Non-odontogenic non-osteogenic tumors of the jaws
Machine translation
Original article is written in RU language (link to read it).
Non-odontogenic non-osteogenic tumors of the jaws are neoplasms, the source of which is not bone tissue or other odontogenic structures. These tumors are formed from other tissues: connective, nervous and others.
More up-to-date information on maxillofacial surgery is available in the section of our website called Maxillofacial Surgery Training .
Representatives of these neoplasms:
neurofibroma, fibroma,
neurolemmoma,
myxoma,
hemangioma,
hemangioendothelioma.
Treatment of such tumors is labor-intensive and involves a combined approach consisting of surgery, chemotherapy and radiation therapy. Often, diagnosis and further treatment planning are carried out by several specialists at once: maxillofacial surgeons, neurosurgeons, ophthalmologists, otorhinolaryngologists.

Figure 1. The course of non-osteogenic neoplasms is often asymptomatic.
Fibroma
Fibroma is a non-osteogenic neoplasm that is diagnosed extremely rarely among patients. This intraosseous tumor accounts for only about 2% of all primary neoplasms of the jaws.
Due to the fact that intraosseous fibroma of the jaw is not a common disease, it has been studied very little.
Histologically, fibroma is represented by connective tissue structures that do not produce bone substance. True intraosseous fibroma does not contain osteoblasts, but petrification may be observed in it.
Petrification is a simple calcification when tumor tissue undergoes diffuse precipitation of calcium salts. It is important to consider that petrification is not capable of causing the transformation of calcified tissue into bone. Intraosseous fibroma, based on morphological characteristics, can be classified as true if its structure corresponds to the structure of fibroma formed outside the skeleton.
Clinical picture
Fibroma of the jaws has no specific clinical manifestations. The tumor is characterized by slow growth, asymptomatic course, and both jaws are affected with equal frequency. Considering the described signs, it becomes clear that until the fibroma reaches a large size, it can only be detected by chance during an X-ray examination of the jaw.
As it grows and reaches an impressive size, the tumor gradually begins to cause deformation of the jaw, which is often accompanied by speech disorders and difficulties in eating.
In some patients, an increase in the size of fibroids is accompanied by the appearance of aching pain, which forces them to see a doctor. The period from the moment the first signs of a tumor appear to a visit to the doctor can range from 1-2 months to several years.

Figure 2. External manifestations of the tumor process.
The addition of a secondary infection is an extremely rare occurrence for fibroids. The tumor, gradually growing beyond the jaw, rises under the unchanged mucous membrane or skin. Typical clinical symptoms:
hemispherical formation,
tightly fused to bone tissue,
has a smooth surface,
clear boundaries
dense consistency upon palpation,
painless,
If the tumor is located within the alveolar process, tooth displacement may occur.
X-ray diagnostics
Fibroma with a central location is characterized by the following radiological signs:
the main pathological focus of the bone lesion has a rounded outline or an ellipse shape,
the boundaries are clear;
the appearance of the lesion is homogeneous, without characteristic structures,
the lesion is surrounded by thinned bone,
no reaction is observed from the periosteum,
the central part of the lesion may include small dense shadows corresponding to areas of calcification.
Jaw fibroids in most cases do not have a typical x-ray picture.

Figure 3. X-ray diagnostics is an important stage in making a diagnosis.
The final diagnosis is made on the basis of clinical symptoms, X-ray data and, necessarily, histological examination.
Histological characteristics of jaw fibroma
Histologically, it is customary to distinguish the following morphological types of fibromas:
simple fibroma, characterized by the presence of fibrous coarse fibrous connective tissue, which includes moderate inclusions of cellular elements;
petrifying fibroma, this type is characterized by the presence of small foci of calcification with calcium salts;
odontogenic fibroma, which is characterized by the content of fragments of tooth-forming epithelium.
The connective tissue mass of the tumor contains only small areas of the epithelial component, which may take the form of rare small islands, or may be represented by isolated strands of round cells. Such remnants of the epithelial component are the main evidence of the odontogenic origin of this type of fibroma.
Differential diagnosis
A prerequisite for correct diagnosis is differential diagnosis of jaw fibroma with the following neoplasms:
sarcoma, especially among pediatric patients,
osteoblastoclastoma,
adamantinoma,
fibrous dysplasia.
Treatment
The main treatment method for true intraosseous fibroma of the jaw is surgery aimed at removing the tumor within healthy tissue.
If a patient is diagnosed with ossifying fibroma, the following technique is recommended: subperiosteal resection of the jaw and simultaneous bone grafting.
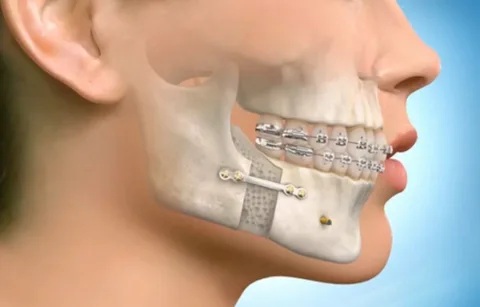
Figure 4. Bone grafting is required after tumor removal.
In the case of fibroma, the tactics of surgical intervention may be limited only to enucleation of the tumor, but if the patient has a mixed tumor - fibromyxoma, it is important to take into account the fact that myxomatous tissue can grow into the surrounding bone structure, therefore such a tumor is excised, retreating at least 5 mm from the visible borders .
Tumor recurrence does not occur after radical surgery. Fibroids are not characterized by malignancy. The effectiveness of radiation therapy for fibroids has not been proven.
Myxoma
Intraosseous myxoma of the jaw is a fairly rare disease, which accounts for about 1% of the primary formations of the bones of the facial skeleton.
Most common tumor location:
lateral areas of both jaws,
the upper jaw is most often affected,
in the upper jaw, the distal parts of the alveolar process are mainly affected, less often the tumor spreads to the entire bone and maxillary sinus,
in the area of the lower jaw, the tumor is more often detected in the distal parts of the body; the branch of the jaw is affected extremely rarely.
Myxoma can be observed among both children and adult patients, equally often among patients of both sexes. True intraosseous myxoma, in its pure form, is rare, occurring only in the lower jaw.
Pathogenesis
Myxomas develop from mucous tissue that includes mucin and Wharton's jelly of the umbilical cord.
It is customary to distinguish the following types of mix:
primary,
secondary.
Secondary is a consequence of mucous degeneration of fibroids, sarcomas, lipomas, sarcomas and other tumors, hence such varieties as:
myxoma,
myxofibroma,
myxolipoma,
myxosarcoma,
myxochondroma.
Clinical picture
Myxoma has a dense, smooth surface.
On palpation the tumor is painless.
Differs in slow growth.
Can reach significant sizes.
Palpation is a dense, smooth, painless node, which is covered on top with unchanged mucosa.
May be accompanied by mobility and displacement of teeth.
When the tumor is localized in the lower jaw and the neurovascular bundle is damaged, the appearance of Vincent's symptom is characteristic.
When the tumor is localized in the upper jaw, the latter often spreads to the nasal cavity and maxillary sinus.
Macroscopic characteristics
An elastic formation of a round shape, represented by a single node.
There is no membrane, so it is impossible to clearly determine the boundary between the tumor and surrounding tissues.
The section reveals a translucent gelatinous mass containing a large number of small cysts, which are filled with mucous fluid mixed with blood.
Microscopic characteristics
It is represented by stellate spindle-shaped cells with anastomosing processes located in a translucent ground substance, which contains mucin and a large number of blood vessels, argyrophilic and collagen fibers.
The tumor does not have a capsule.
There is infiltrating growth of the tumor along connective tissue areas, along large vessels far beyond the boundaries of the tumor node.

Figure 5. Histological examination is mandatory to identify the type of tumor.
X-ray picture
The shape of the focus of destruction is oval or round.
The location is eccentric or central.
A bay-shaped protrusion of the bone, the cortical layer is very thin.
The boundaries are unclear.
Along with destruction, there are bone beams of different shapes and sizes.
Treatment
This tumor is treated exclusively by surgery. Taking into account the polymorphism of cells and the tendency to infiltrating growth, preference should be given to radical excision of the myxoma during subperiosteal resection of the jaw and performing one-stage bone grafting.
After surgery, recurrence is not typical.
Always useful and up-to-date information on various sections of dentistry is presented on our website .


