Outcome of Endodontic Treatment through Existing Full Coverage Restorations: An Endodontic Practice Case Series
ABSTRACT
Introduction: This case series assessed the outcome of nonsurgical endodontic treatment completed through retained full coverage restorations (FCRs) in a board-certified endodontist private practice. The number of cases completed by the first author was 153. You have the opportunity to gather more in-depth information about complex cases treatment in our course "Saving hopeless teeth: surgical and conservative protocols".
Methods: All cases were performed following a standardized protocol for treatment and restoration depending on the type of FCR. Number of cases that showed up for 2- to 4-year follow-up was 127, with 83% recall rate. The age range of patients was 33–95 years, with mean age of 54.734 years. The mean recall time was 2.448 years. FCRs and their distribution were as follows: 4 anterior teeth, 14 premolars, and 109 molars. There were 103 nonsurgical root canal treatments and 24 retreatments. Patients who presented for recall had 74 porcelain fused to metal crowns, 17 zirconia crowns, 15 abutments of porcelain fused to metal bridges, 14 lithium disilicate crowns, 5 gold crowns, 1 full metal crown, and 1 gold onlay.
Results: There were no endodontically related failures. Six cases failed; 3 were due to vertical root fractures, 1 was due to horizontal root fracture, and 2 were due to extensive recurrent caries causing restorative failure. The percentage of healed cases following the American Association of Endodontists outcome criteria adopted in 2004 with intact retained FCR was 95.3%.
Conclusions: The results suggest predictable favorable outcomes for nonsurgical endodontic treatment through FCR following the proposed protocol for diagnosis, treatment, and restoration. (J Endod 2021;-:1–8.)
Full coverage restorations (FCRs) have been used for many years to restore esthetics, form, occlusion, and function. Although they have shown satisfactory clinical performance, mechanical and biological complications still occur that can affect the integrity of crown and/or the tooth[1–3]. It is important to acknowledge that FCRs are prescribed to restore and protect compromised teeth that have been damaged by wear, trauma, or cycles of caries and repair[4]. Loss of pulp vitality is the most frequently reported biological complication, with an incidence rate of 2.1% at 5 years and can be as high as 15%[2,5]. Furthermore, the risk for endodontic biological complication after crown therapy is higher after receiving more esthetically pleasing FCRs and with younger age[6]. The primary objective of nonsurgical endodontic treatment is the healing of existing, as well as prevention of recurrence of, apical periodontitis[7]. This objective can be fulfilled by disinfection of persistent residual microbes present in the root canal system[8]. In many cases of primary endodontic treatments (RCT), the tooth may have an intact FCR, presenting a physical barrier against entry into the root canal system. Similarly, but with more complexity, nonsurgical retreatments (RETX) may exhibit additional challenges regarding access to the root canal system because of the presence of intracanal filling materials, violated anatomy, intracanal impediments such as separated instruments, and possibly retention elements such as posts[9]. In these clinical scenarios, clinicians are faced with 1 of 2 options, either to treat and replace the existing FCR or to perform endodontic treatment through the existing FCR followed by access cavity repair using a direct restoration. Although the latter is more economical because of the reduced overall treatment time and cost, it presents with a mechanical risk of failure of the accessed repaired crown by fracture or loss of retention[10,11], in addition to a biological risk of recurrent caries being left behind.
After nonsurgical endodontic procedures in teeth with existing FCRs, a high quality coronal restoration for the prepared access cavity is critical to prevent percolation of microorganisms[12]. Although the prognosis of nonsurgical endodontic procedures is dependent on the technical qualities of the root filling[13,14], some studies have shown that the quality of coronal restoration has a more significant role in the outcome of treatment[15,16]. Technological advancements in endodontics such as the dental operating microscope[17], ultrasonic instruments[18,19], as well as cone-beam computed tomography (CBCT)[20] provided clinicians with minimally invasive strategies to address disease etiology and more predictable decision-making process.
Several in vitro studies investigated and compared the performance of control non-accessed with accessed repaired crowns, and the results have been conflicting[21–26]. Therefore, clinical evidence-based best practice guidelines have not been established yet to manage crowned teeth in need for endodontic therapy. Furthermore, clinical data on the performance of accessed and repaired FCRs are lacking. Therefore, the aim of this case series observational study was to assess the endodontic and restorative outcome of accessed and repaired FCRs while using same armamentarium and materials for each type of FCR.
MATERIALS AND METHODS
The treated patient cohort was referred to the first author’s practice for endodontic treatment. Patients had clinical and radiographic diagnostic workup for pulpal and periapical diagnoses in addition to periodontal and restorative assessment. After discussion of treatment options and election of endodontic treatment, a signed informed consent was obtained. One hundred fifty-three patients had treatment completed (during the period 2016–2019) through existing FCR after fulfilling all the following inclusion criteria:
Patient is comfortable with occlusion and esthetics.
Clinically intact margins with no clinical or radiographic signs of recurrent caries.
Clinically and radiographically intact proximal contact with no food impaction or signs of impingement on gingival tissue or negative effect on the periodontal status of the tooth.
Absence of signs of fracture and/or cracking in the restoration.
FCR is still retentive on completion of treatment.
All teeth treated in the study had to be functional and showed opposing occlusion that was confirmed with shim stock.
A preoperative bitewing radiograph was taken for each patient in addition to any other radiographic evaluation for proper restorative and periodontal assessment. Strict use of dental operating microscope for examination and treatment was done to check intact extracoronal margins upon explorer probing, and no detection of intracoronal leakage or recurrent caries occurred (Fig. 1).
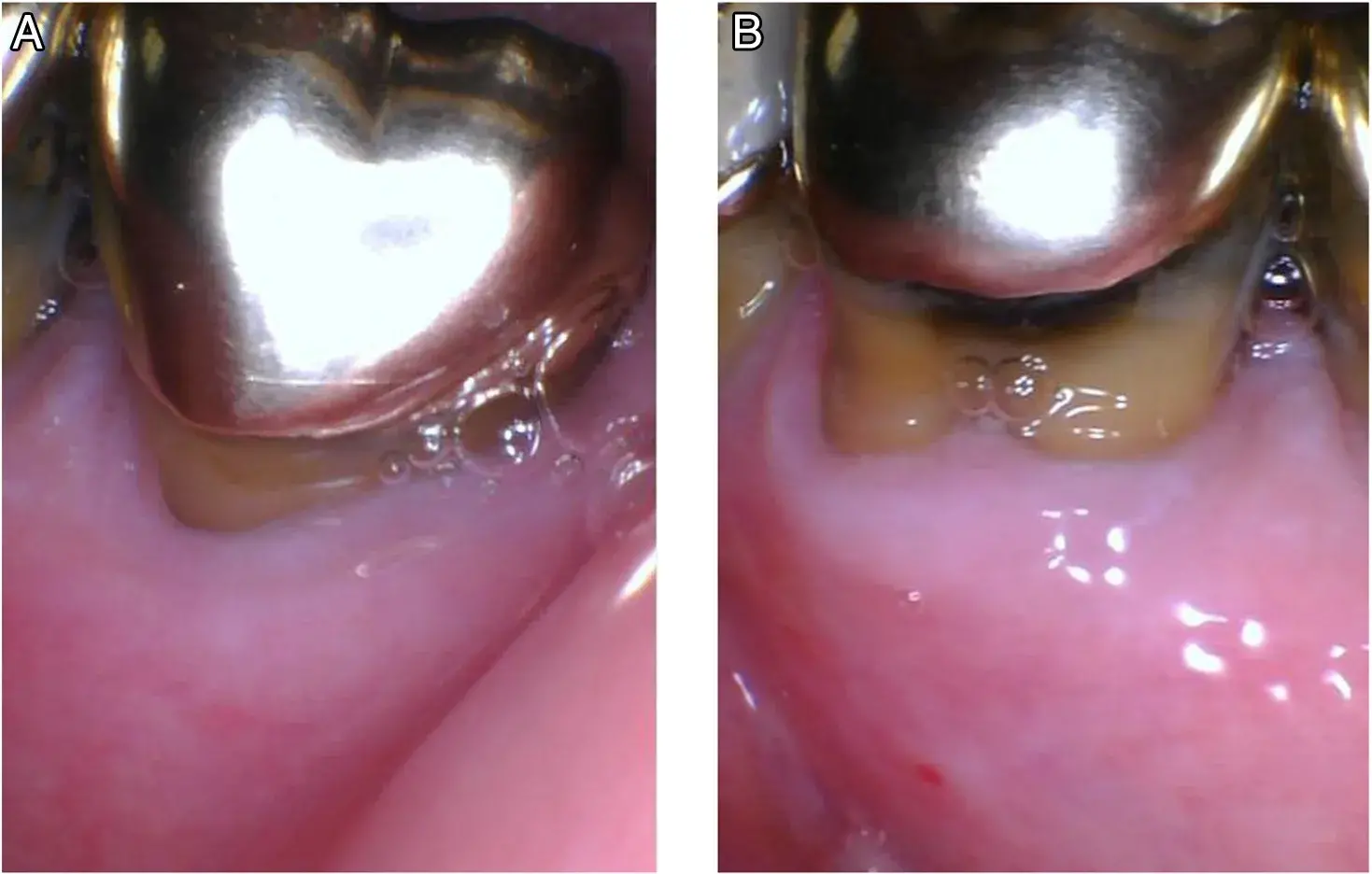 FIGURE 1 – (A ) Intact gold crown margin that was retained, and treatment was performed through crown. (B ) Recurrent caries affecting gold crown, and it had to be sacrificed before treatment.
FIGURE 1 – (A ) Intact gold crown margin that was retained, and treatment was performed through crown. (B ) Recurrent caries affecting gold crown, and it had to be sacrificed before treatment.
Treatment Protocol
All patients were treated by the first author following the same treatment protocol. The type of bur used for access cavity preparation was determined according to the type of the restoration. Carbide burs were used for gold and metal restorations, and diamond burs were used for zirconia and lithium disilicate restorations. For porcelain fused to metal (PFM) restorations, diamond burs were used for the porcelain part, and carbide crosscut fissure burs (transmetal burs) (Dentsply Maillefer, Tulsa, OK) were used for access through the metal framework. Diamond burs used had coarse grit size (Fig. 2).
The use of dental operating microscope with enhanced magnification and illumination facilitated conservative access cavity preparations to allow for proper irrigation and instrumentation while preserving sound tooth structure (Fig. 2).
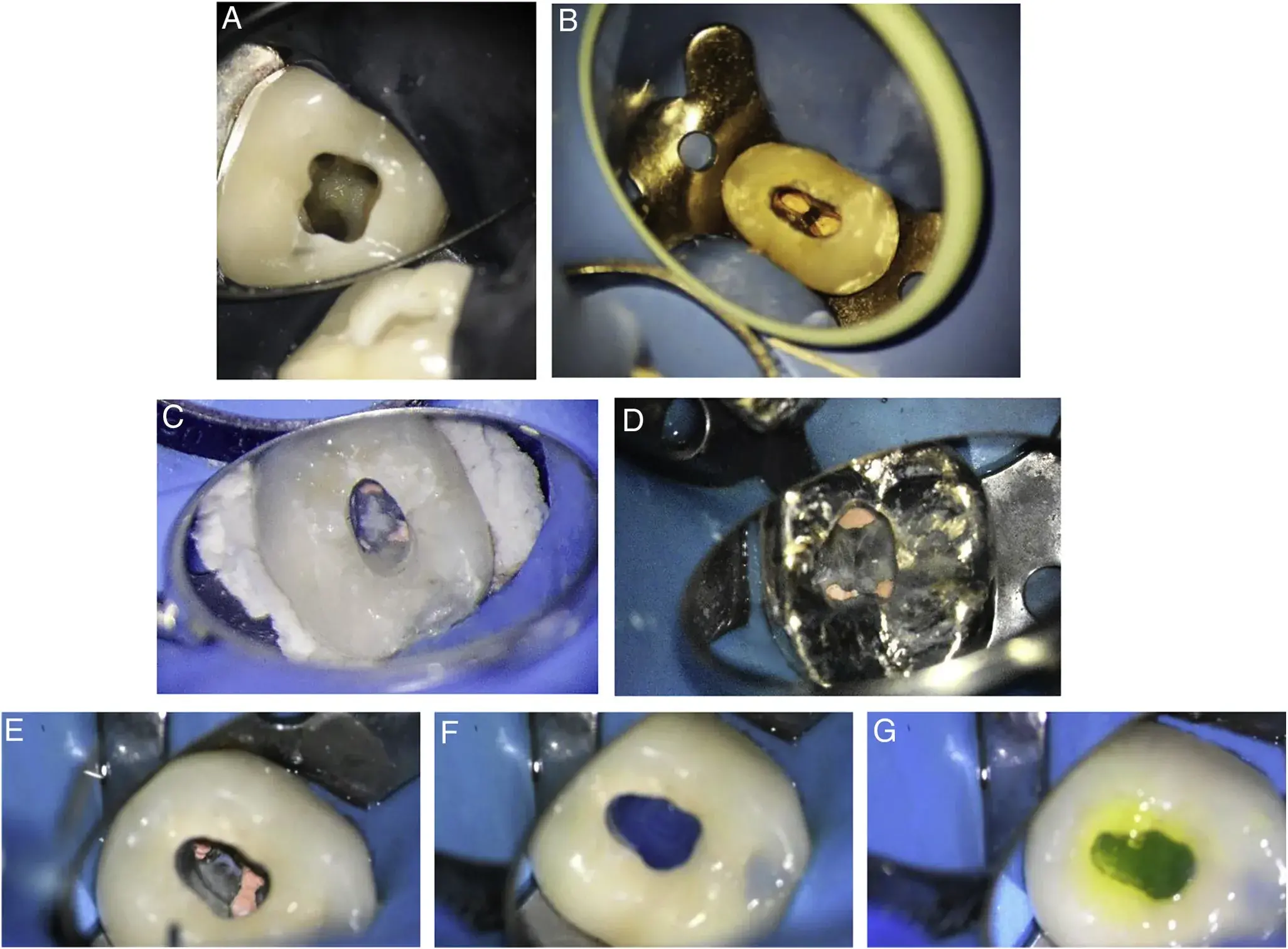 FIGURE 2 – Access cavity preparations through intact zirconia (A ), PFM (B ), lithium disilicate (C), and gold (D ) crowns. Cleaned access cavity through PFM crown from remnants of obturation materials (E ). Acid etch for dentin part (F ). Porcelain etch application for porcelain interface before water rinse (G).
FIGURE 2 – Access cavity preparations through intact zirconia (A ), PFM (B ), lithium disilicate (C), and gold (D ) crowns. Cleaned access cavity through PFM crown from remnants of obturation materials (E ). Acid etch for dentin part (F ). Porcelain etch application for porcelain interface before water rinse (G).
In cases of questionable crown orientation, stepped access cavity preparations were performed to expose dentin, regain alignment, and avoid unnecessary removal of sound tooth structure and FCR. Surgical length round bur was used for deroofing of the pulp chamber. Tapered diamond stone with round end was used to smooth axial walls. All drilling was under continuous water cooling and high-volume suction. In cases of multivisit treatment, teeth were temporized with sterile sponge and Cavit (3M, St Paul, MN). Temporary filling removal was achieved by using a bur for the core of the material, and diamond coated ultrasonic tips were used to clean margins and avoid further drilling through existing FCR. Nonsurgical root canal treatments had preoperative diagnoses of either symptomatic irreversible pulpitis or pulpal necrosis that did not alter the endodontic or the restorative treatment. After completion of treatment and depending on the type of FCR, the restorative material for access cavity was determined.
Amalgam was used for gold onlays, metal crowns, and gold crowns. Composite was used for PFM crowns and abutments, zirconia crowns, and lithium disilicate crowns. One case was restored with fiber post and composite build-up because of lack of full
circumferential dentin under the microscope in a retreatment for a mandibular premolar that was a PFM bridge abutment.
Amalgam restorations were placed in increments with condensation between increments and finalized by carving, burnishing, and occlusion check. Composite restorations were placed using LuxaCore Z Dual bulk fill composite (DMG America, Ridgefield Park, NJ) after the application of 35% phosphoric acid etch (Ultra-Etch; Ultradent, South Jordan, UT), 9.6% hydrofluoric acid gel for porcelain etch (Pulpdent, Watertown, MA) for 20 seconds, bonding agent for dentin (PQ1; Ultradent), and silane coupling agent for porcelain (Pulpdent) (Fig. 2). Light cure was performed following manufacturer instructions and then occlusion check and polishing.
Over the course of follow-ups, teeth were evaluated clinically under the microscope and radiographically using digital periapical and bitewing radiographs. Cases were deemed successful if the tooth was asymptomatic and healed according to American Association of Endodontists outcome terminology[27]. In addition, the FCR had no marginal recurrent caries and no periodontal compromise affecting gingival health or periodontal probing.
RESULTS
A total of 153 patients with completed treatment through intact FCRs were included in this case series. One hundred twenty-seven patients presented for 2- to 4-year recall (mean, 2.45 years), with recall rate of 83%. The age range of patients was 33–95 years, with mean age of 54.734 years. Patients who presented for recall had different FCRs as follows: 74 single PFM crowns, 17 zirconia crowns, 15 abutments of PFM bridges, 14 lithium disilicate crowns, 5 gold crowns, 1 full metal crown, and 1 gold onlay. Successful cases maintained (102 cases) or regained (19 cases) intact lamina dura while being asymptomatic, and FCRs were clinically and radiographically intact (Fig. 3). Success rate was 95.3% with 6 failed cases. Failures were due to vertical root fracture (VRF) (n 5 3), horizontal root fracture (HRF) (n 5 1), and extensive recurrent caries leading to restorative failure (n 5 2). Failed cases were evenly divided between primary endodontic treatment and nonsurgical retreatment patients. No endodontic failures were observed (Table 1).
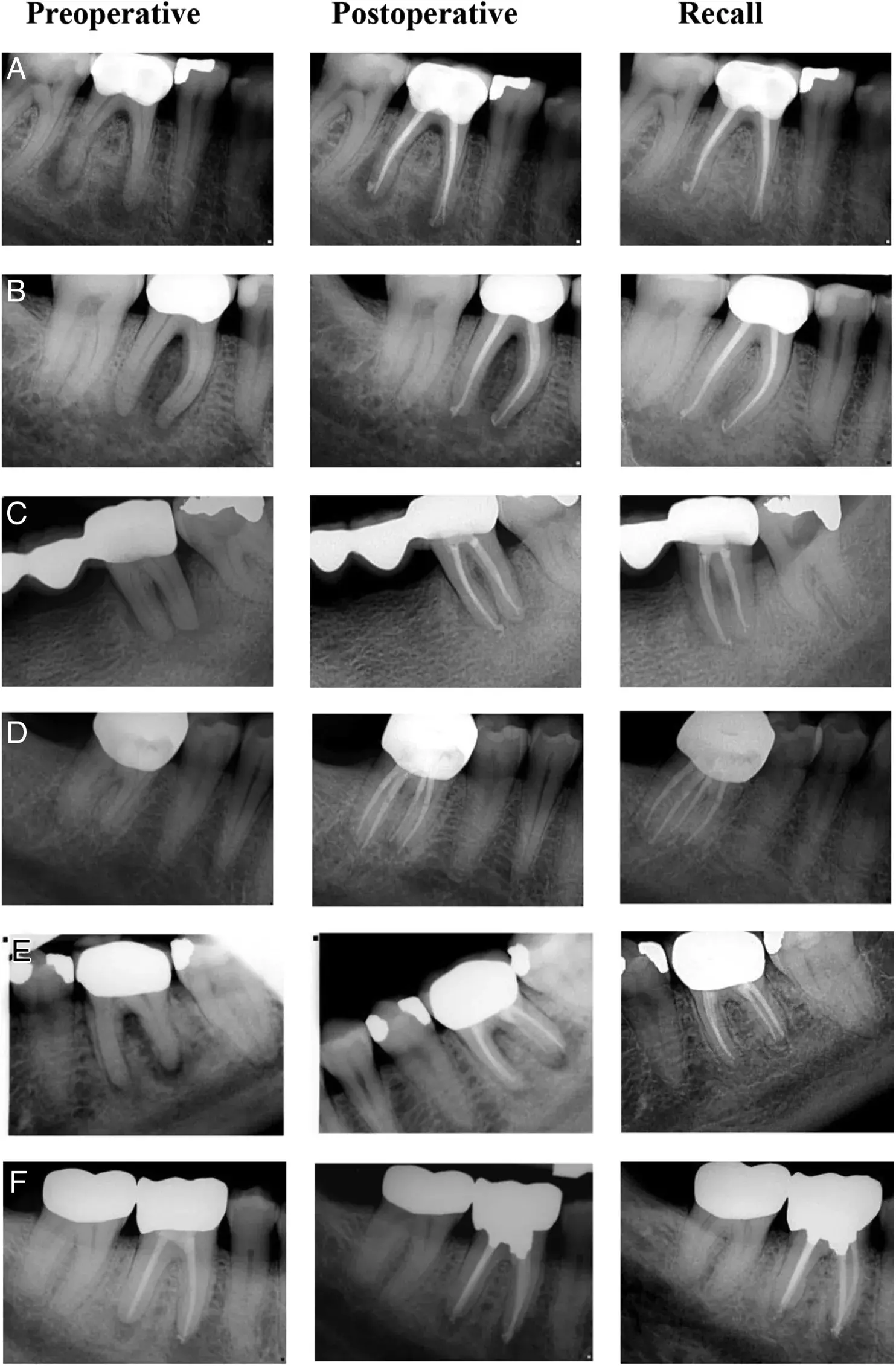 FIGURE 3 – Preoperative, postoperative, and recall periapical radiographs showing complete healing with intact crowns. Cases A, B, and C were diagnosed with pulp necrosis and symptomatic apical periodontitis. Case D was diagnosed with symptomatic irreversible pulpitis and normal apical tissues. Case E was diagnosed with pulp necrosis and chronic apical abscess. Case F was diagnosed with previous treatment and symptomatic apical periodontitis.
FIGURE 3 – Preoperative, postoperative, and recall periapical radiographs showing complete healing with intact crowns. Cases A, B, and C were diagnosed with pulp necrosis and symptomatic apical periodontitis. Case D was diagnosed with symptomatic irreversible pulpitis and normal apical tissues. Case E was diagnosed with pulp necrosis and chronic apical abscess. Case F was diagnosed with previous treatment and symptomatic apical periodontitis.
TABLE 1 - Distribution of Recalled Cases according to Type of Restoration, Tooth Type, and Procedure Performed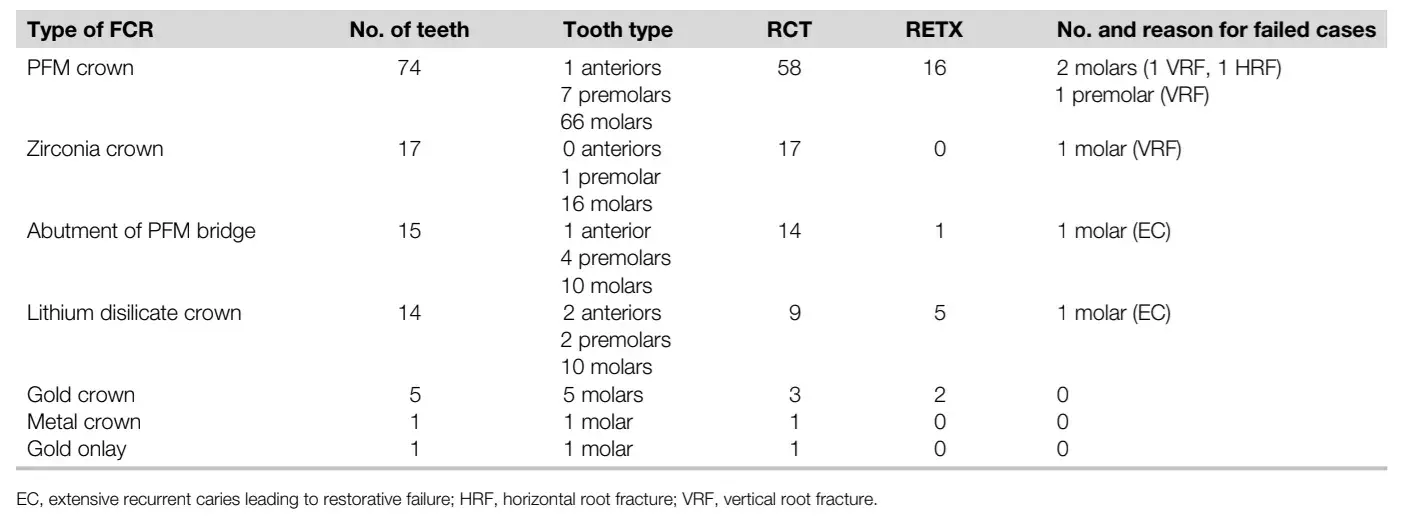
Over the course of recalls, 1 PFM crown was replaced because of fracture of lingual porcelain after 3 years of endodontic treatment, and 1 zirconia crown was replaced because of crown fracture 1 year after endodontic treatment. Both crowns were replaced with same type of crown. One PFM crown had small porcelain chipping that had composite repair unrelated to access cavity seal 1.5 years after endodontic treatment. Crown repairs did not affect endodontic outcome (Fig. 4).
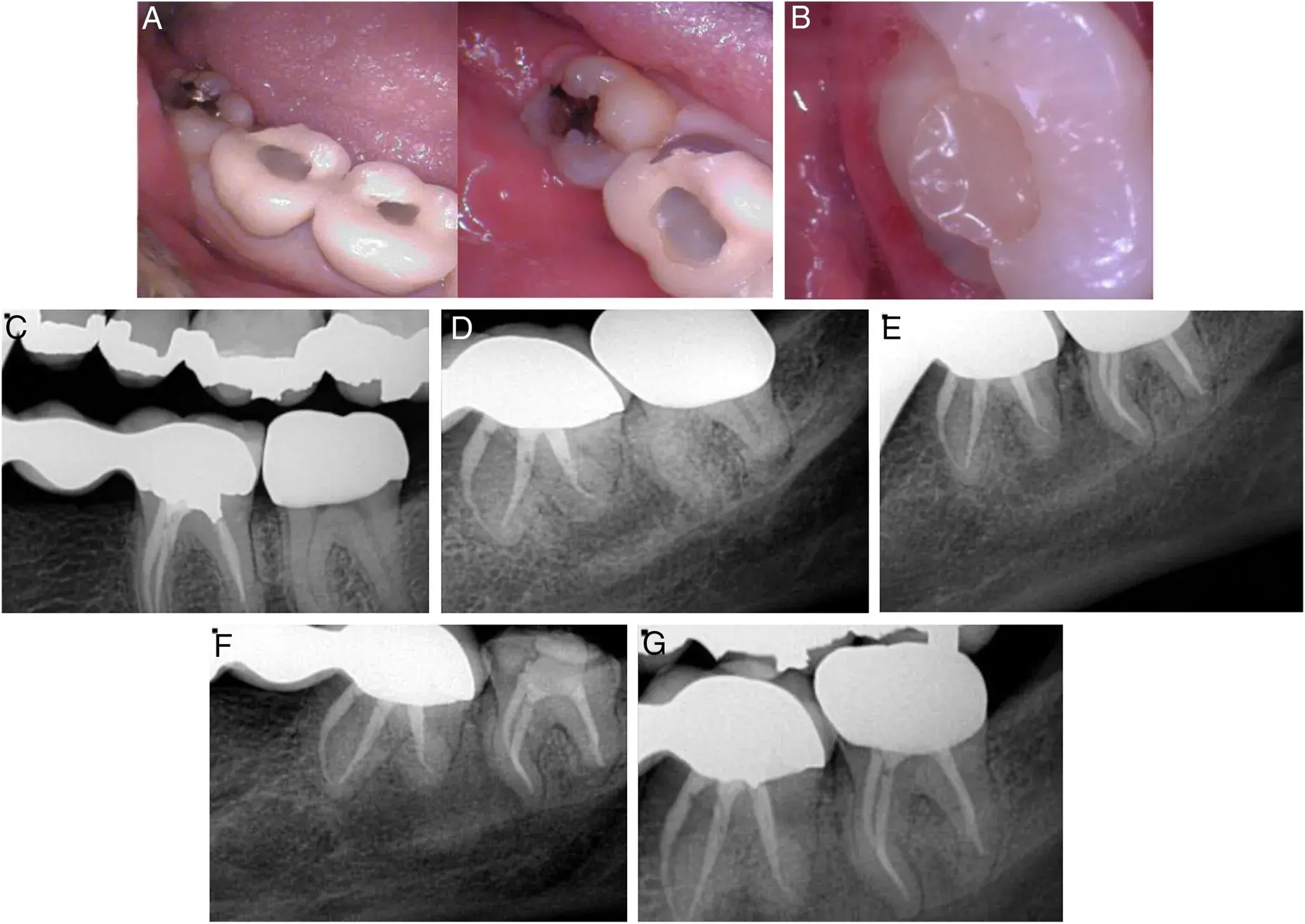 FIGURE 4 – (A ) PFM crown needed replacement because of lingual porcelain fracture. (B ) Fracture zirconia crown with no impact on endodontic status as demonstrated in (C–G ). (C) Intact preoperative bitewing. (D) Preoperative radiograph. (E) Immediate postoperative radiograph. (F )Radiograph at the time of crown replacement. (G ) Recall radiograph showing intact lamina dura.
FIGURE 4 – (A ) PFM crown needed replacement because of lingual porcelain fracture. (B ) Fracture zirconia crown with no impact on endodontic status as demonstrated in (C–G ). (C) Intact preoperative bitewing. (D) Preoperative radiograph. (E) Immediate postoperative radiograph. (F )Radiograph at the time of crown replacement. (G ) Recall radiograph showing intact lamina dura.
DISCUSSION
It is noteworthy that FCRs were retained in this study regardless of their time in service if they satisfied all screening criteria. Saving existing FCR may be an economical goal for the patient, which links up with the findings of this study that show a predictable favorable outcome for endodontic treatment through intact FCR when the aforementioned clinical protocol for diagnosis and treatment planning is followed. Interestingly, the treatment approach was not linked to any procedural errors such as perforations, missing anatomy, and did not jeopardize the crown or tooth longevity. These findings can be attributed to the use of contemporary armamentarium including CBCT, microscope, and ultrasonics, which facilitated conservative treatment of endodontic disease. Evaluation of the healing status can certainly have different interpretation with CBCT vs periapical radiographs. However, the recall plan for the present study followed the American Association of Endodontists and American Academy of Oral and Maxillofacial Radiology joint position statement regarding the use of CBCT published in 2015 with 2016 update. Particularly, recommendation 13 was noted, “In the absence of clinical signs or symptoms, intraoral radiographs should be considered the imaging modality of choice for the evaluation of healing following nonsurgical and surgical endodontic treatment” [28].
Cuspal coverage restorations are recommended for endodontically treated teeth, especially posterior teeth[29]. However, when nonsurgical retreatment was needed for patients in this study, the retention of existing intact FCR did not present a procedural challenge and did not negatively impact the outcome.
Furthermore, a prompt final restoration after endodontic therapy is recommended for adequate seal of the root canal system[30]. Access through intact FCR and repair achieves that goal because the patient receives the final coronal seal under existing rubber dam isolation, protecting the patient from salivary contamination as well as potential chemical hazards of using hydrofluoric acid.
For an ideal bonding at the ceramic resin interface, various surface treatments are indicated depending on the type of ceramic used. Glass-based ceramics require surface treatment with hydrofluoric acid, followed by the application of silane coupling agent; this treatment provides both micromechanical and chemical bond[31,32]. Different concentrations of hydrofluoric acid are available with different application times. Further details about endodontic treatment protocols are accessible for you to learn on our website in the Endodontics section.
Levartovsky et al[31] showed that the application of 9% hydrofluoric acid for 20 seconds resulted in higher shear bond strength between the lithium disilicate specimens and composite resin as compared with 5% hydrofluoric acid applied for 20 seconds. Similarly, high concentrations of hydrofluoric acid (9%–10%) were recommended for use with feldspathic-based ceramics because those concentrations yielded higher shear bond strength values compared with lower concentrations (5%) irrespective of the treatment time[32]. Veneering ceramic chipping is reported to be the most common technical complication with PFM crowns, with incidence rate of 2.6% at 5 years[3]. Although framework fracture is not a common complication with high strength ceramics such as zirconia[3], one zirconia crown failed in this study by fracture (Fig. 4B). The fracture was related to the occlusal access cavity and extended mesiodistally, although no crack was evident at the time of root canal therapy under dental operating microscope. Several authors reported that accessed repaired zirconia crowns had a significantly lower load to failure compared with control non-accessed crowns; furthermore, all accessed crowns exhibited edge chipping around the access opening, and some showed radial crack[33]. We assume that this zirconia crown failed by crack propagation and because of access cavity preparation; therefore, patients should be well-informed that accessed and repaired ceramic crowns are at risk for future fracture due to crack propagation and might require future replacement. However, FCR replacement did not affect the quality of the coronal seal and the endodontic healing progress in this study.
Because patients were treated in a referral-based endodontic office, the type of zirconia whether monolithic or bilayered and cementation material were unknown, which may have had an impact on fracture resistance and the restoration retention, respectively[34,35]. The authors acknowledge the limitation of having this case series done by a single operator, which may denote technique sensitivity. However, this also allowed use of same materials and armamentarium throughout the study. On the other hand, the results cannot be extrapolated for application in general dental practice without advanced training in endodontics and the use of microscopes. We believe this study and clinical report can establish a baseline for confidence for clinicians to trust this treatment modality. Further multicenter prospective studies with extended follow-up time are needed to concur with the favorable outcome of endodontic access through intact FCRs.
REFERENCES
Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications in fixed prosthodontics. J Prosthet Dent 2003;90:31–41.
Pjetursson BE, Sailer I, Zwahlen M, H€ammerle CH. A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years: part I—single crowns. Clin Oral Implants Res 2007;18(Suppl 3):73–85.
Sailer I, Makarov NA, Thoma DS, et al. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? a systematic review of the survival and complication rates—part I: single crowns (SCs). Dent Mater 2015;31:603–23.
Whitworth JM, Walls AWG, Wassell RW. Crowns and extra-coronal restorations: endodontic considerations—the pulp, the root-treated tooth and the crown. Br Dent J 2002;192:315–27.
Bergenholtz G, Nyman S. Endodontic complications following periodontal and prosthetic treatment of patients with advanced periodontal disease. J Periodontol 1984;55:63–8.
Yavorek A, Bhagavatula P, Patel K, et al. The incidence of root canal therapy after full-coverage restorations: a 10-year retrospective study. J Endod 2020;46:605–10.
Trope M, Bergenholtz G. Microbiological basis for endodontic treatment: can a maximal outcome be achieved in one visit?—endodontics: a microbial issue. Endod Topics 2002;1:40–53.
Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germfree and conventional laboratory rats. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1965;20:340–9.
Zhang MM, Fang GF, Chen XT, Liang YH. Four-year outcome of nonsurgical root canal retreatment using cone-beam computed tomography: a prospective cohort study. J Endod 2021;47:382–90.
Brezinsky S, Bowles W, McClanahan S, et al. In vitro comparison of porcelain fused to metal crown retention after endodontic access and subsequent restoration: composite, amalgam, amalgam with composite veneer, and fiber post with composite. J Endod 2020;46:1766–70.
Scioscia A, Helfers A, Soliman S, et al. Performance of monolithic and veneered zirconia crowns after endodontic treatment and different repair strategies. Oper Dent 2018;43:170–9.
Van Nieuwenhuysen J-P, Aouar M, D’Hoore W. Retreatment or radiographic monitoring in endodontics. Int Endod J 1994;27:75–81.
Sjogren U, H € €agglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod 1990;16:498–504.
Kerekes K. Radiographic assessment of an endodontic treatment method. J Endod 1978;4:210–3.
Tronstad L, Asbjørnsen K, Døving L, et al. Influence of coronal restorations on the periapical health of endodontically treated teeth. Dent Traumatol 2000;16:218–21.
Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 1995;28:12–8.
Fu M, Zhang Z, Hou B. Removal of broken files from root canals by using ultrasonic techniques combined with dental microscope: a retrospective analysis of treatment outcome. J Endod 2011;37:619–22.
Peters MC, McLean ME. Minimally invasive operative care: I—minimal intervention and concepts for minimally invasive cavity preparations. J Adhes Dent 2001;3:7–16.
Peters MC, McLean ME. Minimally invasive operative care: II—contemporary techniques and materials: an overview. J Adhes Dent 2001;3:17–31.
Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod 2014;40:910–6.
Wood KC, Berzins DW, Luo Q, et al. Resistance to fracture of two all-ceramic crown materials following endodontic access. J Prosthet Dent 2006;95:33–41.
Qeblawi D, Hill T, Chlosta K. The effect of endodontic access preparation on the failure load of lithium disilicate glass-ceramic restorations. J Prosthet Dent 2011;106:328–36.
Bompolaki D, Kontogiorgos E, Wilson JB, Nagy WW. Fracture resistance of lithium disilicate restorations after endodontic access preparation: an in vitro study. J Prosthet Dent 2015;114:580–6.
Gorman CM, Ray NJ, Burke FM. The effect of endodontic access on all-ceramic crowns: a systematic review of in vitro studies. J Dent 2016;53:22–9.
Mallya J, DuVall N, Brewster J, Roberts H. Endodontic access effect on full contour zirconia and lithium disilicate failure resistance. Oper Dent 2020;45:276–85.
Nejat AH, Dupree P, Kee E, et al. Effect of endodontic access preparation on fracture load of translucent versus conventional zirconia crowns with varying occlusal thicknesses. J Prosthodont 2021;30:1–5.
The American Association of Endodontists Communique. AAE and Foundation approve definition of endodontic outcomes, volume XXIX; August/September 2005. page 3.
Fayad MI, Nair M, Levin MD, et al. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics. Oral Surg Oral Med Oral Pathol Oral Radiol 2015;120:508–12.
Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod 2004;30:846–50.
Heling I, Gorfil C, Slutzky H, et al. Endodontic failure caused by inadequate restorative procedures: review and treatment recommendations. J Prosth Dent 2002;87:674–8.
Levartovsky S, Bohbot H, Shem-Tov K, et al. Effect of different surface treatments of lithium disilicate on the adhesive properties of resin cements. Materials 2021;14.
Moura DMD, Araujo AMM, Souza KB, et al. Hydrofluoric acid concentration, time and use of phosphoric acid on the bond strength of feldspathic ceramics. Braz Oral Res 2020;34:e018.
Lohbauer U, Belli R, Arnetzl G, et al. Fracture of a veneered-ZrO2 dental prosthesis from an inner thermal crack. Case Stud Eng Fail Anal 2014;2:100–6.
ZhangY, Lee JJW, Srikanth R, Lawn BR. Edge chipping and flexural resistance of monolithic ceramics. Dent Mater J 2013;29:1201–8.
Piwowarczyk A, Lauer HC, Sorensen JA. The shear bond strength between luting cements and zirconia ceramics after two pre-treatments. Oper Dent 2005;30:382–3.

Article
OHI-S
23 April 2024

Article
OHI-S
25 April 2024
Video
OHI-S
11 January 2024


