Kinesiographic recordings of jaw movements are not accurate to detect magnetic resonance–diagnosed temporomandibular joint (TMJ) effusion and disk displacement: findings from a validation study
Objective. The aim of this study was to perform a validation study assessing the correlation between magnetic resonance (MR) findings of temporomandibular joint (TMJ) disk displacement and effusion and some parameters drawn from kinesiographic (KG) recordings of jaw motion, i.e., deflection, deviations, incisures.
Study Design. Thirty-one patients with TMJ disorders underwent a kinesiographic recording in the same day in which the MR was performed. Regression analysis was performed to assess the correlation between the MR and KG findings.
Results. MR findings were not correlated with KG parameters (P .05). The accuracy of all KG variables for diagnosing MR-detected signs was low. KG deflection ranged from 38.7% to 54.8%, KG deviation from 42% to 54.8%, and KG incisures from 9.6% to 71%. Specificity and positive predictive values were far from acceptable levels for all KG variables.
Conclusions. The findings do not support the usefulness of jaw-tracking devices in dental practices that diagnose and manage temporomandibular disorders. (Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:457-463)
Further details about diagnostic functional protocols in dentistry for you to learn in our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
INTRODUCING
In the field of temporomandibular disorders (TMD), a clinical assessment of signs and symptoms is considered to be the gold standard for diagnostic work-up of new patients. Therefore, the main internationally recognized diagnostic and classification guidelines are based on clinical evaluations of the jaw muscles and the temporomandibular joints (TMJs). Beyond that, imaging-based approaches may be needed to more thoroughly assess these disorders in selected cases involving structural problems or pathologies of the TMJ.
Among these, magnetic resonance (MR) has become the standard of reference for the assessment of soft tissues, because it can depict TMJ disk position and the presence of joint effusion.6 In recent years, however, the indications for TMJ imaging of these phenomena has decreased owing to the emerging evidence that the natural course of most TMJ disk derangements is benign in nature. As a result, the accurate depiction of disk position abnormalities is now less important for treatment planning than thought in the past. In view of this consideration, a thorough clinical assessment is often enough for managing the majority of TMD patients.
On the other hand, there are some clinicians who argue for using more technologic devices in the diagnosis of TMDs. In the clinical setting, instruments for making electromyographic (EMG) and kinesiographic (KG) recordings have been proposed as diagnostic aids for TMJ and jaw muscle disorders on the basis of their claimed usefulness to detect dysfunctions of the stomatognathic system. In using such instruments, the ultimate TMD diagnosis is based on abnormal EMG activity of the jaw muscles or peculiar features of jaw movements. However, recent studies have questioned the validity and reliability of those diagnostic instruments. Also, recent investigations using more sophisticated research instruments in an experimental setting have brought new insights into the assessment of jaw function and muscle activity, but clinicians may find it difficult to draw clinically useful information from studies using devices designed for research purposes. The most suitable strategy to avoid confusion and to ease the science transfer process is to perform investigations based on the use on commercially available devices, to obtain findings that can be easily interpreted for their impact in everyday clinical practice.
Also, it must be noted that parameters for physiology with the use of those instruments were not based on validation studies, and are drawn from the opinions of the users.
With this premise, and with the aim to test the validity of surface EMG and KG in the clinical practice, a series of investigations has been performed recently on TMD patients showing, among other things, that surface EMG recordings have a poor diagnostic accuracy for myofascial pain16 and that KG recordings can not be relied on to monitor the course of disease symptoms after treatment (Manfredini et al, personal communication, 2012).
However, studies have not been reported previously about the accuracy of KG recordings to detect TMDs such as various forms of disk displacements and/or joint effusions. To this aim, MR has to be assumed to be the standard of reference for visualizing those signs and trying to correlate them with either clinical or other instrumental findings.
Considering these premises, the aim of the present investigation was to assess the correlation between MR findings of TMJ disk displacement and effusion and some parameters drawn from kinesiographic recordings of jaw motion. The null hypothesis was that no correlation exists between MR and KG signs. Also, the accuracy, sensitivity, specificity and predictive values of KG findings for MR signs were assessed.
Statement of Clinical Relevance
This investigation evaluated the usefulness of a commercially available device purported to diagnose temporomandibular disorders. In this small study population, the findings from kinesiographic recordings of jaw motion did not accurately correlate with the findings from magnetic resonance imaging.
MATERIALS AND METHODS
Study population
The study population was composed of 31 patients (87% female; overall mean age 43.1 years) seeking treatment at the TMD Clinic, Department of Maxillofacial Surgery, University of Padova. Participants were selected among those subjects for whom the need to undergo magnetic resonance was clinically established in the attempt to get deeper into the assessment of internal derangements and/or differential diagnosis with other muscle or joint disorders. The patients who gave their consent to take part in the study underwent a KG recording in the same day in which the MR imaging was performed. Exclusion criteria were the presence of systemic diseases affecting joint and/or masticatory muscles, such as fibromyalgia or other rheumatic diseases diagnosed according to the American College of Rheumatology criteria. All patients were informed about the study’s aims and procedures and agreed to participate. Approval from the local ethical committee was obtained based on the noninvasive nature of the investigation.
Magnetic resonance
MR was carried out with a 1.5 Tesla (GE Signa Contour; GE Medical Systems, Buc, France) with a bilateral circular (8 cm diameter) surface coil for both right and left TMJs. The investigation protocol provided for a first axial scan “scout” from which were established 7 sagittal-oblique slices in lateral- medial direction and coronal sections deviated obliquely in posteroanterior direction. Sequential gradient-echo T1 (TR 340 ms, TE 16 ms, FOV 15 cm, slice thickness 3 mm, matrix 256 - 192, inter-slice gap 0.5 mm) and fast-stir T2-weighted (TR 3,500 ms, TE 27 ms, FOV 15 cm, slice thickness 3.5 mm, matrix 256 - 160, interslice gap 0.5 mm) were made with the subjects in both closed-mouth and maximum-open-mouth positions. The latter position was obtained by means of a wooden intermaxillary device at the same opening as measured clinically.
The articular disk was directly identified in sagittal oblique T1-weighted images as an area of hypointensity with a biconcave shape above the condylar structure, and its position was categorized according to literature data:
Superior (normal) disk position (N): posterior band of articular disk located above the apex of the condylar head (at 12 o’clock position) in both closed-mouth and maximum-open-mouth positions.
Disk displacement with reduction (DDR): posterior band of the disk located anteriorly to the condylar head in closed-mouth position, but normal disk-condyle relationship established in maximum open-mouth position.
Disk displacement without reduction (DDNR): posterior band positioned anteriorly to the condyle in both closed-mouth and maximum-open-mouth positions.
Joint effusion has been identified in T2-weighted images as a large area of high signal intensity inside the joint space, so that the presence/absence of effusion was defined as follows, in accordance with the hypothesis that mild to moderate amount of fluid can be detected in normal joints as well:
No effusion: no area or thin lines of hyperintensity.
Effusion: presence of areas of high signal intensity 2 mm of superior-inferior height or anterior-posterior length inside the articular space.
To avoid interpretation bias related to the different radiologists assessing the images, MR images were interpreted by the expert clinicians of this investigation (D.M., L.G.N.), who recorded the presence/absence of effusion and disk position abnormalities by consensus (Figures 1 and 2).
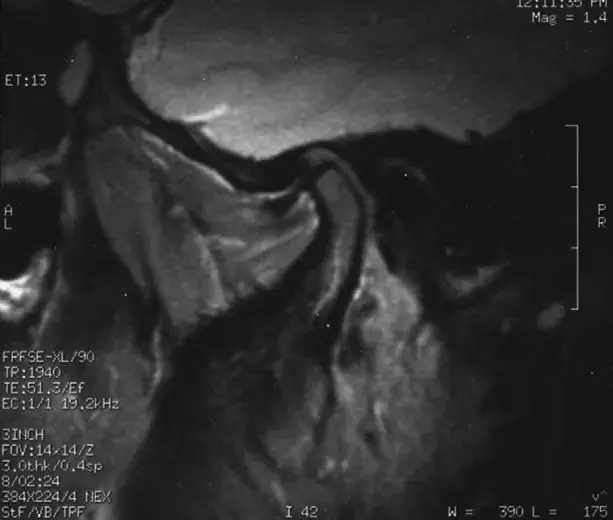 Fig. 1. Disk displacement with reduction in closed-mouth position.
Fig. 1. Disk displacement with reduction in closed-mouth position.
 Fig. 2. Disk displacement without reduction in presence of joint effusion
Fig. 2. Disk displacement without reduction in presence of joint effusion
Kinesiographic recordings
Each study participant underwent a KG recording with a commercially available device (K6 Diagnostic System, Myotronics, Seattle, WA). During all exams, which were performed with strict observance of the manufacturer’s guidelines, the patient was seated on a wooden high-backed chair, with the trunk perpendicular to the floor and the head upright, in a position achieved by asking the patient to look ahead. The kinesiographic recordings were made with the use of a magnet temporarily applied on the subject’s buccal mucosa under the lower arch central incisors to monitor the location of the mandible against a sensor array suspended in front of the face by a lightweight frame suspended on the bridge of the nose and connected behind the head by straps. All tasks were performed 3 times at 10-minute intervals and the average value of the 3 attempts was recorded. All KG assessments were made by one investigator (F.C.) with expertise in the use of such devices and with continued education training at in-house courses organized by the manufacturer. For all participants, the following parameters were recorded for statistical analysis, based on their purported relevancy as markers for disk displacement and effusion:
Maximum lateral deviation: shift from the midsagittal plane during jaw opening with subsequent realignment on the same plane.
Maximum lateral deflection: Shift from the midsagittal plane at the end of the jaw opening movement (Figure 3).
Kinesiographic incisure: sudden decrease in jaw speed during the jaw opening-closing movements (Figure 4).
For statistical purposes and comparison with MR findings, all KG parameters were dichotomized into cate goric (yes/no) variables: Deviations and deflections from the midsagittal plane were considered to be positive for values 2.5 mm, and the presence of KG incisures was considered positive when 1 variation (sudden decrease-increase effect) in speed velocity occurred during jaw opening.
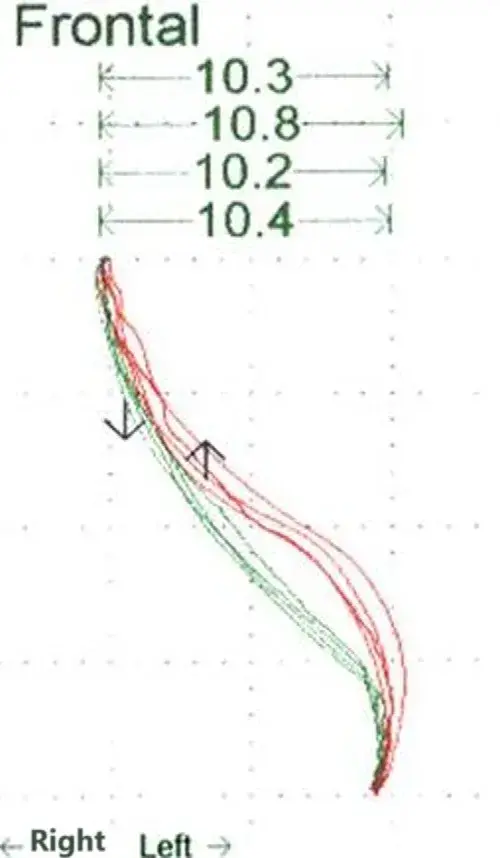 Fig. 3. Left deflection from the midsagittal plane during jaw opening.
Fig. 3. Left deflection from the midsagittal plane during jaw opening.
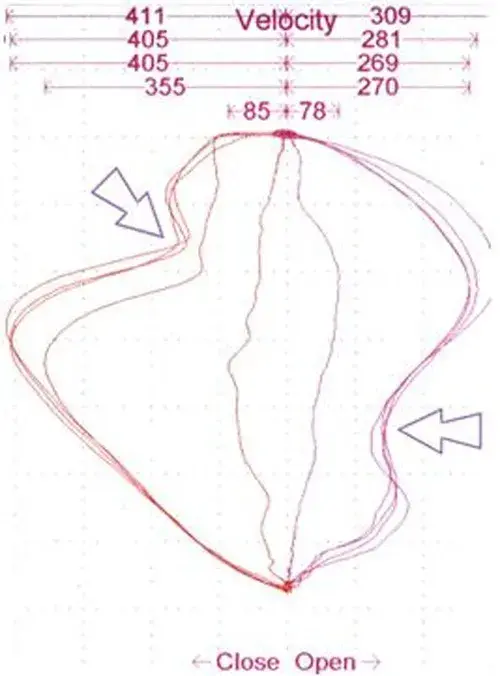 Fig. 4. Speed variations (incisures, arrows) during jaw opening/closing movements.
Fig. 4. Speed variations (incisures, arrows) during jaw opening/closing movements.
Statistical analysis
A binary single variable regression analysis was performed to assess the correlation between the MR findings (per each side: DDR, DDNR, effusion) and the KG parameters (lateral deviation, lateral deflection, incisure).
In the case that 1 KG variables showed a P value of .10 with any MR finding at the single variable regression analysis, they were managed as potential predictors of the specific MR diagnosis and entered into a multiple regression analysis as independent variable(s) to describe predictive models for MR diagnoses. In addition, the accuracy and positive/negative predictive values of KG findings to predict MR signs of disk displacement and joint effusion were assessed.
All statistical procedures were performed with the software Statistical Package for the Social Sciences 19.0 (IBM Italia, Segrate, Italy).
RESULTS
The most frequent MR diagnosis was DDR, which was shown in 35.5% and 54.8% of the right and left joints, respectively; effusion was diagnosed in 19.4% and 29.0%, respectively. DDR was shown in 67.7% of the patients, joint effusion in 41.9%, and DDNR in 6.5%. As for KG findings, 87.1% and 83.9% of patients showed 1 incisures during jaw closing and opening movements, respectively, with 96.8% of patients showing incisures during -1 movement. Deviations to -1 side were shown by 54.8% of the patients, and 45.2% showed either right or left deflection. Details of the specific distribution of the different findings per side are shown in Table I.
The presence of MR-depicted disk displacement with reduction was not correlated with any of the KG findings, with P values ranging from .062 to .999. KG findings were not found to be correlated with MR-depicted DDNR (P values ranging from .063 to .999). Also, the presence of MR-depicted joint effusion was not correlated with any of the KG findings, with P values ranging from .09 to .999 (Table II). Correlations between MR and KG findings below the P .10 level did not emerge from the single-variable regression analysis. Therefore, multiple regression analysis was not performed.
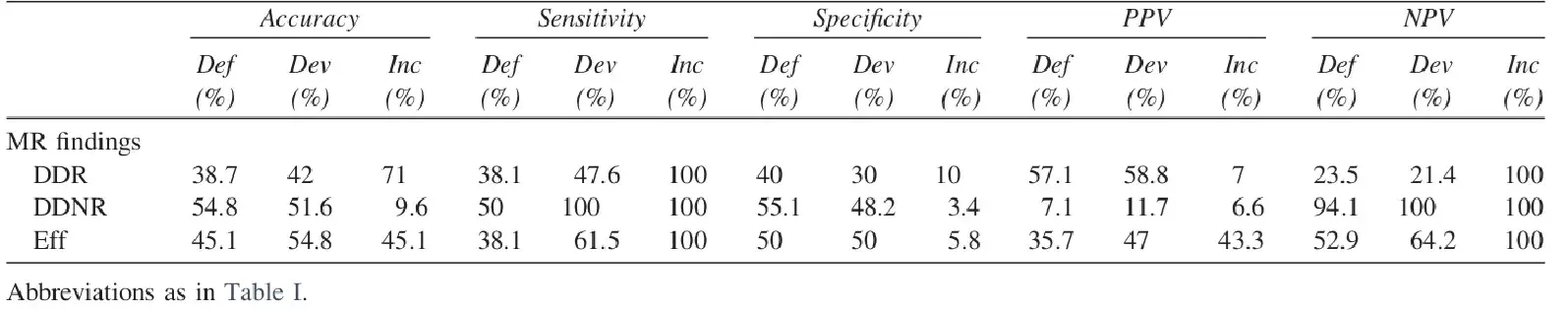
As a consequence of the poor relationship between KG and MR findings, the accuracy of the various KG findings to predict the presence of any specific MR sign at the patient level was poor. The accuracy values of KG deflection for diagnosing MR-detected signs ranged from 38.7% to 54.8%, that of KG deviation spanned from 42% to 54.8%, and that of KG incisures from 9.6% to 71%. Importantly, specificity (deflection: 40%-55.1%; deviation: 30%-50%; incisures: 3.4%-10%) and positive predictive values were far from acceptable for all the KG variables, thus suggesting that the high sensitivity (deflection: 38.1%-50%; deviation: 47.6%-100%; incisures: 100%) and negative predictive values levels described for some parameters were strongly due to the risk of overdiagnosing disease in subjects not presenting any MR signs (Table III).
Table I. Frequency of magnetic resonance and kinesiographic findings
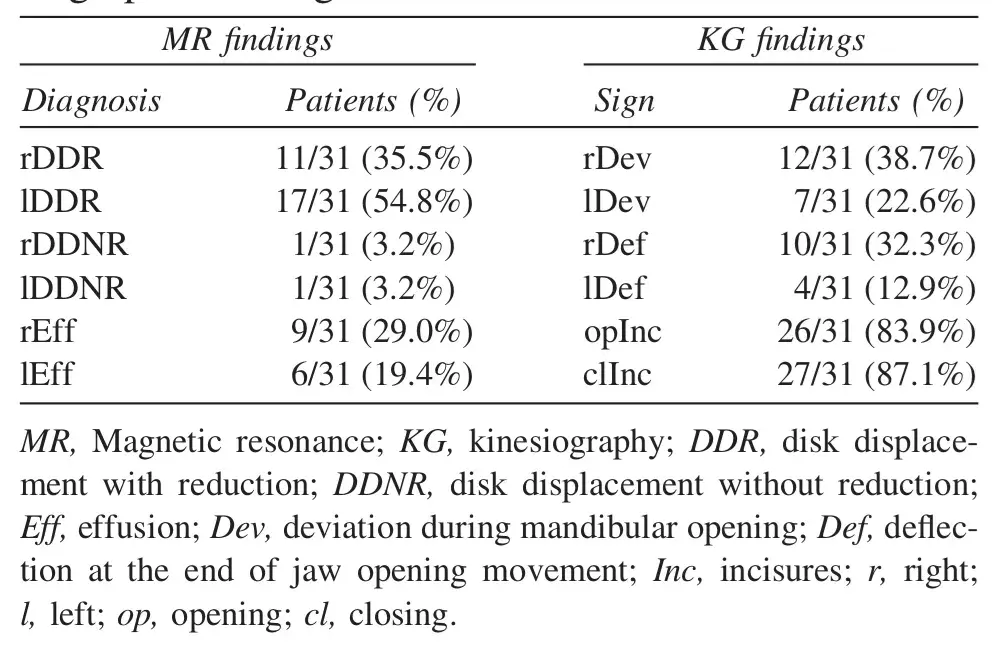
Table II. Single-variable regression analysis and P values (correlation) of the KG findings for predicting MR diagnoses
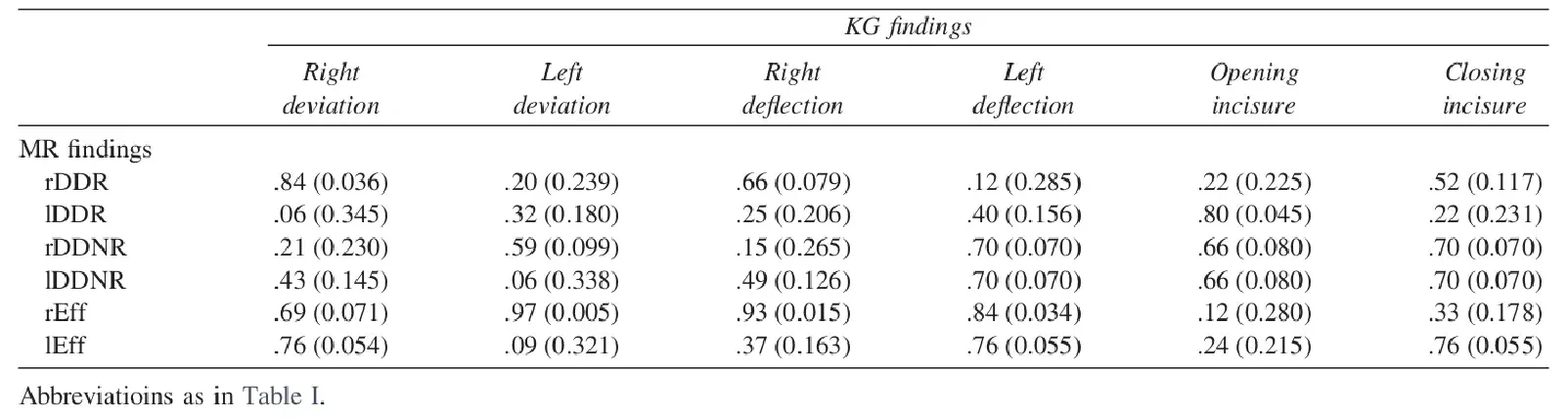
Table III. Accuracy, sensitivity, specificity, and positive (PPV) and negative (NPV) predictive values of the different KG parameters for MR findings
DISCUSSION
In the field of pain medicine, there has always been much debate on how to provide objective measurement of patients’ symptoms. TMDs are no exception, and the literature provides several examples of the debate surrounding the usefulness of instrumental devices as a diagnostic aid to integrate clinical assessment. Instruments should be reliable, i.e., have their own internal validity, and accurate, i.e., have external validity to capture findings correlated with patients’ symptoms.
Over the years, the role of imaging techniques for diagnostic purposes in TMD patients has been progressively clarified, to the point that the relationship between images and clinical symptoms as well as the indications to prescribe diagnostic deepening via imaging techniques have become clearer and clearer.
In contrast, despite cautionary statements by the research community, findings from devices adopted to measure jaw muscles with the use of EMG and KG have been accepted as valid by several clinical practitioners, without appraising their validity, based only on claims and opinions of the users of those instruments.
A possible explanation for such a contrasting approach, i.e., research setting versus clinical communities, is that several studies on the issue were performed with EMG and jaw-tracking devices designed for ad hoc research purposes and not available for the everyday practice, thus limiting the diffusion of findings. For this reason, it is worthwhile to focus efforts on the assessment of the validity of commercially available devices.
In the present investigation, KG recordings were obtained with a device used by clinical practitioners, and the correlation of the findings with those of MR imaging was assessed. MR is considered to be the standard of reference for the evaluation of soft tissues, and thus for the depictiion of disk position abnormalities and intrarticular effusion. KG parameters, which were claimed to be useful for diagnosing intracapsular disorders, were chosen on the basis of their supposed relevance regarding the MR assessments.
Based on this premise, deviations and deflections from the sagittal midline during jaw opening were included in the analysis for their potential relationship with the presence of disk displacement with and without reduction, respectively. Also, sudden-onset speed variations during jaw movements, i.e., incisures, were included because of their potential correlation with both disk disorders and joint effusion. For purposes of comparison with the dichotomic MR findings, all KG parameters were assessed as presence/absence instead of, e.g.,, adopting the millimeter measures of deviations/deflections from the midline and the raw number of incisures. This was due to the study strategy aiming to compare all KG variables with all MR findings in the attempt to describe multiple variable models that may help defining KG predictors for MR diagnoses.
The results showed that none of the KG variables were correlated with any of the MR findings, thus limiting all attempts to define multiple variable models to predict MR-based diagnoses. As a consequence of the poor correlation with imaging signs, the accuracy of jaw KG findings to predict MR diagnoses was not acceptable and too low to support the use of KG in the clinical setting. In particular, the high levels of false positives, as suggested by the very poor specificity and positive predictive values, are associated with a strong risk of overdiagnosing disease and overtreating subjects who do not actually need treatment. These suggestions are even more noteworthy if one considers that also the standard of reference adopted for comparison in this investigation, i.e., magnetic resonance, is losing indications for routine use. So, the use of instrumental electronic devices for analyzing TMD patients should stand comparison with less expensive diagnostic approaches even if those instruments did have a good agreement with MR findings. Based on these suggestions, the use of KG recordings of jaw movements as a diagnostic aid for TMJ disk displacement and effusion can not be supported.
Findings from the present study were in line with those of recent works suggesting that surface EMG is not accurate to predict the presence of myofascial pain16 and that KG recordings of jaw movements are not useful to monitor the disease if pain levels are assumed to be the main treatment outcome. All of these validation studies provided support to the negative findings of comprehensive reviews on the role of those technologic devices in the TMD practice. Therefore, clinicians proposing diagnostic and treatment approaches to TMD patients based on the analysis of jaw movements are strongly encouraged to reconsider their claims in the light of evidence-based findings suggesting that those instruments’ accuracy to diagnose disease is poor.
From a methodologic viewpoint, it must also be pointed out that data were drawn from a convenience sample of TMD patients in which subjects and joints with or without specific MR signs served as cases and controls. It could be argued that studies on larger samples of “pure” case and control subjects must be performed to confirm findings from this investigation.
Nonetheless, correlations between MR and KG findings had such a low level of significance that it is not likely that the distribution of findings could have been changed with recruitment of additional or different patients. In any case, a major strength of the present investigation is that it is easily replicable in the research as well as the clinical settings, thus offering a basis for data comparison with future studies. Moreover, it must also be borne in mind that, in theory, the duty of testing an instrument’s validity is the manufacturer’s, so a strong recall to the ethical duties of all those individuals involved in TMD and orofacial pain practice is recommended.
From a clinical viewpoint, it is also interesting that the poor correlation of jaw movements’ trajectories and velocity with MR-depicted disk displacement and effusion raises concerns about the common beliefs that disk position abnormalities are associated with peculiar jaw opening-closing patterns (e.g., deviations/deflections toward the affected side). On the other hand, it should also be pointed out that the role of muscle disorders as a factor influencing the jaw movement patterns was not assessed in this investigation, thus representing a potential factor of interest for future investigations.
There are additional information about TMJ radiodiagnostics you can gain on our author's course "School of radiodiagnostics in dentistry. Module 1:TMJ and maxillofacial area rediodiagnostics" by Kaan Orhan.
CONCLUSION
This investigation assessed the correlation between TMJ disk position abnormalities and joint effusion, as depicted with MR images, and jaw movement features, as recorded with KG devices, and a correlation between the findings from the 2 assessments was not observed. The accuracy of KG parameters to predict MR findings was not acceptable. Data from this investigation do not support the usefulness of jaw-tracking devices to detect TMJ disk displacement and effusion.
AUTHOR'S INFORMATION
Daniele Manfredini, DDS, PhD
Lorenzo Favero, MD
Elvis Federzoni, DDS
Francesco Cocilovo, DDS
Luca Guarda-Nardini, MD, DDSa
REFERENCES
Okeson JPO. Management of temporomandibular disorders and occlusion. 6th ed. St. Louis: Mosby-Elsevier; 2008.
Manfredini D, editor. Current concepts on temporomandibular disorders. Berlin: Quintessence; 2010.
Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992;6:301-55.
De Leeuw R, American Academy of Orofacial Pain. Orofacial pain: guidelines for assessment, diagnosis, and management. Chicago: Quintessence; 2008.
Petersson A. What you can see and can not see in TMJ imaging—an overview related to the RDC/TMD diagnostic system. J Oral Rehabil 2010;37:771-8.
Tasaki MM, Westesson PL. Temporomandibular joint: diagnostic accuracy with sagittal and coronal MR imaging. Radiology 1993;186:723-9.
de Leeuw R, Boering G, van der Kuijl B, Stegenga B. Hard and soft tissue imaging of the temporomandibular joint 30 years after diagnosis of osteoarthrosis and internal derangement. J Oral Maxillofac Surg 1996;54:1270-80, discussion 1280-1.
Kalaykova S, Lobbezoo F, Naeije M. Two-year natural course of anterior disc displacement with reduction. J Orofac Pain 2010;24:373-8.
Jankelson B. Neuromuscular aspects of occlusion. Effects of occlusal position on the physiology and dysfunction of the mandibular musculature. Dent Clin North Am 1979;23:157-68.
Lund JP, Widmer CG, Feine JS. Validity of diagnostic and monitoring tests used for temporomandibular disorders. J Dent Res 1995;74:1133-43.
Klasser GD, Okeson JP. The clinical usefulness of surface electromyography in the diagnosis and treatment of temporomandibular disorders. J Am Dent Assoc 2006;137:763-71.
Suvinen TI, Kemppainen P. Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J Oral Rehabil 2007;34:631-44.
Gonzalez Y, Iwasaki LR, McCall WD Jr, Ohrbach R, Lozier E, Nickel JC. Reliability of electromyographic activity vs. biteforce from human masticatory muscles. Eur J Oral Sci 2011;119:219-24.
Castroflorio T, Falla D, Wang K, Svensson P, Farina D. Effect of experimental jaw-muscle pain on the spatial distribution of surface EMG activity of the human masseter muscle during tooth clenching. J Oral Rehabil 2012;39:81-92.
Cooper BC. Parameters of an optimal physiological state of the masticatory system: the results of a survey of practitioners using computerized measurement devices. Cranio 2004;22:220-33.
Manfredini D, Cocilovo F, Favero L, Ferronato G, Tonello S, Guarda-Nardini L. Surface electromyography of jaw muscles and kinesiographic recordings: diagnostic accuracy for myofascial pain. J Oral Rehabil 2011;38:791-9.
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of rheumatology criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum 1990;33:160-72.
Matsuda S, Yoshimura Y, Lin Y. Magnetic resonance imaging assessment of the temporomandibular joint in disk displacement. Int J Oral Maxillofac Surg 1994;23:266-70.
Westesson PL, Erikson L, Kurita K. Reliability of a negative clinical temporomandibular joint examination: prevalence of disk displacement in asymptomatic temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;68:551-4.
Orsini MG, Kuboki T, Terada S, Matsuka Y, Yatani H, Yamashita A. Clinical predictability of temporomandibular joint disk displacement. J Dent Res 1999;78:650-60.
Haiter-Neto F, Hollender L, Barclay P, Maravilla KR. Disk position and the bilaminar zone of the temporomandibular joint in asymptomatic young individuals by magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:372-8.
Manfredini D, Tognini F, Zampa V, Bosco M. Predictive value of clinical findings for temporomandibular joint effusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:521-6.
Greene CS. The role of biotechnology in TMD diagnosis. In: Laskin DM, Greene CS, Hylander WL, editors. TMDs. An evidence-based approach to diagnosis and treatment. Chicago: Quintessence; 2006. p. 193-202.
Larheim TA. Role of magnetic resonance imaging in the clinical diagnosis of the temporomandibular joint. Cells Tissues Organs 2005;180:6-21.
Manfredini D, Guarda-Nardini L. Agreement between research diagnostic criteria for temporomandibular disorders and magnetic resonance diagnoses of temporomandibular disc displacement in a patient population. Int J Oral Maxillofac Surg 2008;37:612-6.
Manfredini D, Bucci MB, Montagna F, Guarda-Nardini L. Temporomandibular disorders assessment: medicolegal considerations in the evidence-based era. J Oral Rehabil 2011;38:101-19.
Clark GT, Tsukiyama Y, Baba K, Simmons M. The validity and utility of disease detection methods and of occlusal therapy for temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;83:101-6.
Greene CS. The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain 2001;15:93-105.
