMaillefer, Ballaigues, Switzerland) and heat pluggers (VDW Beefill, VDW GmbH, Munich, Germany). Patency across the apical foramen was established and working length confirmed using an electronic apex locator (ProPex Pixi, DentsplyMaillefer, Ballaigues, Switzerland) and confirmed radiographically (Fig. 2B).
Canal shaping was performed using a reciprocating instrument (WaveOne Gold primary, DentsplyMaillefer, Ballaigues, Switzerland), and irrigation performed using 3.5% sodium hypochlorite (Jik, Reckitt Benckiser, South Africa). After drying with sterile paper points, a medicated paste (Ledermix, Lederle Pharmaceuticals, Wolfratshausen, Germany) was placed into the canals and the access cavity temporised using glass-ionomer cement (Riva Self Cure, SDI ltd., Australia).
Two months after the initial visit, the patient reported that the paresthesia in the area remained, but no further discomfort to mastication was experienced. In light of this improvement, the decision was made to complete the root canal treatment. The tooth was reaccessed under dental dam isolation and the intra-canal medication removed. The final rinse protocol included 3.5% sodium hypochlorite and 17% ethylenediaminetetraacetic acid (Topclear EDTA, Dental Discounts, Johannesburg, South Africa), followed by a final rinse of sterile saline and 2% chlorhexidine.
The canals were dried using sterile paper points and obturated using a bioceramic sealer (TotalFill BC sealer, FKG Dentaire, Switzerland) and single matching cones in the apical half (Fig. 2C). The remainder of the canal system in the coronal segment was backfilled using warm GP (VDW BeeFill, VDW GmbH, Munich, Germany). The access cavity was restored using a thin layer of resin-modified glassionomer (Vitrebond, 3M ESPE, St. Paul, MN, USA) applied to cover the gutta percha as an intraorifice barrier (for the purpose of providing additional coronal seal). This was followed by etching, application of dentin adhesive (Single Bond Universal, 3M ESPE, St. Paul, MN, USA) and composite resin (Filtek XTE, 3M ESPE, St. Paul, MN, USA) as a final restoration.
Three-year recall:
Despite scheduling follow-up recalls at 3-month intervals after treatment for 1 year (then yearly), the patient could not attend as scheduled due to the Covid-19 pandemic. Three years following non-surgical retreatment in June 2021, the patient presented for follow-up reporting no symptoms. At this stage, the paresthesia had subsided completely and normal sensation had returned to the skin innervated by the left mental nerve. Restoration of neuro-sensory function in the area was confirmed by the same tests performed at the time of case evaluation(3). Periapical radiography demonstrated good healing of the periapical periodontitis with new bone formation (Fig. 2D). A follow-up CBCT scan (with the same acquisition parameters, using the same machine) confirmed radiographic healing and the reestablishment of bone in the apical area surrounding the tooth, with adequate hard tissue formation between the apex and the mental foramen (Figs. 3D, 3E and 3F).
Discussion
Paresthesia is defined as a neuro-sensory alteration resulting from a type of nerve injury called “neuropraxia”(4). Neuropraxia can be described by patients to include the following symptoms: episodic or continuous tingling, numbness or a prickling sensation, a sensation of unusual cold/warmth, or formication in the affected area which may occur secondary to local or systemic factors(4,5). Paresthesia may occur due to several conditions affecting the peripheral nervous system, including: traumatic injuries, osteomyelitis, viral infections (e.g., herpes zoster/shingles) or as a complication of a chronic systemic disease (e.g., diabetic neuropathy). Some diseases originating in or affecting the central nervous system, such as stroke or malignancies may also cause paresthesia(5,6). Trigeminal nerve injury in endodontics (presenting as paresthesia) most commonly affects the mandibular division, and has been reported to be caused by a number of factors. These include; primary apical periodontitis/periapical lesions(7,8), sealer extrusion(9,10), extrusion of intra-canal medicaments(11,12), gutta percha overfilling(13) and inadequate primary endodontic treatment causing persistent apical periodontitis(1,8,14), as demonstrated in the present case. The maxillary division of the trigeminal nerve is reportedly less affected than the mandibular division, and injury to these structures is usually the result of sodium hypochlorite extrusion(15). Several mechanisms of injury to the inferior alveolar nerve (IAN) or the mental neurovascular bundle during endodontic procedures have been reported.
Albeit uncommon, IAN injury during local anaesthetic block injection may occur due to direct mechanical stimulation of the nerve fibres, or trauma to the sheath which may lead to pressure on the nerve. Prolonged pressure to the nerve fibres can lead to nerve atrophy(16). A higher incidence of transient or permanent paresthesia has been reported with the use of prilocaine or articaine for mandibular block anaesthesia(15). Mechanical injury can be also caused by overinstrumentation, however, it is difficult to determine whether such nerve injury is due to overinstrumentation itself or overfilling, especially if treatment was completed in a single visit. Chemical injury can result from extrusion of endodontic materials into the mandibular canal. A number of case reports have demonstrated paresthesia due to paraformaldehyde neurotoxicity from materials such as AH26 or AH-plus endodontic sealers(17,18). However, many endodontic materials have a high pH, including calcium hydroxide and bioceramic sealers, which could be neurotoxic if extruded in close proximity to a neural structure(11,12). Even inert materials, such as gutta percha, could induce nerve injury if extruded into the IAN. In such cases, nerve injury may be due to a combination of direct thermal injury caused by warm gutta percha, and/or mechanical compression of the neuro-vascular bundle(6,13). Periapical inflammation due to infected root canal systems may be a causative factor for paresthesia, both in primary cases as well as failed endodontic treatments. Bacterial toxins (e.g., endotoxins of gram-negative bacteria) and metabolic by-products can cause direct nerve injury especially in teeth in close proximity to the inferior alveolar canal or the mental neurovascular bundle(1). Moreover, the inflammatory reaction towards the bacterial challenge may result in mechanical compression and ischemia of the nerve fibres. In the present case, the previously treated mandibular second premolar demonstrated apical periodontitis due to a failure to manage the complex internal anatomy during primary treatment. The missed anatomy was the source of the bacteria responsible for the persistent disease. Left untreated, the periapical lesion extended to involve the mental nerve bundle causing paresthesia. Surgical treatment was not considered in the present case due to missed anatomy in the root canal system and the proximity of the lesion to the mental nerve. Three-dimensional imaging (CBCT) provided a reliable baseline reference for recalls and the assessment of bone healing.
At the time of the 3-year recall, CBCT imaging was requested for the scheduled extraction and implant planning of the left mandibular first molar. This second CBCT scan was beneficial to help demonstrate endodontic healing of the neighbouring left second pre molar, but not was not taken primarily for this purpose.
Elimination of bacteria from the previously treated root canal system was performed using strict infection control measures, including: dental dam isolation, thorough debridement of the root canal system, a well-defined irrigation protocol, inter-appointment medication and proper sealing of the root canal system both apically and coronally. Obturation of the present case was challenging, due to a deep split and complex internal anatomy of the canal system.
Bioceramic sealer was chosen to fill these complex inter-canal communications, and single matching GP cones were placed in areas where canal shaping with reciprocating instrumentation could reliably be achieved. A dense fill of the main canals was seen, but some voids were present in areas of inter-canal communication (Fig. 2C and 2D). A small amount of sealer extrusion was furthermore seen apically. Following endodontic retreatment, healing of the apicalя periodontitis and resolution of the associated nerve injury occurred without the need for surgical intervention.
Whilst it is not known exactly how long after non-surgical retreatment the paresthesia had resolved, it is known that resolution of this condition may require several weeks, months or even years(1,19). Furthermore, mandibular second premolars are known to display complex internal anatomy at times(20), contributing to the development of the apical periodontitis in the present case.
In conclusion, long-standing untreated apical periodontitis may result in complications such as paresthesia involving a nearby neural structure. Patients should therefore be informed of this, as well as other possible sequelae of untreated periapical disease. The present case demonstrates that conservative non-surgical endodontic retreatment may be successful in managing such cases, and should be considered by clinicians prior to surgical intervention, especially where clear deficits in the existing endodontic treatment are observed. More courses in endodontic treatment are accessible for you to learn on our website in Endodontics section.
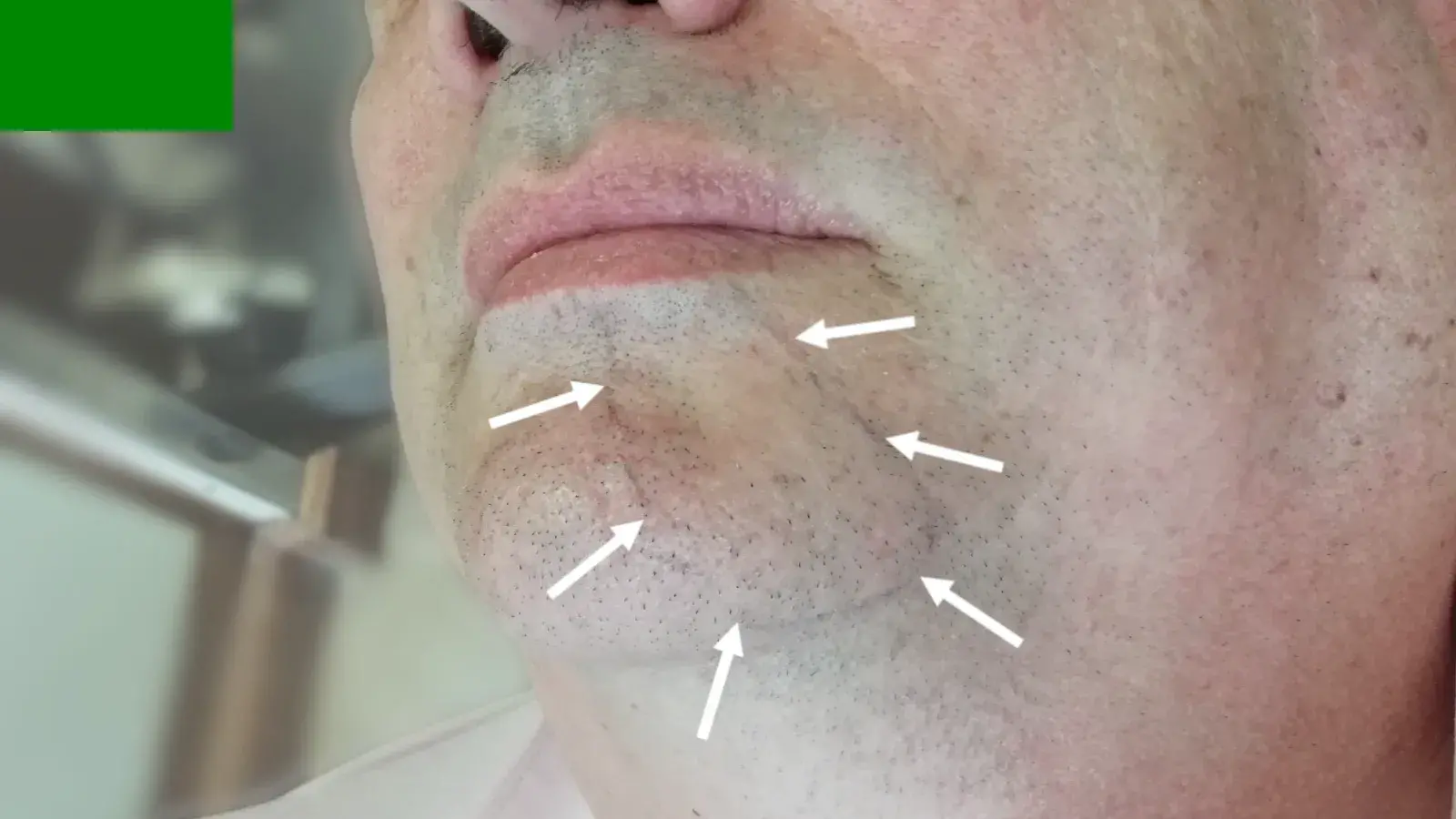 Fig. 1 The skin in the region of the left mental nerve distribution (indicated by white arrows) presented with paresthesia characterised by numbness to sensory testing. The affected area was marked using a ball-point pen
Fig. 1 The skin in the region of the left mental nerve distribution (indicated by white arrows) presented with paresthesia characterised by numbness to sensory testing. The affected area was marked using a ball-point pen
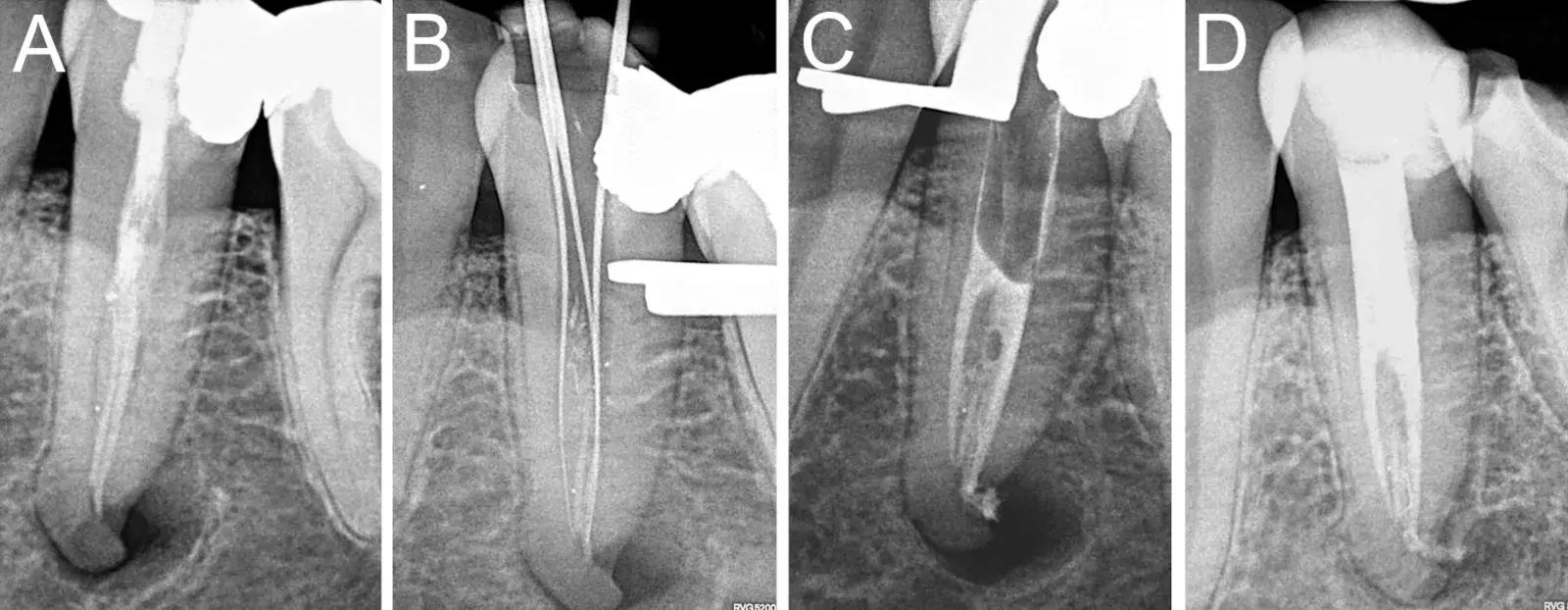 Fig. 2 (A) Periapical radiography revealed a well-defined radiolucency surrounding the apex of the left mandibular second premolar with previous endodontic treatment, involving the mental foramen. (B) The existing GP and sealer was removed and working length reestablished. (C) Bioceramic sealer and single cones were used to obturate the apical half of the canal system. (D) The 3-year follow-up periapical radiograph demonstrated good bone healing around the apex of the left mandibular second premolar and complete resolution of the paresthesia
Fig. 2 (A) Periapical radiography revealed a well-defined radiolucency surrounding the apex of the left mandibular second premolar with previous endodontic treatment, involving the mental foramen. (B) The existing GP and sealer was removed and working length reestablished. (C) Bioceramic sealer and single cones were used to obturate the apical half of the canal system. (D) The 3-year follow-up periapical radiograph demonstrated good bone healing around the apex of the left mandibular second premolar and complete resolution of the paresthesia
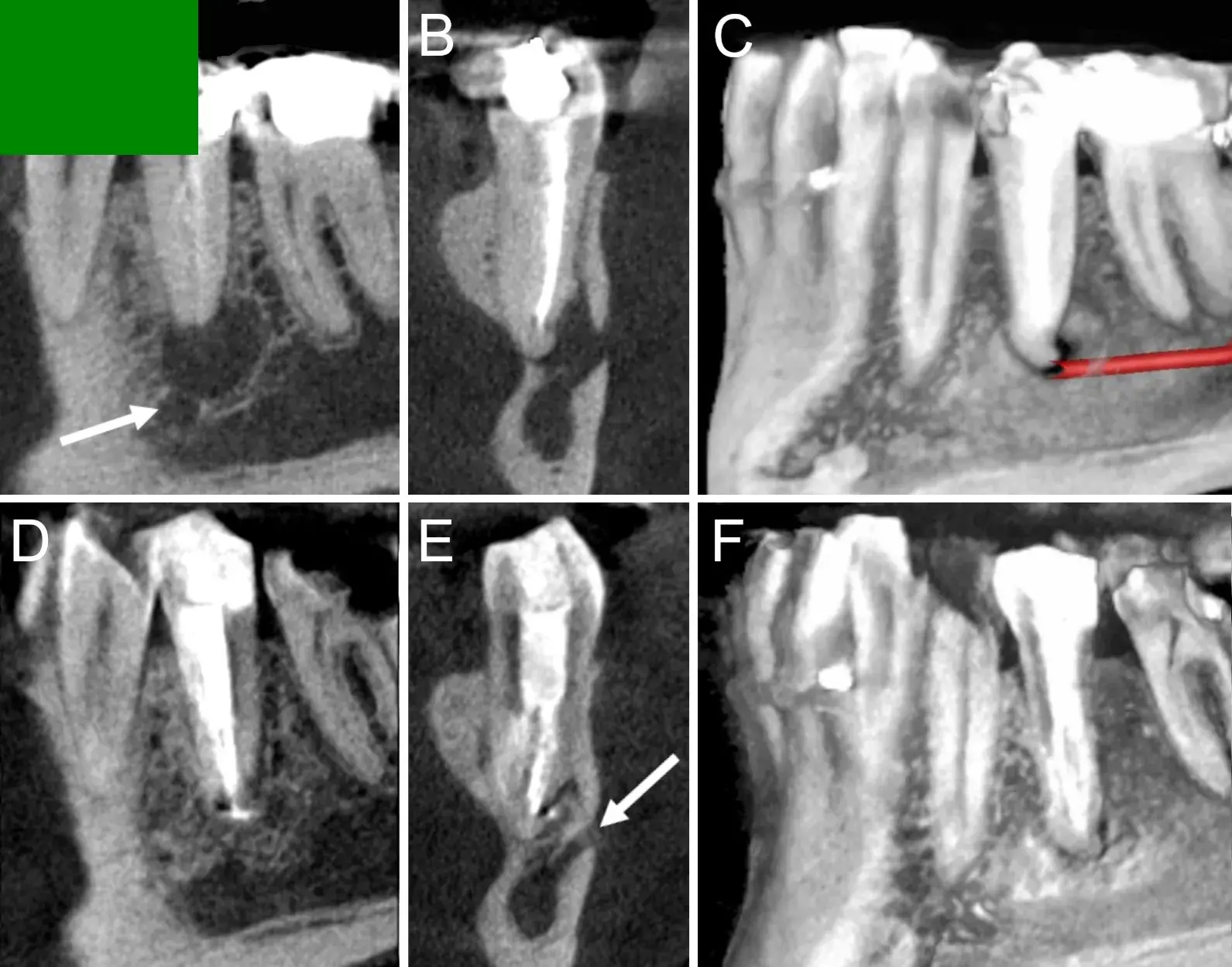 Fig. 3 Upper panel: cone-beam computed tomography (CBCT) images of the initial visit. (A) Sagittal slice showed a hypodense periapical lesion measuring 8.9 by 7.9mm with close proximity to the mental nerve (white arrow). The missed canal is evident on this view. On coronal view (B) the lesion was indistinguishable from the mental foramen. (C) Three-dimensional reconstruction and nerve mapping showed the close approximation with the periapical lesion and the inferior alveolar and mental nerve. Lower panel: CBCT images of the follow-up visit after 3 years. (D) the sagittal slice showed bone healing with the absence of a periapical lesion. On coronal view (E), the healing is apparent by cortication and narrowing of the mental foramen (white arrow. (F) Three-dimensional reconstruction showed the extent of bone fill and healing in the periapical region
Fig. 3 Upper panel: cone-beam computed tomography (CBCT) images of the initial visit. (A) Sagittal slice showed a hypodense periapical lesion measuring 8.9 by 7.9mm with close proximity to the mental nerve (white arrow). The missed canal is evident on this view. On coronal view (B) the lesion was indistinguishable from the mental foramen. (C) Three-dimensional reconstruction and nerve mapping showed the close approximation with the periapical lesion and the inferior alveolar and mental nerve. Lower panel: CBCT images of the follow-up visit after 3 years. (D) the sagittal slice showed bone healing with the absence of a periapical lesion. On coronal view (E), the healing is apparent by cortication and narrowing of the mental foramen (white arrow. (F) Three-dimensional reconstruction showed the extent of bone fill and healing in the periapical region
List of authors:
Glynn Dale Buchanan, Chane Smit, Mohamed Yasin Gamieldien, Ahmed S. ElSheshtawy
References
Ricucci D, Loghin S, Siqueira JF. Complicated untreated apical periodontitis causing paraesthesia: A case report. Aust Endod J. 2018;44:281–285. Doi: 10.1111/aej.12220.
Nair PNR. On the causes of persistent apical periodontitis: A review. Int Endod J. 2006;39:249–281. Doi: 10.1111/j.1365-2591.2006.01099.x.
Robinson PP, Smith KG, Johnson FP, et al. Equipment and methods for simple sensory testing. Br J Oral Maxillofac Surg. 1992;30:387–389. Doi: 10.1016/0266-4356(92)90206-X.
Tsesis I, Taschieri S, Rosen E, et al. Treatment of paresthesia following root canal treatment by intentional tooth replantation: A review of the literature and a case report. Indian J Dent Res. 2014;25:231–235.
Lambrianidis T, Molyvdas J. Paresthesia of the inferior alveolar nerve caused by periodontal-endodontic pathosis. Oral Surg Oral Med Oral Pathol. 1987;63:90–92.
Krishnan U, Moule AJ. Mental nerve paraeshesia: A review of causes and two endodontically related cases. Saudi Endod J. 2015;5:138–145. Doi: 10.4103/1658-5984.155454.
Von Ohle C, Elayouti A. Neurosensory impairment of the mental nerve as a sequel of periapical periodontitis: Case report and review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e84–89. Doi: 10.1016/j.tripleo.2010.03.033.
Devine M, Yilmaz Z, Hirani M, et al. A case series of trigeminal nerve injuries caused by periapical lesions of mandibular teeth. Br Dent J. 2017;222:447–455. Doi: 10.1038/sj.bdj.2017.268.
López-López J, Estrugo-Devesa A, Jané-Salas E, et al. J. Inferior alveolar nerve injury resulting from overextension of an endodontic sealer: Non-surgical management using the GABA analogue pregabalin. Int Endod J. 2012;45:98–104. Doi: 10.1111/j.1365-2591.2011.01939.x.
Froes FGB, Miranda AMMA, Abad EDC, et al. Non-surgical management of paraesthesia and pain associated with endodontic sealer extrusion into the mandibular canal. Aust Endod J. 2009;35:183–186. Doi: 10.1111/j.1747-4477.2009.00163.x.
Kasapoğlu MB, Dogancali GE. Inferior alveolar nerve injury due to the extrusion of calcium hydroxide during endodontic treatment: A case report. Aust Endod J. 2022;48:342–346. Doi: 10.1111/aej.12650.
Montenegro Fonsêca J, Palmier NR, Amaral-Silva GK, et al. Massive extrusion of calcium hydroxide paste containing barium sulphate during endodontic treatment. Aust Endod J. 2020;46:257–262. Doi: 10.1111/aej.12382.
De Souza JC, Machado R, Batts RA, et al. Inferior alveolar nerve paraesthesia after overfilling into the mandibular canal, confirmed by cone-beam computed tomography: A case report. Brazilian Dent Sci. 2021;24:1–8. Doi: 10.14295/bds.2021.v24i2.2421.
Devine M, Modgill O, Renton T. Mandibular division trigeminal nerve injuries following primary endodontic treatment. A case series. Aust Endod J. 2017;43:56–65. Doi: 10.1111/aej.12209.
Pelka M, Petschelt A. Permanent mimic musculature and nerve damage caused by sodium hypochlorite: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:e80–83. Doi: 10.1016/j.tripleo.2008.05.003.
Shimpo T, Gilliatt RW, Kennett RP, et al. Susceptibility to pressure neuropathy distal to a constricting ligature in the guinea-pig. J Neurol Neurosurg Psychiatry. 1987;50:1625–1632.
Coskunses FM, Sinanoglu A, Helvacioglu-Yigit D, et al. The extrusion of root canal cement containing paraformaldehyde into the inferior alveolar nerve canal resulting in infection and numbness. Int Endod J. 2016;49:610–617. Doi: 10.1111/iej.12510.
Ahonen M, Tjäderhane L. Endodontic-related paresthesia: A case report and literature review. J Endod. 2011;37:1460–1464. Doi: 10.1016/j.joen.2011.06.016.
Ozkan BT, Celik S, Durmus E. Paresthesia of the mental nerve stem from periapical infection of mandibular canine tooth: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e28–31. Doi: 10.1016/j.tripleo.2008.01.023.
Buchanan GD, Gamieldien MY, Fabris-Rotelli I, et al. A study of mandibular premolar root and canal morphology in a Black South African population using cone-beam computed tomography and two classification systems. J Oral Sci. 2022;64:300–306. Doi: 10.2334/josnusd.22-0027.

/social-network-service/media/default/100727/b4c9a4c2.jpg)
