Manifestations of mycoses in the oral cavity. Candidal stomatitis
Machine translation
Original article is written in RU language (link to read it).
Candidal or fungal stomatitis is an inflammatory disease of the oral mucosa, which is caused by fungi of the genus Candida. The latter are representatives of opportunistic microorganisms. This pathology is most often diagnosed in children of primary school age, as well as among elderly patients.
There is even more useful information on diseases of the oral mucosa in the Periodontology Training section of our website.
Factors contributing to the appearance of candidal stomatitis
- metabolic disorders,
- diseases of the endocrine system, including diabetes mellitus,
- long-term use of antibiotics,
- hypovitaminosis,
- pregnancy,
- use of oral contraceptives,
- bad habits.
The most common symptoms of fungal stomatitis in the oral cavity are as follows:
- whitish cheesy coating,
- erosive surface, sometimes ulcers that appear when trying to remove plaque,
- swelling of the affected mucous membranes,
- discomfort, pain while eating,
- loss of appetite,
- digestive disorders, especially in the case of generalization of the process and involvement of other parts of the gastrointestinal tract in the pathological process,
- burning in the mouth,
- a yellowish film may be detected on the tongue and mucous membranes of other parts of the oral cavity,
- metallic taste, loss of taste sensitivity,
- pain when swallowing.

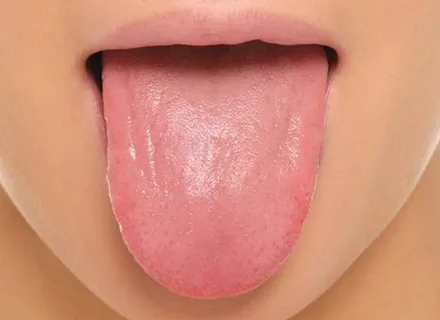
Rice. 1. Healthy mucous membrane of the tongue.
Etiology of the disease
Candidal stomatitis is a pathology associated with a violation of the number of yeast-like fungi Candida, is isolated, local in nature, or is associated with damage to the mucous membranes of other parts. In the case of the addition of factors such as cellular immunodeficiency, or with late diagnosis or untimely treatment, candidiasis can acquire a generalized course associated with damage to internal organs; the prognosis of such a pathology will be extremely unfavorable.
Clinical manifestations
Symptoms of candidiasis are very diverse and are determined by the patient’s age, immunological status, and the presence of chronic pathology that requires constant use of medications.
The form of candidal stomatitis can be acute or chronic.
The acute form of fungal stomatitis is in turn divided into acute pseudomembranous and acute atrophic candidiasis.
Chronic candidiasis can be represented by the following clinical forms: hyperplastic and atrophic.
Acute pseudomembranous form
Acute pseudomembranous candidal stomatitis is the most common form of this pathological condition. Children of primary school age, who are characterized by this disease, suffer from this particular form, for them it is relatively easy, recovery occurs quickly with timely treatment, without complications.
Among adult patients, candidal stomatitis can also occur in an acute pseudomembranous form; its appearance is usually associated with severe general somatic pathology: hypovitaminosis, diabetes mellitus, blood diseases, malignant tumors.
Patients complain of a burning sensation in the oral cavity, the addition of plaque, and soreness of the mucous membrane during meals, especially acute ones. Pathological changes are most often observed on the mucous membrane of the following localizations: the back of the tongue, lips, cheeks, palate.

Rice. 2. Fungi of the genus Candida.
Clinical symptoms
In place of the hyperemic mucosa, a whitish coating appears, which in appearance resembles cottage cheese or curdled milk. Characteristically, plaque rises above the surrounding intact mucosa; at the initial stage of the disease, plaque is easily removed by scraping with a spatula to expose a smooth, moderately swollen and reddened surface. In case of prolonged absence of treatment and neglect of the disease, the plaque thickens significantly, and it is almost impossible to remove it by scraping.
Acute atrophic form
For the acute atrophic form of fungal stomatitis, typical symptoms are: burning and soreness of the oral mucosa, additional dryness. An external examination reveals dry, fiery red mucous membrane. If the pathological process is localized on the surface of the tongue, the back acquires a crimson-red color, becomes shiny and dry, and atrophy of the filiform papillae is characteristic.
Rice. 3. Atrophy of filiform papillae.
Plaque in most cases is not detectable, can rarely be present in deep folds, is difficult to remove, and is a conglomerate of exfoliated epithelium and actively budding colonies of fungi of the genus Candida. Acute forms of candidal stomatitis are not characterized by a disturbance in the patient’s general condition, there is no enlargement of the lymph nodes, and the body temperature does not rise.
Clinical manifestations of chronic forms of candidal stomatitis
Hyperplastic form
The patient's complaints with the hyperplastic form of stomatitis are as follows: the appearance of dryness and burning in the oral cavity, the addition of pain against the background of erosion.
Clinical symptoms
- Against the background of hyperemic mucosa, thickened plaque accumulations in the form of plaques or nodules are formed, tightly attached to the affected surface.
- Foci of plaque are located on an uneven underlying surface and are tightly welded to it.
- Typical localization of plaque is the palate and the dorsal surface of the tongue.
- On the back of the tongue, pathological changes resemble those with rhomboid glossitis.
- In the case of localization on the mucous membrane of the hard palate, the hyperplastic form of chronic candidiasis externally resembles papillary hyperplasia.
- In the absence of proper treatment for a long time, the foci of plaque are impregnated with fibrin, films are formed that have a yellow-gray color, which are tightly fused to the affected surface of the mucous membrane.
- Scraping with a spatula allows only partial removal of plaque, under which an erosive surface is exposed, bleeding and hyperemic.
Atrophic form
In most cases, the atrophic form of chronic candidiasis is observed in elderly people who have been using removable lamellar dentures for a long time. With this pathological condition, patients note dry mucous membranes, a burning sensation in the oral cavity, and pain when using a removable denture. The mucous membrane, located within the boundaries corresponding to the prosthetic bed, becomes swollen, hyperemic, and painful.

Rice. 4. Budding of fungi of the genus Candida.
In patients who wear removable dentures for a long time, damage to the mucous membrane of the prosthetic bed in the form of papillomatosis, erosion or hyperemia, the addition of mycotic seizure and atrophic candidal glossitis is typical, when the dorsal surface of the tongue acquires a crimson-red color, becomes shiny and dry, and atrophy of the filiform papillae is observed. Inflammatory lesions of the corners of the mouth, tongue and palate are characteristic of the atrophic form of fungal stomatitis.
Yeast or mycotic seizure occurs mainly among elderly patients who have a decrease in the height of the bite as a result of irrational prosthetics, adentia, and increased abrasion of hard dental tissues. The formation of deep folds in the corners of the mouth and maceration of these areas with saliva provide favorable conditions for mycotic infection.
The patient's complaints may be the following: burning and pain in the corners of the mouth. Clinically characterized by the formation in the corners of the mouth of tender crusts, transparent or gray scales, plaque, which is easily removed, revealing weeping or dry cracks or erosions.
Gradually, the pathological process spreads from the corners of the mouth to the red border of the lips, which is accompanied by the appearance of candidal cheilitis.
Clinical manifestations of candidal cheilitis
- Hyperemia and swelling of the red border.
- Grayish scales on the surface of the lips.
- Small transverse cracks on the red border.
- Stretching the lips causes pain.
Diagnostics
The diagnosis is based on the patient's complaints, clinical examination, and also on laboratory tests (taking a smear from the oral cavity and its subsequent microbiological examination). It is also recommended to conduct a general blood test and determine blood glucose levels. To exclude generalization of the pathological process and the development of complications, consultations with the following specialists are necessary: endocrinologist, mycologist, gynecologist.

Rice. 5. White coating on the tongue.
At the initial stage of treatment, the dentist is required to undergo mandatory sanitation of the oral cavity, since periodontal pockets and carious cavities are favorable areas for the budding of Candida fungi.
If you liked this article and want to keep up to date with current information on various sections of dentistry, you can always find it on our website .


