Periodontal techniques of local anesthesia
Machine translation
Original article is written in RU language (link to read it).
The main object in the vast majority of outpatient interventions at a dental appointment is the hard tissue of the tooth. At the same time, anesthesia of the tissues surrounding the teeth is often not only unnecessary, but also undesirable.
Over the course of many years of practice, local anesthesia techniques have been developed that allow anesthesia of tooth tissue and a small area of surrounding tissue.
About new strategies for local anesthesia in dentistry at the webinar New techniques for effective local anesthesia in endodontics .
These pain relief techniques are called periodontal, they include the following:
intraligamentary anesthesia;
intraseptal anesthesia;
intraosseous anesthesia.
All of the above methods according to the mechanism of pain relief are representatives of infiltration anesthesia. The key route for penetration of the anesthetic solution into the dental tissues is the bone marrow space.

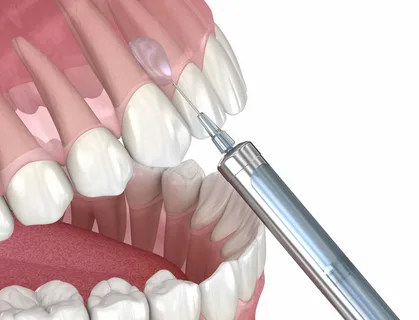
Rice. 1. Conducting intraseptal anesthesia.
Routes of distribution of anesthetic
After entering the bone space, the anesthetic solution spreads further in the following ways.
First way
The diffusion of the solution occurs directly through the bone tissue, the bone marrow space of the tooth socket and interdental septa. The nerve endings located here, which innervate the pulp and periodontium, are gradually blocked.
The diffusion of the anesthetic is determined by the pressure and volume of the incoming solution. In case of weak pressure, the entire volume of anesthetic drug remains in the injection zone, creating a high local concentration and guaranteeing effective anesthesia. The injection is made directly near the tooth, so effective pain relief occurs with a volume of the drug that is significantly smaller than with conventional methods - 0.2-0.6 ml. In this regard, effective pain relief occurs with intraligamentary anesthesia in one tooth, and with intraosseous and intraseptal anesthesia in two adjacent teeth.
Second way
Caused by the penetration of the drug into the bloodstream. From the injection zone, the anesthetic spreads through capillaries to the maxillary sinus and nasal cavity during anesthesia in the upper jaw, and in the lower jaw - towards the mandibular canal. With such a vertical movement, three levels are distinguished in which the solution moves mainly horizontally:
large veins located in the transitional fold represent one horizontal tier, it is located at the level of the crowns and roots of the teeth;
the next horizontal level is represented by a finely looped plexus, located in the area of the apexes of the roots, covering the teeth adjacent to the area of insertion;
the last horizontal tier is the periodontal plexus, intraosseous blood vessels and plexuses located in the sinus and mandibular canal.

Rice. 2. Periodontal pain relief techniques are the option of choice at a children’s appointment.
Through the vessels located in the first and last levels, the injected anesthetic flows out. To reduce the outflow during periodontal anesthesia techniques, local anesthetic drugs with vasoconstrictors are used, this makes it possible to reduce the volume of the injected solution. Blood vessels are filled in the direction of blood flow, as well as against the flow under the influence of injection pressure, as a result the capillaries of the pulp and intraosseous tissues are filled with solution. Due to the spread of the solution, maximum bleeding of the pulp and periodontal tissue occurs, which is not observed with other methods of anesthesia. Clinically, this can be determined by the whitening of the tissue near the injection site.
Indications for periodontal pain relief techniques
Treatment and removal of teeth that are located far from each other, on different jaws.
Surgical procedures in children, which reduces the risk of soft tissue damage due to burns or biting.
Treatment of patients with concomitant diseases to prevent complications, since the volume of injected solution is significantly reduced.
Surgical treatment of patients for whom nerve blockade is contraindicated.
Intraligamentary anesthesia
Intraligamentous anesthesia is one of the methods of local anesthesia, which involves the introduction of a local anesthetic drug into the periodontal space. A feature of this method of anesthesia is the injection of the solution under higher pressure than with other methods. With proper administration, a small proportion of the anesthetic remains inside the gap of the periodontal space, the main volume of liquid diffuses into the intraosseous space of the bone tissue, spreading further into the periapical region.

Rice. 3. Instruments for intraligamentary anesthesia.
Advantages
almost instant effect, pain relief occurs within the first minute;
duration of anesthesia is about 20 minutes;
the procedure is slightly painless;
there is no feeling of soft tissue numbness as a result of the injection.
Advantages in pediatric practice
prevention of hematomas and biting of numb soft tissues;
ease of bite correction during therapeutic treatment;
less toxicity of drugs due to the minimum volume of injected solution.
To carry out intraligamentary anesthesia, special injectors are required, their advantages:
ensuring the high level of pressure required for injection;
the presence of a solution dosing system (up to 0.06 ml of the drug);
equipped with a rotating head or an angular attachment, which allows you to change the inclination of the needle relative to the tooth;
the manufacturing material guarantees simplicity and convenience of sterilization;
convenient to use.
Anesthesia technique
Carrying out professional hygiene, the gingival groove and adjacent tooth tissues are subjected to antiseptic treatment.
The injection is made into the periodontal space with constant pressure.
Having positioned the needle at an angle of 30°, it is advanced along the tooth, the gingival groove is punctured, the needle slides to a depth of up to 3 mm until resistance occurs.
A clinical sign of correct technique is the appearance of gingival ischemia.
To provide pain relief in the incisor area, only 0.1–0.2 ml of solution is needed.
The main requirement is a low rate of drug delivery. The injector injects 0.06 ml of solution over 7 seconds.
Anesthesia is performed on approximal surfaces, in multi-rooted teeth - in the area of each root.
The area of anesthesia is limited to only one tooth, into the ligament of which the anesthetic has penetrated.
Rice. 4. Method of periodontal anesthesia.
Intraseptal anesthesia
Intraseptal anesthesia is a type of intraosseous anesthesia in which the anesthetic must enter the bone septum separating the tooth sockets.
The mechanism of onset of anesthesia is based on the distribution of the anesthetic in the following ways:
through the bone marrow space,
by intravascular distribution along the vascular bed of periodontal and bone marrow substances.
Result of intraseptal anesthesia
blockade of the transmission of nerve impulses within bone structures, as well as soft tissues,
ischemia of periodontal tissues,
enhanced analgesic effect due to hypoxia of nerve endings.
Technique
The needle is inserted into the bone directly of the interdental septum.
A short needle is used, its initial position is at a right angle to the pierced gum surface.
Add 0.2 ml of solution, then you need to push the needle deeper so that it rests on the bone, and then, overcoming resistance, push the needle into the bone structure of the septum by 1.5-2 mm.
The slower the injection of 0.2-0.6 ml of solution is performed, the smaller the area of penetration of the anesthetic solution will be.
The anesthesia zone is not extensive and does not extend beyond the adjacent teeth and surrounding tissues.
The short duration of anesthesia is due to the rapid resorption of the small volume of the injected drug.

Rice. 5. Scheme of intraligamentary anesthesia.
Features of intraseptal anesthesia technique
It is difficult to determine the injection point, since it must be at the same distance from neighboring teeth and correspond to the top of the interdental septum. Intraseptal anesthesia has become more widespread when carrying out various manipulations on the lower jaw; here the cortical layer has a minimum thickness just at the top of the interdental septum. The septal bone is located a few millimeters downward from the protrusion of the gums, but due to periodontal disease, this distance changes significantly. Radiography allows us to determine the exact location of the apex of the septum.
The introduction of the solution should be accompanied by high resistance, which is better felt when using a conventional syringe. Resistance is evidence that the solution is penetrating the bone and not the soft tissue. The solution should not be poured into the patient's mouth. In this case, it is necessary to redirect the needle and immerse it a little deeper.
This method of pain relief is effective, simple, minimally traumatic and has no post-injection pain.
More detailed information on this topic in the online lesson Local anesthesia: modern problems .


