Interarch space assessment in edentulous patients rehabilitated with complete removable dentures using open-access software
Abstract
Background: The interarch space is defined as the vertical space between the edentulous ridge and the occlusal or incisal aspect of the opposing arch. Measuring the interarch space in a patient requiring an implant-supported fixed prosthesis is crucial for determining the prostheses to be used in each clinical situation. Depending on the measurements and other factors, such as the need for lip support or pink esthetics issues, decisions about the most convenient type of implant-supported prosthesis can be taken. Analogic workflow to measure the interarch space can represent a time-consuming and expensive procedure that may lead to inaccuracies.
Objective: To describe a step-by-step protocol to measure the upper and lower interarch space with open-access software, starting from the digital scan of the patient’s complete dentures obtained with an intraoral scanner.
Methods: An extraoral scan (using an intraoral scanner) of the existing complete removable prosthesis is required to assess the interarch space for making an implant-supported prosthesis treatment planning. If the existing complete denture does not fulfill the required functional and esthetic parameters, a complete interim denture, a wax trial denture, or a printed denture prototype should be previously fabricated. The antagonist arch and the intermaxillary record scan also need to be obtained. Finally, all STL files are imported into an open-access software for measuring the interarch space.
Results: Open-source software can be used to measure the upper and lower interarch space from existing complete dentures following the step-by-step protocol outlined in this paper.
Conclusion: Interarch space of edentulous patients rehabilitated with complete dentures can be measured with a 360 degrees scanning of the existing complete denture and open-access software by applying the protocol outlined in this paper.
Clinical relevance: The clinician can assess and digitally measure the interarch space of edentulous patients requiring an implant-supported fixed prosthesis using an open access software.
You have the opportunity to gather more in-depth information about total rehabilitation in our course "Indirect restoration in the biomimetic concept".
Introduction
Implant-supported fixed prostheses (with/without pink gingiva) or overdentures (on single anchors or bars) represent a satisfactory solution to rehabilitate most patients with complete edentulism. Several extraoral and intraoral factors, such as lip support, cleanability, and prosthetic space, must be considered when determining the correct indication of each type of prosthesis [1–7]. The need for a vestibular flange covering the existing alveolar ridge to ensure correct lip support or to mask the gingival exposure in high smile patients will make the clinician choose removable prostheses or overdentures [1,3-6]. The inability of the patient to achieve adequate hygiene of the implant-supported prosthesis due to, for example, limitations in manual dexterity may also determine the use of removable prosthetic solutions [6,8].
Further details are accessible for you to learn on our website.
The interarch space, defined as the vertical distance between the maxillary and mandibular dentate or edentulous arches, is crucial for determining the prostheses to be used in each clinical situation. The minimum interarch space for a fixed prosthesis is 9-10 mm [1-2,7]. Overdentures require more interarch space to include all the prosthetic components: the anchors (unitary or bar type), the retentive elements, the reinforcement structure, the pink veneering resin, and the prosthetic teeth. Insufficient space will cause prosthetic structural weakness, which could lead to fractures [3,9-10]. The literature recommends a minimum clearance of 13-14 millimeters for bar overdentures and 9-12 millimeters when using unitary anchors [3,7,11]. It is considered that for correct performance of the unitary anchors in the medium and long term, there should not be significant angular divergences between them [12].
Nevertheless, the centripetal resorption pattern of the maxilla often makes it very difficult to place implants without significant deviations [11,13], which often leads to the need for bar-supported prostheses, which demands more interarch space [1-3,13]. It is also advisable to consider the opposing arch and the patient’s muscular strength. In general terms, the more fixed the opposing arch and the higher patient’s muscular strength, the more reinforced the implant-supported removable prosthesis must be, and subsequently, more space will be required [14–16].
It is necessary to acknowledge the position of the teeth of the future prosthesis to measure the interarch space of each maxillary arch, upper and lower. A complete denture with correct esthetic and functional parameters is crucial before planning any implant-supported prosthesis. These parameters include the vertical occlusion dimension, incisal plane, occlusal plane, size and teeth position, and teeth exposure at rest and smile [17–19]. If the patient does not have a denture fulfilling the previously described functional and esthetic parameters, a mucosa-supported interim complete denture, a wax trial denture, or a printed complete denture prototype should be performed during the planning phase. However, on many occasions, patients are already rehabilitated with acceptable complete dentures that may be used for implant-supported treatment planning [6-7,20]. The interarch space can be measured analogically in the articulator by mounting the casts with the complete dentures of the patient [6,20].
The upper interarch space can then be measured in the articulator by removing the complete upper denture and vice versa. This procedure can be time-consuming, and the patient is left without the removable prostheses during the articulator mounting procedure. The interarch space could also be determined by measuring the thickness of the patient’s complete dentures, wax rims, or wax trial dentures with a Boley gauge (Hu-Friedy; Chicago) [7]. Currently, no digital method to measure the interarch space without physical casts and articulators was found in the literature. The objective of this article is to describe a step-by-step protocol to measure the upper and lower interarch space with open-access software from the digital scan of the patient’s complete dentures obtained with an intraoral scanner.
Methods
The protocol for measuring the upper and lower interarch space with open-source CAD software proceeds as follows:
Reline the complete denture in light occlusion with light body polyvinylsiloxane (PVS) silicone (Virtual light body; Ivoclar Vivadent), white-zinc oxide paste (Impression Paste; SS White), or polysulfide (Permlastic; Kerr). Then, make a 360-degree digital scan with an intraoral scanner (TRIOS 3; 3Shape A/S) of the superior and inferior complete denture. A 360-degree digital scan requires acquiring the outer part and the intaglio of the complete removable denture, and it is performed extra-orally with an intraoral scanner. Contrast spray (Vita Powder Scan Spray; Vita) can ease the scanning procedure overcoming brightness issues. In case of complete edentulism of both arches, make the procedure with the two complete dentures. After, make a bite registration scan. Finally, remove the impression material from the intaglio of the complete denture, and return the denture to the patient.
Import the Standard Tesselation Language (STL) files of the complete dentures or the antagonist scans into Meshmixer (Meshmixer; Autodesk Corp). In case scanning inaccuracies are present (Fig 1A), the Meshmixer "Inspector" function could be used to repair the resulting mesh. (Fig 1B) This tool arbitrarily fixes the mesh of the most frequent errors, such as floating mesh areas or holes. (Fig 1C) This repairing can cause inaccuracies which may not influence the planning or measurements of the interarch space.
Select (Select tool in the left column or shortcut key "S") the intaglio of the prosthesis (Fig 2A). The size of the tool area can be adjusted by pressing the space bar. Keep the shift key pressed to erase any undesired selected areas. Use the smooth boundary tool to refine the borders of the chosen area (Modify> Smooth Boundaries or shortcut key "B").
Invert the selection (Modify>Invert or shortcut key "I") (Fig 2B). Erase the selected area (Edit>Discard or shortcut "X") (Fig 2C). Then, select the entire remaining scan (shortcut key "Control or Command +A"), and make an extrusion (Edit> Extrude or shortcut key "D"), adjusting the offset to 15 mm, with a constant direction and a flat end type. Extruding with these parameters will flip the remaining mesh of the scan, and it will pull all mesh in a constant direction finishing in a flat surface, resulting in a closed mesh design similar to a trimmed analogic edentulous cast [21] (Fig 2D).
Repeat steps 3 and 4 if the patient has a complete denture in the opposite arch (Fig 3). Next, import and append the files corresponding to the scanned complete dentures again (Fig 4).
Hide the prosthesis corresponding to the arch to be measured by unclicking the eye toggle icon in the object browser and showing the antagonist arch. Measure from the edentulous mucosa of the cast of the arch to the treated to the opposing teeth using the "Units / Dimensions" measurement tool, found within the Analysis menu in the left column menu (Analysis> Units / Dimensions). The length of the selected length is indicated in millimeters in the “Real Length” option at the “Set from Measurements” information showed at the lower part of the “Units/Dimensions” window (Fig 5).
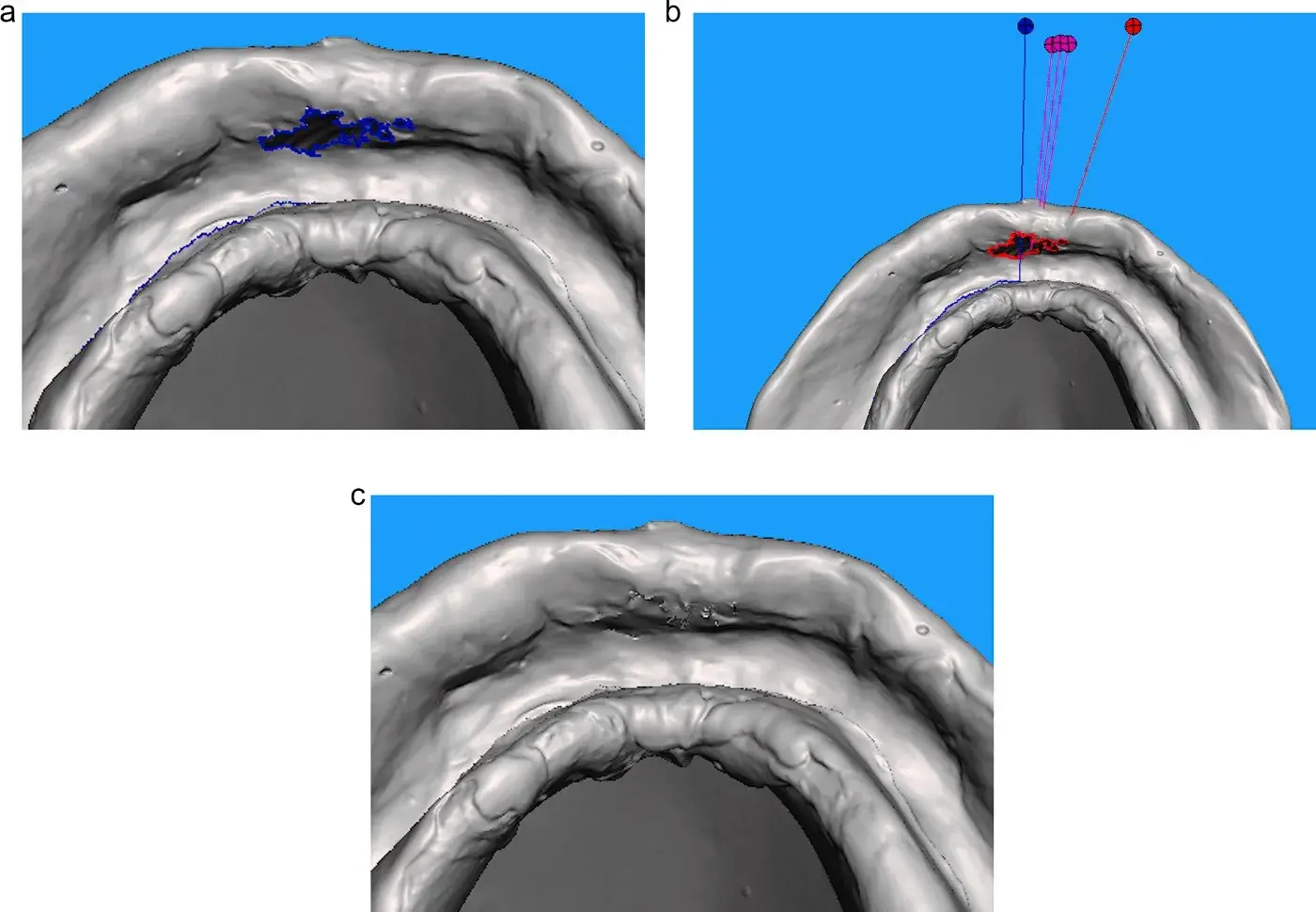 Fig. 1. A. Detail of defects in the resulting mesh after 360-degree scanning of complete dentures, Fig 1B. Meshmixer’s "Inspector" tool for mesh defects repairing, Fig 1C. Mesh of complete denture scan repaired with Meshmixer’s "Inspector" tool.
Fig. 1. A. Detail of defects in the resulting mesh after 360-degree scanning of complete dentures, Fig 1B. Meshmixer’s "Inspector" tool for mesh defects repairing, Fig 1C. Mesh of complete denture scan repaired with Meshmixer’s "Inspector" tool.
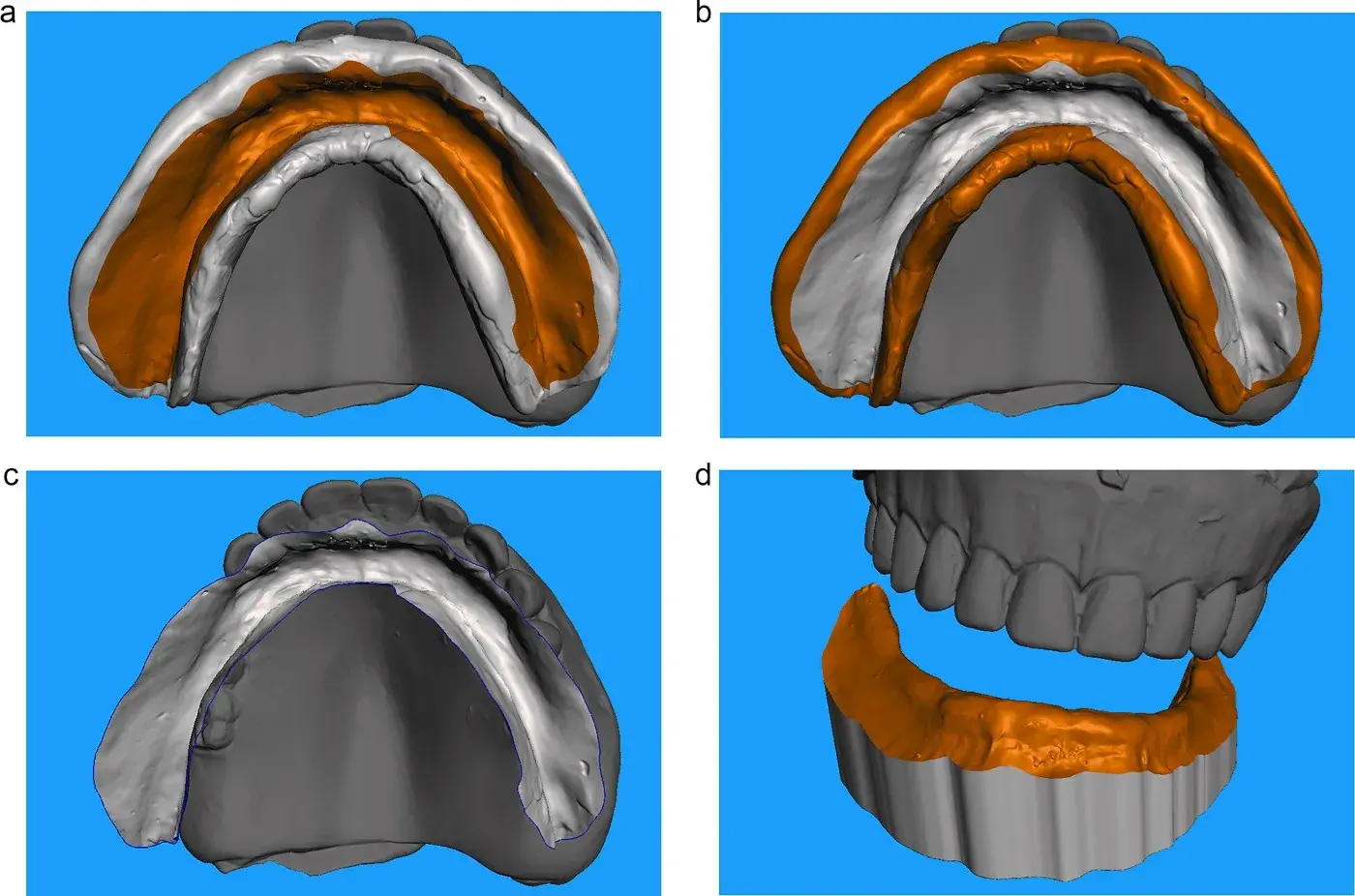 Fig. 2. A. Selection of intaglio of lower complete denture scan., Fig 2B. Inverted selection., Fig 2C. Remaining scan after erasing inverted selection., Fig 2D. Extrusion of remaining scan with -15 mm offset, constant direction, and flat end type.
Fig. 2. A. Selection of intaglio of lower complete denture scan., Fig 2B. Inverted selection., Fig 2C. Remaining scan after erasing inverted selection., Fig 2D. Extrusion of remaining scan with -15 mm offset, constant direction, and flat end type.
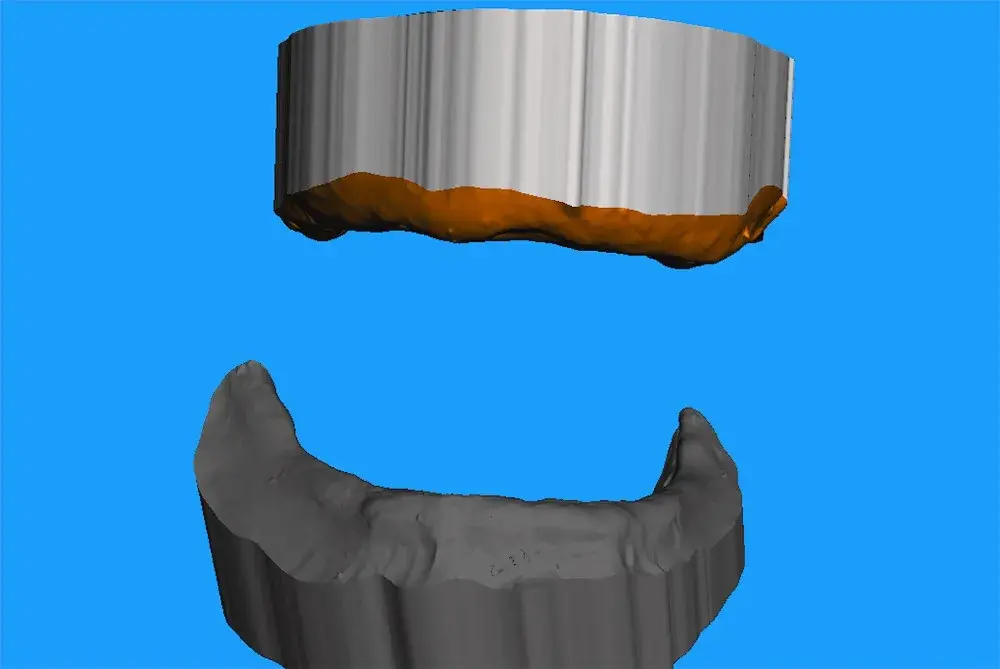 Fig. 3. Extrusion of remaining scan with -15 mm offset, constant direction, and flat end type.
Fig. 3. Extrusion of remaining scan with -15 mm offset, constant direction, and flat end type.
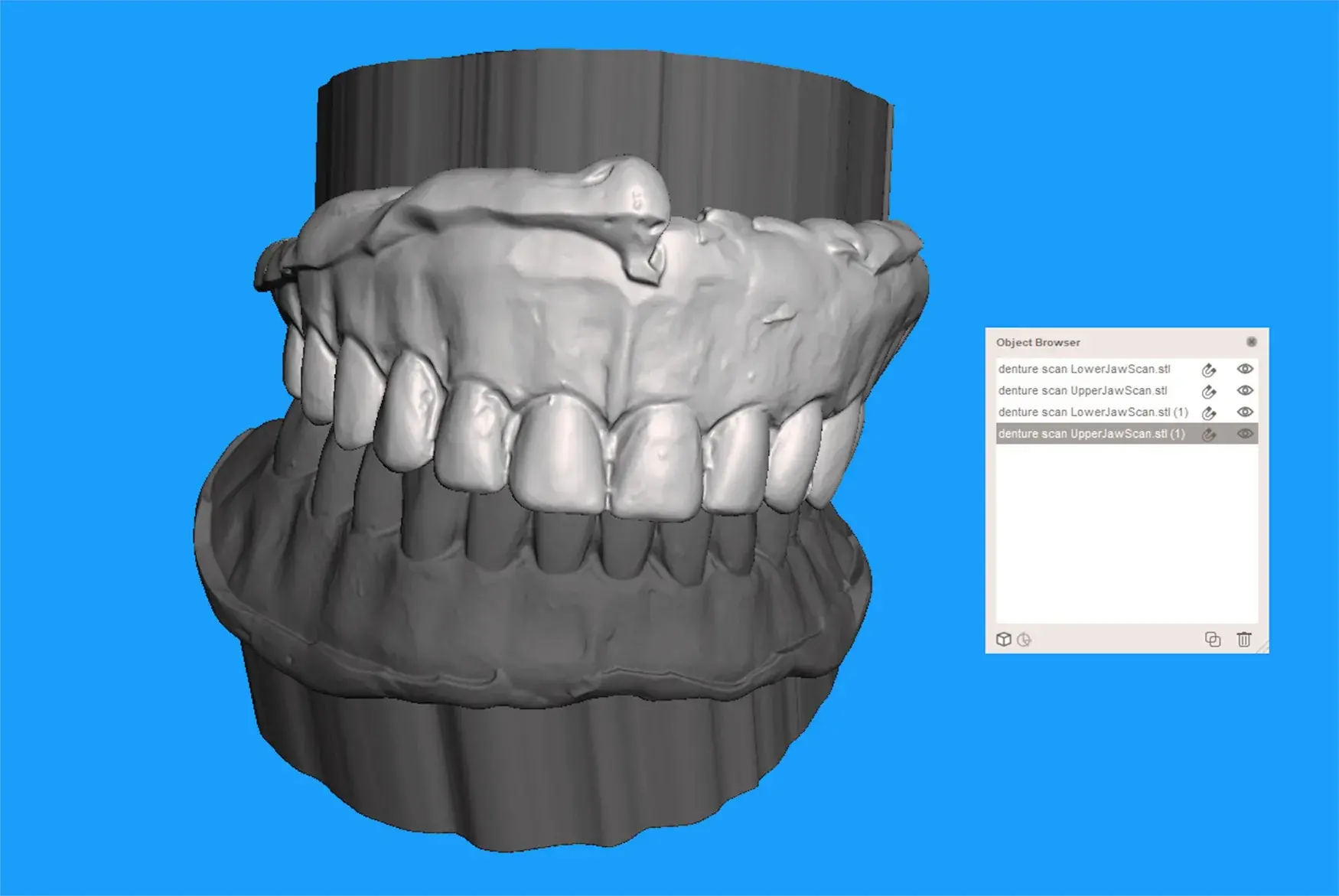 Fig. 4. Import and append scanned complete dentures again into Meshmixer.
Fig. 4. Import and append scanned complete dentures again into Meshmixer.
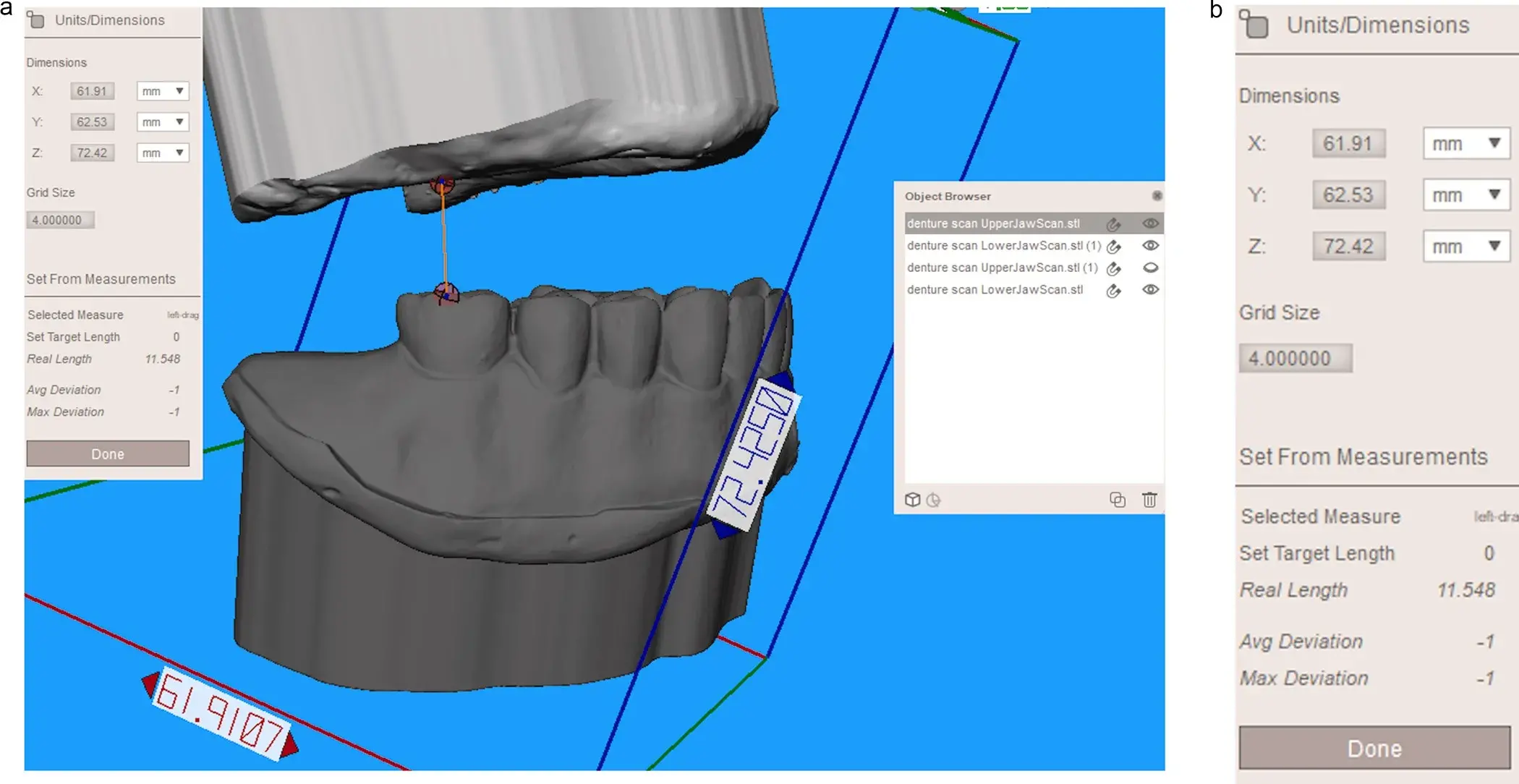 Fig. 5. A. Hiding of upper complete denture and measurement of posterior upper interarch space, Fig 5B. Detail of the “Units & Dimensions” window where selected length is displayed in millimeters in “Real Lengh” option.
Fig. 5. A. Hiding of upper complete denture and measurement of posterior upper interarch space, Fig 5B. Detail of the “Units & Dimensions” window where selected length is displayed in millimeters in “Real Lengh” option.
Results
Open-source software (Meshmixer, Autodesk, San Rafael, USA) can be used to measure the upper and lower interarch space from existing complete dentures following the step-by-step protocol outlined in this paper. Following the above procedure, clinicians can obtain edentulous casts from the existing complete dentures, where the needed measurements can be performed.
Discussion
The protocol described in this manuscript can be applied to fully edentulous patients of one or both arches with dentures fulfilling the correct functional and aesthetic parameters. Determining the position of teeth in the final prosthesis is paramount to assessing the interarch space in case of fully edentulism [1,3,5,17]. When performing the measurements, it is necessary to hide the complete denture STL file corresponding to the arch from which the measurement is to be made, leaving the opposing arch visible.
Suppose the patient does not have complete dentures fulfilling the required functional and aesthetic parameters. In that case, it is advisable to perform a complete interim denture, a wax trial denture, or a printed complete denture prototype during the planning phase [6,22-28]. If the complete interim denture design is made virtually, following a digital protocol, it is necessary to scan the edentulous arches and their occlusion beforehand [27–28].
In this case, the interarch space measurement can be performed with the virtual design of the denture, so the scanning of the denture is not required. If the complete interim denture is manufactured following a conventional protocol, the scanning of the finished denture or the wax trial denture, in case the finishing of the prosthesis is not desired, and the application of the protocol described in the present manuscript allows the measurement of the interarch space straightforwardly.
The interarch space could be determined easily by measuring the thickness of the patient’s complete dentures [7]. However, with the described protocol, a properly articulated cast of the edentulous arch is obtained from the complete denture scan, which is very helpful for interarch space assessment, as described in the manuscript, and other essential steps to plan the final prosthesis. The resulting cast can be exported to an STL file for later use as an operative scan in proprietary dental CAD software, such as Exocad (Exocad ChairsideCAD, Exocad GmBh, Darmstadt, Germany). Then, interarch space assessment could be performed using the measuring tools of the proprietary dental CAD software. In addition, a digital wax-up design can then be performed with the obtained cast and the antagonist scan. The scanned complete dentures’ STL files could also be uploaded as pre-operative scans, serving as a reference in the designing process. The resulting digital design can then be transformed into a trial denture prototype fabricated with 3D printing technology by adding a base plate with or without a buccal flange. Thus, the printed trial denture will be helpful to assess the need for lip and facial support and the esthetics of the proposed digital waxing. In general, an overdenture will be advised if lip or facial support is required and for cases in which masking the gingival exposure in high smile patients is necessary [1–6]. On the other hand, a fixed prosthesis with pink esthetics will be indicated when no lip support is needed and when there is no gingival exposure during smiling [1–6]. Finally, the approved waxing can be helpful for prosthetically guided implant planning and for fabrication of immediate loading prostheses or interim removable dentures [6,29-30].
The described protocol only showed how to obtain an articulated edentulous cast from a complete denture. The edentulous cast could also be obtained following the described protocol with a 360 degrees scan of the articulated wax trial try-in. Then, interarch space assessment and final prosthesis digital designing could be performed using appropriate software.
Among the limitations of the present technique is the difficulty in scanning the entire surface of the complete denture and the fact that the technique’s accuracy is not proved. Current intraoral scanners may present issues in scanning deep areas of the intaglio of the complete denture. Moreover, the transition while scanning from the external part to the intaglio of the prosthesis might generate errors in the resulting mesh. The use of contrast scanning sprays may be helpful [31]. Nevertheless, the resulting inaccuracies may not influence the planning or measurements of the interarch space, and the post-processed scans could be adopted to fabricate the interim prostheses or printed trial dentures prototypes. Another limitation is the need for a learning curve to use Meshmixer, which is not user-friendly; in fact, it is sometimes challenging. Following the step-by-step protocol outlined in this paper will provide interarch measurements straightforwardly, but the first attempts may take a long time.
There are more additional information in our course Removable dentures.
Conclusions
Interarch space of edentulous patients rehabilitated with complete dentures can be measured with a 360 degrees scanning of the existing complete dentures and open-access software by applying the protocol outlined in this paper.
Afterward, depending on the measurements and other factors, such as the need for lip support or pink esthetics issues, decisions about the most convenient type of implant-supported prosthesis can be taken.
Declaration of Competing Interest
Authors confirm that this manuscript has not been published else-where, nor is it under consideration by another journal. The authors have no conflicts of interest to declare.
References
W. Daudt Polido, T. Aghaloo, TW. Emmett, TD. Taylor, D. Morton, Number of implants placed for complete-arch fixed prostheses: A systematic review and meta-analysis, Clin. Oral Implants. Res. 29 (2018) 154–183.
A. Tunkiwala, U. Kher, NH. Vaidya, ABCD" Implant classification: a comprehensive philosophy for treatment planning in completely edentulous arches, J. Oral Implantol. 46 (2020) 93–99.
J. Carpentieri, G. Greenstein, J. Cavallaro, Hierarchy of restorative space required for different types of dental implant prostheses, JADA 150 (2019) 695–706.
L. Lago, B. Rilo, N. Fernandez-Formoso, L. DaSilva, Implant rehabilitation planning protocol for the edentulous patient according to denture space, lip support and smile line, J. Prosthodont. 26 (2017) 545–548.
A. Pollini, J. Goldberg, R. Mitrani, D. Morton, The lip-tooth-ridge classification: a guidepost for edentulous maxillary arches. Diagnosis, risk assessment, and implant treatment indications, Int. J. Periodontics Restorative Dent. 37 (2017) 835–841.
SJ. Sadowsky, B. Fitzpatrick, DA. Curtis, Evidence-based criteria for differential treatment planning of implant restorations for the maxillary edentulous patient, J. Prosthodont. 24 (2014) 433–446.
S. Ahuja, DR. Cagna, Defining available restorative space for implant overdentures, J. Prosthet. Dent. 104 (2010) 133–136.
J. Dudley, Implants for the ageing population, Aust. Dent. J. 60 (2015) 28–43.
CK. Lee, JR. Agar, Surgical and prosthetic planning for a two-implant-retained mandibular overdenture: a clinical report, J. Prosthet. Dent. 95 (2006) 102–105.
A. Messias, P. Nicolau, F. Guerra, Different interventions for rehabilitation of the edentulous maxilla with implant-supported prostheses: an overview of systematic reviews, Int. J. Prosthodont. 34 (2020) s63–s84.
SJ. Sadowsky, Treatment considerations for maxillary implant overdentures: a systematic review, J. Prosthet. Dent. 97 (2007) 340–348.
MA. Elsyad, FA. Setta, AS. Khirallah, Strains around distally inclined implants retaining mandibular overdentures with locator attachments: an in vitro study, J. Adv Prosthodont. 8 (2016) 116–124.
S. Ahuja, DR. Cagna, Classification and management of restorative space in edentulous implant overdenture patients, J. Prosthet. Dent. 105 (2011) 332–337.
C. Ohkubo, KW. Baek, Does the presence of antagonist remaining teeth affect implant overdenture success? A systematic review, J. Oral Rehabil. 37 (2010) 306–312.
MF. Gibreel, A. Khalifa, MM. Said, F. Mahanna, N. El-Aimer, TO. N¨arhi, et al., Biomechanical aspects of reinforced implant overdentures: a systematic review, J. Mech. Behav. Biomed. Mater. 91 (2019) 202–211.
YT. Hso, JH. Fu, K. Al-Hezaimi, HL. Wang, Biomechanical implant treatment complications: a systematic review of clinical studies of implants with at least 1 year of functional loading, Int. J. Oral Maxillofac. Implants. 27 (2012) 894–904.
AS. Bidra, Three-dimensional esthetic analysis in treatment planning for implant-supported fixed prosthesis in the edentulous maxilla: review of the esthetics literature, J. Esthet. Restor. Dent. 23 (2011) 219–236.
M. Calamita, C. Coachman, N. Sesma, J. Kois, Occlusal vertical dimension: treatment planning decisions and management considerations, Int. J. Esthet. Dent. 14 (2019) 166–181.
FM. Spear, VG. Kokich, DP. Mathews, Interdisciplinary management of anterior dental esthetics, JADA 137 (2006) 160–169.
NF. AbuJamra, MM. Stavridakis, RB. Miller, Evaluation of interarch space for implant restorations in edentulous patients: a laboratory technique, J. Prosthodont. 9 (2000) 102–105.
O. Figueras-Alvarez, F. Real-Voltas, Straightforward procedure for fabricating a digital cast from a conventional impression with a dental scanner and a free software program, J. Prosthet. Dent. (2020) 20, https://doi.org/10.1016/j. prosdent.2020.08.046.
E. Ellis, D. Mc Fadden, The value of a diagnostic setup for full fixed maxillary implant prosthetic, J. Oral Maxillofac. Surg. 65 (2007) 1764–1771.
WA. Clark, I. Duqum, BJ. Kowalski, The digitally replicated denture technique: a case report, J. Esthet. Restor. Dent. 31 (2019) 20–25.
S. Kourtis, K. Kokkinos, V. Roussou, Predicting the final result in implant-supported fixed restorations for completely endentulous patients, J. Esthet. Restor. Dent. 26 (2014) 40–47.
WM. Ahmed, TV. Verhaeghe, APG. McCullagh, Maxillary complete-arch implant-supported restoration: a digital scanning and maxillomandibular relationship workflow, J. Prosthet. Dent. 125 (2021) 216–220.
Y. Sa, D. Morton, WS. Lin, Using existing interim complete dentures as an aid for an interocclusal record to align edentulous intraoral scans for implant-retained overdentures, J. Prosthet. Dent. 125 (2021) 854–857.
PM. Muniz, ED. Kukucka, Incorporating digital dentures into clinical practice: flexible workflows and improved clinical outcomes, J. Prosthodont. 30 (2020) 125–132.
J. Espona, C. Vidal-Ponsoda, P. Quintana, V. Henarejos-Domingo, M. Roig, A fully digital protocol to provide a fixed interim complete denture for immediate loading for a completely endentulous patient: a dental technique, J. Prosthet. Dent. 21 (2021), https://doi.org/10.1016/j.prosdent.2021.09.011.
A. Ozkomur, F. Manfroi, Multifunctional guide for implant placement, impressions, and an occlusal index for fixed complete dentures, J. Prosthodont. 27 (2018) 197–200.
J. Katsoulis, P. Pazera, R. Mericske-Stern, Prosthetically driven, computer-guided implant planning for the edentulous maxilla: a model study, Clin. Implant. Dent. Relat. Res. 11 (2009) 238–245.
SI. Hategan, TF. Ionel, L. Goguta, A. Gabrilovici, MD. Negrutiu, A. Jivanescu, Powder and powder-free intra-oral scanners: digital impression accuracy, Prim. Dent. J. 7 (2018) 40–43.
Oscar Figueras-Alvarez, Associate Professor
Anna Clua-Palau, Assistant Professor
Lucas Queiroz Caponi, Assistant Professor
Carla Vidal-Ponsoda, Assistant Professor


