Is early treatment over-treatment?
As far back as 1900 Angle began to preconize early treatment, in the 6th edition of his book, “Treatment of malocclusion of the teeth and fractures of the maxilla: Angle’s System reporting that treatment in children is easier and faster; nature, regarding growth, tissue repair and response behave better in the mixed dentition stage; waiting is a mistake due to malocclusion worsening and early treatment is more stable than late treatment”.
When Angle wrote about early treatment, he was referring to mixed dentition. Planas [1] in his book “Genesis de la Rehabilitacion Neuro-oclusal” approached the theme from a different perspective. He talked about prevention in the first year of life, and treatment in the deciduous dentition. According to Planas the physiological movement of the stomatognathic system is the main goal of early treatment which he preconized must be achieved with selective wear and the construction of Planas’ direct tracks made of resin on the deciduous teeth. Simões [2], in her levels of prevention, categorized what to treat and when to treat. Corroborating the concepts of Planas, in deciduous dentition the use of appliances is appropriate only in severe cases, such as conditions of anterior cross bite and displasias. She preconized the use of functional appliances in the mixed dentition at 7/8 years of age.
Neuroscience supports early treatment. Jou [3] reports that the maintenance of wrong afferences from the stomatognathic system can damage the brain. This will not appear in a young period of life because of the brain plasticity. When this plasticity decreases, the clinical manifestations of the problem begin.
The first thing to define is whether the early treatment is being performed in deciduous dentition or in the mixed dentition. Treatment protocols tend to be quite different. As quoted above, the use of appliances for the treatment of deciduous dentition is restricted. The main tools are occlusal plane adjustments and physiotherapy exercises.
Corroborating this thought, over 15 years ago, Turpin, in his Editorial in November of 2004 in the American Journal of Orthodontics and Dentofacial Orthopedics, clearly stated his point of view that more scientific evidence was necessary but reported that selective grinding would treat most of posterior cross bite corroborating Planas’ protocol of early treatment. In June of 2004, Turpin, also in his editorial, reported that even the use of expansion appliances was justifiable in the early treatment of posterior cross bite due to the severity of esthetic and functional consequences of this malocclusion.
Many cases of open bite are treated with occlusal plane adjustments to stimulate lateral movements of the mandible, as the type seen in Fig. 1 and Fig. 2. The change in movement pattern due to selective grinding is an extremely important factor to eliminate de the oral parafunction of non-nutritional sucking (fingers or pacifier), which even allows self-correction of the malocclusion, but the child was not able to cease with the parafunctional behavior until the occlusal adjustment was made. In Fig. 2 the grinding in the canines can be observed. It is extremely important to emphasize that the ankylosed tooth will not respond to any non-surgical treatment protocol. The aim of the occlusal plane adjustment is to create conditions for the child to change the pattern of mastication, thereby enhancing the lateral movement of the mandible during the masticatory cycle.
Some aspects have to be considered when planning an early treatment. Neural and mental development of the child are most important. For instance, one cannot use Planas’ protocol of adjustment of the occlusal plane with the aim of obtaining mature lateroprotrusive movements of the mandible before 4 or 5 years of age.
Many adjustments can and must be made in the occlusal plane to correct mandibular deviations, remove occlusal interferences, begin to stimulate lateroprotrusive movements, but watch out, congruence of the Temporomandibular Joint (TMJ) anterior eminence with incisor guide in protrusive movements and canine guide in lateral movements are crucial. If these issues are not respected the TMJ can be permanently damaged.
Furthermore, according to Jou (2018) [3], brain damage can be permanent. The author reported that wrong treatments can cause serious problems to the SNC including predisposing the patient to Alzheimer’s disease and dementia in the aging process.
 Fig. 1. Anterior open bite in deciduous dentition. Tooth 51 suffered a trauma from a fall and ankylosed
Fig. 1. Anterior open bite in deciduous dentition. Tooth 51 suffered a trauma from a fall and ankylosed
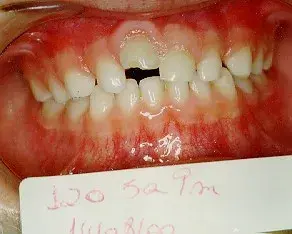 Fig. 2. The bite closed with occlusal plan adjustment. The grinding can be observed in the superior canines.
Fig. 2. The bite closed with occlusal plan adjustment. The grinding can be observed in the superior canines.
The aim is to stimulate more lateral movements during the masticatory cycle changing the vector of force dissipation in the periodontium and bone.
When treatment of a child in the mixed dentition stage is proposed, many authors reprove under the over treatment flag. For instance, if the malocclusion is a retrognathism the recommendation is waiting until the pre pubertal spurt due to a fast response caused by sexual hormones and GH. If the patient has only the anteroposterior discrepancy this idea of treatment could be right, but it very rarely occurs that the retrognathism is not accompanied by transversal and vertical problems in the mandible and/or maxilla. Therefore, let us remember the advice of Angle about a better response in the mixed dentition and that waiting could worsen the malocclusion.
New materials and treatment protocols and appliances are arriving with increasing speed some of them favor early treatment, such as the trainers from Myofunctional Research Co., the aligners and some new functional orthopedic appliances [4], for instance. I sincerely believe that more options will be created in the coming years. Two things are essential, more research about the subject was previously recommended by Turpin in 2004 and this is still underexploited. However, before creating new protocols, the existing protocols must be mastered with correct prescription and domain of the technics is crucial. Investigations about their efficacy is crucial for jaw functional orthopedics based on scientific evidence. In research like this of Dimberg et al. [5], control groups will be very rare because neuroscience findings have increasingly shown the importance of a healthy mouth to a healthy brain at an early age.
There is a wide field and much need for investigations into the subject of early treatment and, to my way of thinking, the most important question is why do some individuals and some cases of malocclusion self-correct with the removal of the parafunctional habit and others do not. Is this due to genetics, duration and/or intensity of the parafunction? Why?
This issue is dedicated to Pedro Planas who fought with all his strength to make early treatment became a reality.
You have the opportunity to gather more in-depth information about early orthodontic treatment on our website.
Author: Orlando Santiago Júnior
References
P. Planas, Rehabilitación neuro-oclusal (RNO). 2a Ed. (in Spanish), Barcelona: Masson Salvat Odontologia, 1994.
W. A. Simões, Ortopedia funzionale dei mascellari Attraverso La Riabilitazione Nuero-Occlusale. 5a Ed. (in Italian), Orbetello, 2010.
Y.-T. Jou, “Dental deafferentation and brain damage: A review and a hypothesis,” The Kaohsiung Journal of Medical Sciences, Wiley, 2018.
O. Santiago Júnior, M. Vedovello Filho, M. V. Lucas Ferreira, and R. Huebner, “Functional orthopedic appliance for vertical dimension increase and mandibular deprogramming ORLANDO SANTIAGO SYSTEM 1 – OSS1. Indications and laboratorial manufacturing,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 1, No. 1, pp. 12–17, Jun. 2021.
L. Dimberg, B. Lennartsson, K. Arnrup, and L. Bondemark, “Prevalence and change of malocclusions from primary to early permanent dentition: A longitudinal study,” The Angle Orthodontist, Vol. 85, No. 5, pp. 728–734, Aug. 2015.
