Osseointegration and factors influencing it
Machine translation
Original article is written in RU language (link to read it).
Osseointegration is the connection of an implant with bone tissue structures due to the formation of bone substance on the metal surface without an intermediate layer of connective tissue.
Learn more about dental implantation in the online course Implantation in the aesthetic zone: stages and techniques .
Osseointegration normally undergoes three stages:
Stage I
During the first few days after installation, a primary matrix is formed on the surface of the implant. The stages of its formation can be distinguished as follows:
loss of fibrin threads, proteoglycans, attachment of mononuclear cells to the surface of the implant, their transformation into macrophages; adhesion of stem cells, some of which are transformed into fibroblasts; the production of collagen of the second and third types is launched;
fibrillization of the primary matrix, gradual differentiation, compaction; formation of a bone or cement-like substrate is observed; this process continues in the second stage.
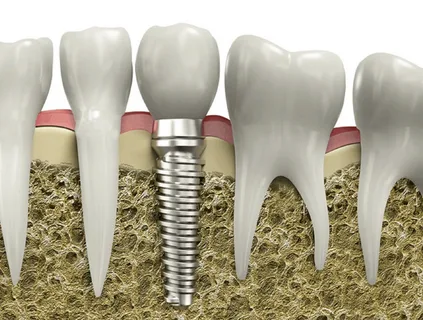
Figure 1. Osseointegration of the implant.
Stage II
Bone-forming cells differentiate at the periphery of the primary matrix under the influence of growth factors that penetrate from the maternal bone as a result of its resorption. Type I collagen is actively synthesized, and foci of fibrous bone substrate are formed. The peri-implantation zone of the implant bed is subject to resorption under the action of osteoclasts. Substances that are required for the construction of bone tissue accumulate. They attach to the surface of the implant, where, together with active cellular structures, they participate in the construction of the bone matrix.
Stage III
Remodeling, or secondary restructuring. Its onset coincides with the beginning of the creation of an osteoid matrix on the surface of the implant (1-2 weeks from the moment of implantation) and is accompanied by the formation of young trabecular bone tissue. Secondary restructuring lasts for a year or more, during which imperfect bone tissue is replaced by mature bone structures.
Factors affecting osseointegration can be divided into local and general.
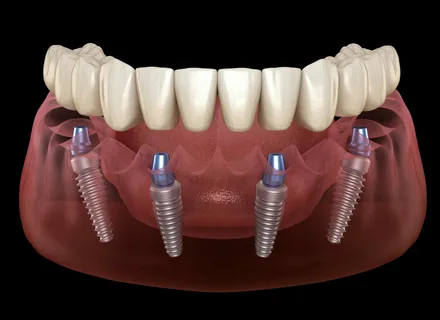
Figure 2. Prosthetics on dental implants.
Local ones include the following:
Material.
Surface structure.
Heating the bone.
Contamination, pollution.
Primary stability.
Bone condition.
Ingrowth of mucosal epithelium.
Increased load.
Material
The effectiveness of osseointegration is determined by the type of material from which the implant is made. High-quality titanium is the basis of dental implant technology. But there are other materials that can form a strong bond with bone tissue: zirconium, certain types of ceramics.
Surface structure
Osseointegration of titanium is due to the ability of this metal to rapidly form a persistent inert oxide coating on its surface. This coating promotes the construction of bone tissue and is osteoconductive. The ability for osseointegration is also characteristic of materials such as gold, zirconium, glassy carbon, and ceramics. The initial bond between the bone matrix and the implant surface is determined more actively than around an implant made of titanium.
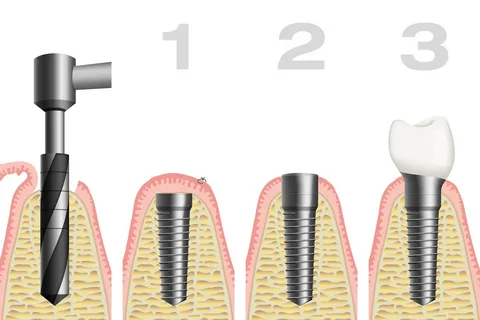
Figure 3. Stages of dental implantation.
Overheating
A local increase in bone temperature of more than 47°C during surgery causes collagen denaturation and cell lysis. As a result, instead of osseointegration, a fibrous capsule is formed around the implant, which significantly reduces the strength of the connection with the bone. It is very important to avoid overheating the bone during bone bed preparation. The following factors influence overheating:
tool rotation speed,
tool shape,
thickness of bone tissue cut at once,
bone density,
cooling.
The ideal option is to use low-speed tools with good cooling.
Pollution, contamination
Contamination of the bone bed with organic and inorganic fragments can create an obstacle to osseointegration. The greatest danger comes from necrotic fragments, chemicals, bacterial agents, and drill microparticles. To prevent contamination of the peri-implantation zone, it is important to use modern equipment (titanium instruments), and the implant surgeon must strictly follow the surgical protocol.
Primary stability
This concept assumes a tight position of the implant inside the bone bed. Primary stability is determined by the accuracy of implant insertion, its configuration, structure and bone density. By giving preference to screw implants, it is easier to achieve stability than when working with implants that do not have a pronounced relief.
The bone bed, represented by a loose, coarse bone structure, is not able to guarantee primary stability. To solve this problem, manufacturers offer self-tapping implants.

Figure 4. Dental implant.
Bone quality
The qualitative characteristics of the bone also influence osseointegration; its density, morphological structure, and volume are taken into account. The qualitative characteristics of bone are determined by the density and percentage of the cortical plate to the cancellous substance. Osseointegration is not directly affected by bone thickness, but is an important criterion when placing an implant. If the volume is insufficient, there is a high risk of functional overload and an unfavorable treatment outcome. Given this indicator, it is important to choose the correct implant size.
Epithelial sprouting
The first implants were characterized by design flaws that allowed mucosal epithelium to grow along the root surface of the implant. To prevent epithelial growth when installing next-generation implants made of pure titanium, the implant was covered with a mucous flap during the period of osseointegration. After the process is completed, the implant is opened, the superstructure is installed, and the integrated surface is resistant to epithelial ingrowth. Other methods of using implants involve penetration of the mucosa immediately at the time of implant installation. During this technique, the superstructure is installed on the implant immediately after its placement in the bone tissue.
Load
Premature loading in the early stages of implantation negatively affects osseointegration. If the implant is subjected to high loads, osseointegration will not occur and a fibrous capsule will form around the implant. Overloading the implant in the later stages, after the onset of osseointegration, will lead to destruction of osseointegration and implant rejection. Moderate loads do not affect the osseointegration process. Reasons for significant loads: bad habits, bruxism, structural features of the superstructure.
General factors influencing the process of osseointegration
Floor.
Age.
Chronic diseases.
Nutritional features.
Bad habits.
Floor
Sex hormones are of great importance here. Estrogens increase the activity of osteoblasts and increase the rate of mineralization of the primary matrix. Androgens have a general anabolic effect on the body, slow down bone resorption, and accelerate mineralization.
Age
The bone structure in the area of damage can fully recover only in childhood. This is due to a decrease in the intensity of reparative processes with age. Osseointegration slows with age and natural bone loss occurs.

Figure 5. Prosthetics after completion of osseointegration.
Chronic diseases
The presence of somatic pathology has a significant impact on osseointegration.
Hypo- or hyperfunction of some hormones causes disruption of the mechanisms of reparative osteogenesis.
Diabetes mellitus is characterized by osteoporosis and slower bone remodeling. Lack of insulin inhibits the synthesis and mineralization of bone tissue.
Cholelithiasis is characterized by osteopenia and vitamin D deficiency.
Chronic liver diseases are associated with pathologies of mineral metabolism, hypocalcemia, hypomagnesemia and hypercalciuria.
In chronic ulcerative colitis and Crohn's disease, bone mineral density decreases.
Renal failure is accompanied by pathology of calcium-phosphorus metabolism.
Bad habits
Dental implantation is contraindicated if the patient has bad habits: alcoholism, smoking, drug use.
Long-term smoking is characterized by weakening of the local immunity of the oral cavity, poor hygiene, and impaired microcirculation.
In those suffering from alcoholism, bone tissue pathology is associated with disorders of mineral metabolism. Ethanol negatively affects the activity of most endocrine glands.
How to avoid complications of dental implantation in the online course Implantation without peri-implantitis .


