Clinical performance of resin composite restorations
Abstract
Purpose of Review This article reviews recent evidence and provides a general overview on the clinical performance of resin composite restorations. Four electronic databases were searched for articles that investigated factors associated with the long-term performance and failure of resin composites placed in anterior and posterior teeth. Signs that could be observed in aging restorations were also addressed.
Recent Findings Resin composite restorations fail due to the same reasons that lead to restoration of teeth, namely: caries, esthetics, fractures, and wear. Variables infuencing failure rates include tooth-related factors (e.g., loss of dental tissue, quality of remaining structure, tooth position, endodontic treatment) and patient-related risk factors (e.g., caries, parafunctional habits, sex, age, socioeconomic variables). State of the art restorative techniques and materials have limited infuence on the durability of resin composite restorations. Dentists and their clinical decisions also play a signifcant role in longevity, including their approach to aging restorations that are in service. Aging restorations may show surface and marginal staining, loss of anatomical shape and translucency, wear, chipping, fractures, and other minor defects that do not need intervention.
Summary The clinical service of resin composite restorations is a challenging aspect of their longevity, but posterior and anterior composites can achieve long-lasting clinical durability. Patients’ risks appear to be the most predominant factors afecting longevity. In general, the longevity of restorations would be longer if dentists were to use a more conservative approach when dealing with aging restorations in service.
Further details about composite restorations are accessible for you to learn in our course "Brazilian School of Aesthetic Restorations".
Introduction
The use of resin-based materials represents the fundamental basis of contemporary restorative dentistry that is primarily based on adhesive approaches. Adhesive restorative procedures allow the use of additive restorations and minimally invasive practices. Although silver amalgam was still regarded as being a longer-lasting material than resin composite in a recent meta-analysis, the evidence was classifed as being of low certainty and having high risk of bias [1]. In addition, the analysis was not based on recent studies. The authors suggested new research to demonstrate the long‐term efectiveness and safety of contemporary composites.
However, there is abundant evidence that resin composites can be used in direct, semi-direct, and indirect versions of restorations for a multitude of clinical scenarios in which amalgam has little space. Moreover, it is implausible that a large scale randomized clinical study could be designed adequately to compare amalgam and resin composite, mainly due to environmental issues and because amalgam does not ft the minimally invasive concept.
Longitudinal studies published in the past decade have confrmed a long-lasting clinical performance of resin composites [2–5, 6, 7–9, 10]. Studies with observation time intervals of longer than 25 years have reported annual failure rates (AFRs) of around 2% [3, 4, 7]. However, the majority of long-term studies are conducted in university settings or in a single dental ofce. For example, in a practice-based study with 24 general dental practitioners, AFRs as high as 8% were reported for posterior restorations [5]. Long-term studies with anterior restorations are limited and indicate survival rates that are comparable with those for posterior restorations, although with diferent failure characteristics [6, 8].
The long-term durability of resin composite restorations does not mean that longevity is no longer a challenge. In a recent study in the UK, with over 3.5 million composite restorations placed by multiple operators, in diverse clinical scenarios, approximately 59% of restorations survived for 5 years, 43% survived for 10 years, and 34% for up to 15 years [9]. In the same study, 7% of the teeth restored with resin composite had been extracted after 15 years [9]. These fgures suggest that restoration failure is likely to occur over the course of time. The intraoral environment imposes varied mechanical and biochemical challenges to restorations and adhesive interfaces, including loading, humidity, temperature changes, bioflm accumulation, and erosive and abrasive challenges. The restorative materials may react to the harsh environment by hydrolysis, leaching, color change, staining, fatigue, and cracking. Resin composite restorations may fail clinically due to the same reasons that lead to restoration of teeth, namely caries, esthetics, fractures, and/or wear [11••].
The longevity of restorations is subjected to higher levels of challenge to both the dentition and materials in high-risk situations such as in cases of patients with active caries, bruxism, and tooth wear.
Several factors have been reported to be associated with the failure rates of resin composite restorations. A classic review article in 2012 stated that the longevity of posterior restorations was not only a matter of materials [12], and this was corroborated by subsequent fndings of clinical studies. In addition to material- and technique-related factors that may increase the risk of failures, tooth-related variables, patient- and professional-related aspects play signifcant roles in resin composite durability. This article reviews recent evidence and provides a general overview on challenges to the clinical performance of resin composite restorations. Signs that could be observed in aging restorations were also addressed.
Factors Associated With Failures
Literature Search
Four electronic databases were searched for articles investigating the clinical performance of anterior and posterior resin composite restorations: PubMed, Scopus, Web of Science, and Google Scholar. The following keywords were used alone or in combination: dental, composite, restoration, clinical, longevity, durability, and performance. All the articles were eligible, but special attention was given to recent literature (last 5 years), clinical studies with follow-up periods≥5 years, and articles investigating the infuence of tooth-related variables, patients’ risks, and dentists’ decisions on the performance of resin composite restorations.
Tooth‑Related Factors
The two clinical cases shown in Fig. 1 represent diferent challenges to the restorative technique and clinical service of any type of restoration. The reasons why case B would generally be more challenging than case A include several aspects. Greater loss of dental structure and the presence of fewer cavity walls will increase the mechanical challenges imposed on the underlying remaining structure. Several studies have shown that multiple-surface restorations are at higher risk of failure [5, 6, 8, 9, 10, 11, 13–15]. The cavity size may have a greater impact on restoration survival in the premolar than in molar teeth [13]. The quality of the remaining structure is also essential, including the presence of cracks [16, 17]. The dentin in A is sound and superfcial, whereas the dentinal tissue is sclerotic and deep in B. Deep margins are more difcult to access and to keep moisture-free during adhesive procedures. Deeply located cervical margins are more likely to result in restoration failure than margins ending in enamel [18]. The larger restorative interface in B means more hydrolytic challenges to the bond stability.
In A, all margins are located in enamel, which is regarded as a better substrate than dentin/cementum for the purpose of bonding and the recommendation has been to preserve the enamel as much as possible when preparing teeth for restorations [19].
Type of tooth, its position, and antagonistic contacts are also relevant features in longevity [20]. Diferent studies show that restorations may survive longer in the premolars than in molars [2, 5, 11, 13]. Reports have indicated that resin composite restorations in the mandibular teeth showed better performance than those in the maxillary teeth [6, 9]. Furthermore, direct restorations in the maxillary teeth of patients with tooth wear showed more wear after 5 years than restorations in the mandibular teeth [21]. Another study reported similar AFRs of restorations throughout the four quadrants of dental arches, but restorations in the frst molar failed more frequently than those in the other teeth [5]. An 8-year retrospective study reported more failures in anterior than posterior restorations [14]. Anterior and posterior restorations may show distinct reasons for failure in the long term, particularly because esthetic failures are more prevalent in the front teeth [8].
The need for endodontic treatment is one of the most distinctive aspects between the cases shown in Fig. 1 to infuence the prognosis, long-term survival, and success of teeth and restorations [5, 9, 10, 11, 13, 22]. A practice-based study with over 430,000 restorations reported that fewer than 20% of those placed in endodontically treated teeth (ETT) survived after 10 years [5]. A 22% lower success rate of Class II restorations in ETT when compared with vital teeth was reported after 6–13 years [22]. The reasons for failure also difered: in ETT, secondary caries, root and cusp fracture, loss of retention, and restoration fracture were observed. In vital teeth, restorations failed mainly due to secondary caries and restoration fracture [22]. In a period of up to 18 years, a clinical study on anterior and posterior ETT reported that the quality of endodontic flling and coronal marginal adaptation were important factors that infuenced the long-term clinical complications [23]. In contrast, the presence of a post did not have a signifcant infuence [23].
In fact, there is increasing discussion on using or not using posts to restore ETT [24] because the maintenance of cavity walls and ferrule efect appear to be predominant factors in the survival of teeth and restorations [25]. A study with a 10-year period of follow-up on the survival of teeth and success of postless resin composite restorations in ETT suggested that the clinical routine of placing posts should be critically revised [26]. According to a cost analysis study, the use of posts for restoring ETT may be costly both in the initial phase of the restorative treatment and in the long-term due to the need for treating complications [27].
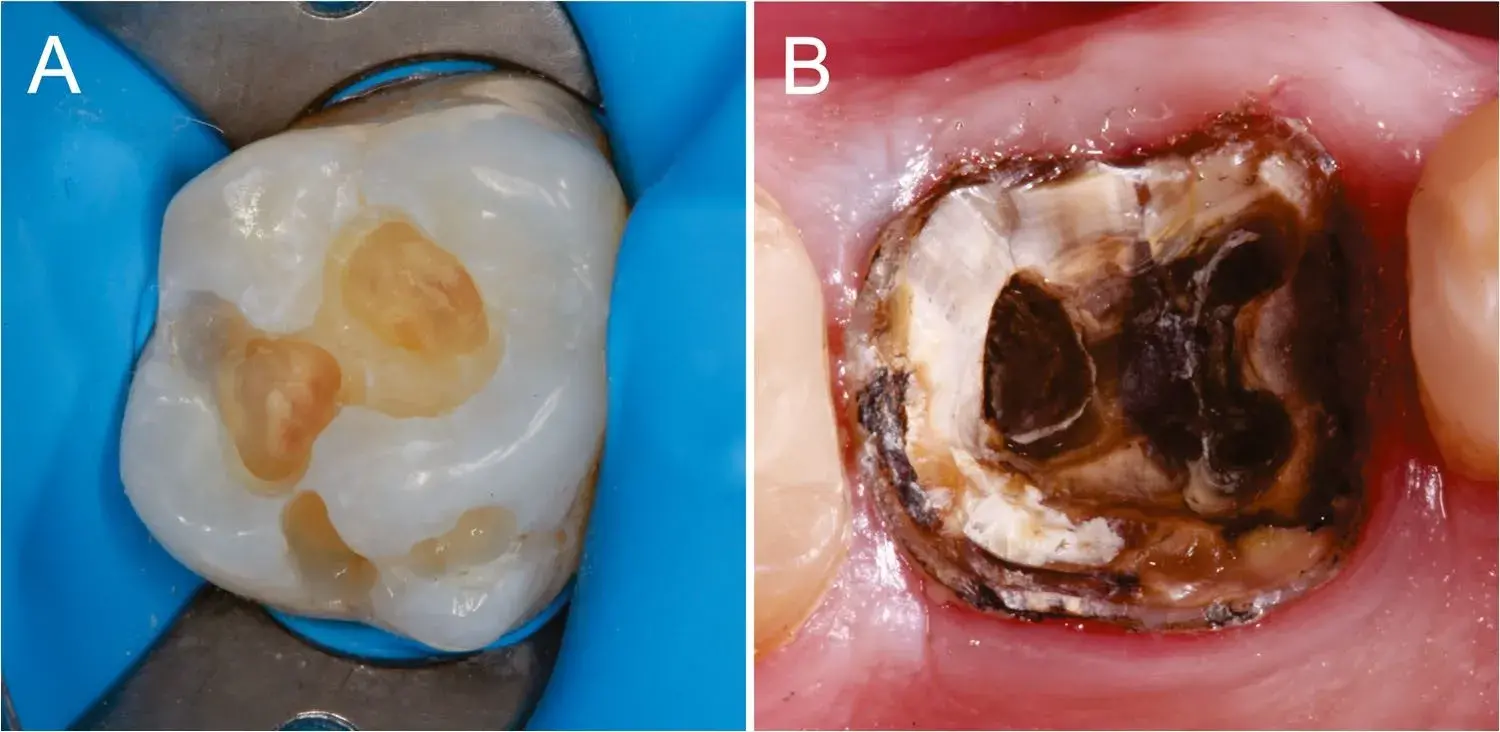 Fig. 1 Two distinctive tooth cavities that will impose diferent challenges to the clinical restorative procedures and longevity of restorations. The reasons why case B is more challenging than A are addressed in the text. Images from Dr. José R. Moura, Brazil
Fig. 1 Two distinctive tooth cavities that will impose diferent challenges to the clinical restorative procedures and longevity of restorations. The reasons why case B is more challenging than A are addressed in the text. Images from Dr. José R. Moura, Brazil
Patient’s Risks: the Context
Previous investigations [12, 28, 29] have been corroborated by recent studies showing that several patient-related factors were associated with failure of anterior and posterior restorations. These aspects include patients’ sex, age, and socioeconomic variables, in addition to oral health-related variables such as oral hygiene, parafunctional habits, caries risk, and caries experience during the course of life [5, 9, 11, 13, 14, 30, 31]. Restorations in male patients have been reported to have shorter survival in the long term than those in female patients [9, 13], which may be related to higher levels of oral hygiene and lower occlusal forces in females.
Diferent studies have reported higher restoration failure rates in adolescent and elderly patients [5, 11, 13, 31], a result likely to be related to a higher degree of caries activity in these age groups. Socioeconomic deprivation and age factors impacted the survival of posterior composite restorations in a primary care dental outreach center [32], fndings that could also be associated with increased caries risk. Occlusal stress related to bruxism decreased the survival of restorations in a retrospective study conducted in a period of up to 13 years [22]. A practice-based study showed that 78% of Class II resin composite restorations in patients at high risk for caries were indeed placed due to caries, in contrast with only 46% due to fracture or wear in patients with parafunctional habits as their main risk [11]. The same study showed that restorations placed due to fracture were more prone to fail than restorations placed due to caries [11]. This result could be associated with structural fatigue and warrants further investigation. In addition, new restoration placement due to caries and endodontic treatment were the most common interventions after 3 years of service [11]. When one risk factor is combined with another (e.g., high occlusal forces and caries activity), the risk for failure increases [11, 28].
Recent studies have observed other patient-related aspects that may be associated with restoration longevity, adding higher complexity to the contextual scenario. Deep periodontal pockets were associated with increased risk of restoration failures [33]. In a practice-based study, medically compromised patients and patients with periodontal disease were more susceptible to restoration failures [11••]. A clinical study conducted in a period of up to 15 years showed that missing teeth and proximal contacts were associated with lower restoration survival [20]. In corroboration, the number of teeth in the dentition was reported to be a protection factor for the survival of ETT [33]. In contrast, the presence of partial or full removable dentures could compromise the survival of restorations [11].
A retrospective study showed that the survival of restorations and teeth, especially those restored with large composites, was shortened in patients with dry mouth [34], which is also a risk factor for caries. Higher anterior tooth wear scores were associated with an increased risk for failures in anterior restorations [35]. Head and neck radiotherapy has also been found to have a negative impact on the longevity of adhesive restorations [36]. Many of the risk factors addressed herein are indirectly related to the survival of composite restorations, which are more prone to failures in an aggressive oral environment. The presence of a partial denture, for example, indicates that the patient has experienced tooth loss in the past. Tooth loss is likely to be related to higher caries and periodontal risks. In addition, secondary caries being one of the main reasons leading to restoration failures indicate that bioflms may also afect the clinical durability of resin composites. An in vitro study observed that depending on their composition, oral bioflms may degrade the surface topography of composites by the action of bacterial esterases, although the surface changes did not appear to afect further bioflm accumulation [37].
A literature review reported that the development of secondary caries around resin composite restorations was to some extent associated with the restorative material, but failed to identify material properties involved in the development of new caries lesions around restorations [38].
Dentists and Their Clinical Decisions
Restored teeth may be considered the result of a collection of choices made by patients and those of their dentists, who assessed their teeth and restorations over time. The question of how long a restoration should last is ubiquitous in clinical ofces; however, it is also difcult to answer.
In fact, only dentists themselves could assess the average durability of the restorations they place. Consider the fgures given in Table 1 to illustrate how variation in success rates among professionals may lead to diferent durability scenarios. The percentages in this example were the minima and maxima AFRs reported among 47 dentists in a practice-based study with anterior resin composite restorations [6••].
In the case of Dentist A, if patients receive the indication that their restorations could last 5 or 10 years, the estimation would be correct for at least 80% of cases. In contrast, the same predictions made by Dentist would represent an overestimation of longevity because 45% of restorations would fail after 5 years and approximately 70% of restorations after 10 years. Several underlying aspects could be associated with those distinct failure rates, such as the previously discussed tooth-related aspects and patient-related characteristics, including esthetical demands that may vary across countries and even between practices located in areas with diferent socioeconomic realities. Professional decisions relative to whether or not to intervene in aged restorations may be decisive for their clinical durability. Success and survival rates will be lower should a dentist decide to repair or replace composite restorations due to minor problems such as marginal staining, gaps, chipping, or wear, for instance [39]. In a retrospective study conducted in a period of up to 18.5 years, restorations that were submitted to more frequent check-ups per year showed higher failure rates than those with fewer check-ups, and diferent dentists assessing the restorations signifcantly infuenced the time until failure [31].
Several studies corroborated the fndings that there were substantial variations in restoration failure rates among practitioners [5, 6, 13, 20]. In one study, among 22 dentists, the AFRs of restorations ranged between 3.6 and 11.7% [11], whereas another article reported that restorations placed by one dentist only or in small practices, lasted longer than those in practices with more than 3 dentists [5]. Other professional aspects that may infuence the durability of restorations have recently been addressed in clinical studies. Higher AFRs were observed for restorations placed by less experienced dentists, i.e., those with fewer years since graduation [5]. A 17% higher risk for anterior restoration failure was observed when more than one dentist performed restorative treatments in the same patient [6]. Restorations placed in a practice located in an area with low socioeconomic status were reported to have higher AFRs [5]. In a multicenter study, anterior resin composite restorations were judged diferently relative to maintenance, repair, or replacement depending on the dentists who evaluated the restorations [40]. However, a large retrospective study reported that dentists’ gender played no role in the long-term survival of composites [9].
In general, a possible explanation for the relatively large diference in AFRs observed for resin composite restorations placed by diferent dentists is related to their clinical decisions to intervene in aged restorations, or not, resulting in behaviors we here defne as being “proactive” or “reactive” attitudes. A proactive dentist will decide to replace or repair a restoration with a minor defect, such as marginal discoloration or a small chipping fracture, or even to replace a restoration to prevent a possible cusp fracture in the future.
In contrast, a reactive dentist will only decide to intervene in restorations when signifcant clinical problems such as cavitated caries lesions, pain, broken cusps, or esthetic demands from patients are clearly present, and monitoring only is not an option. A proactive attitude when dealing with aged restorations will most certainly lead to more interventions and shorter longevity of restorations when compared with dentists who have a reactive, more conservative approach.
In addition, the proactive dentist cannot guarantee that the new restoration will look better in the future or even last longer than the restoration that will be replaced.
Table 1 Comparison of the clinical durability between restorations placed by two given dentists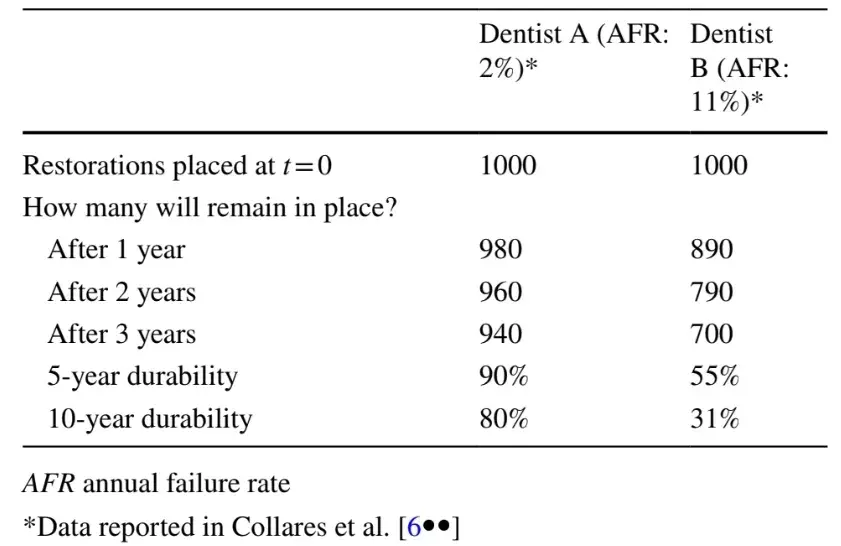
Material and Technical‑Related Aspects
Challenges to the clinical performance of resin composite restorations may also involve material and technical aspects. Comparisons between composites are still frequently made in clinical studies but seldom lead to signifcant diferences between brands and types of materials. For example, a split-mouth, randomized trial with a 14-year period of follow-up showed that two packable composites showed a clinical performance that was similar to that of a resin composite with regular viscosity [41]. In another study with follow-up period of 13 years, composites for anterior restorations were divided into two categories, i.e., materials with multiple shades, developed for esthetic indications, and universal materials that could be used for both posterior and anterior teeth [6]. No signifcant diferences in clinical performance were observed between the two types of composites. In contrast, Class II restorations with a highly-flled microhybrid composite showed the lowest risk for failure in a practice-based study [11]. In addition, dental material manufacturers often release updated versions of their products, usually claiming improved performance. However, in a recent split-mouth, double-blinded trial, no signifcant diference in the clinical behavior of posterior restorations after 5 years was observed between an “old” resin composite formulation and its successor material [42].
A more or less recent material development was the introduction of bulk-fll composites that allowed larger increments to fll cavities. A randomized controlled trial concluded that using a bulk-fll composite, presented in capsules or syringes, was less time consuming and did not change the risk or intensity of 1-week postoperative sensitivity than a traditional incremental technique [43].
A randomized trial comparing bulk-fll and conventional composites in Class II restorations after 6 years reported no signifcant diferences for the majority of clinical criteria evaluated, except for a better performance of the bulk-fll in marginal discoloration [44]. A network meta-analysis on directly placed restorations suggested that etch-and-rinse adhesives combined with conventional composite could be preferable in permanent teeth [45].
This result was in line with those from another study reporting better performance for restorations bonded with 3-step etch-and-rinse than self-etch adhesives [11]. In contrast, another network meta-analysis of adhesive strategies for cervical restorations concluded that no strategy was better than any other in terms of restoration retention [46]. In fact, the authors discouraged clinicians, researchers, and teachers from labeling the efcacy of adhesives based on their bonding strategy. However, most randomized trials included in both network meta-analyses [45, 46] had high or unclear risks of bias, reducing the certainty of evidence. The observation of high risk of bias in clinical trials is a contemporary commonplace feature in healthcare metascience. Therefore, better research and reporting practices are urgently required to improve reproducibility and reduce uncertainty in evidence and knowledge syntheses.
In vitro studies evaluating diferent physical–mechanical properties of resin composites are abundant in the literature, e.g., assessing their fexural strength, elastic modulus, microhardness, and compressive strength. Laboratorial studies observing diferences among restorative materials and techniques commonly suggest that these diferences could be relevant to the clinical performance of restorations. Examples may include diferent cavity preparation designs, inactivation of dentin metalloproteinases during bonding steps, variations in incremental flling techniques, or light polymerization strategies.
However, the evidence for the mentioned relevance is seldom presented or established in clinical studies. A systematic review evaluated varied mechanical parameters of resin composites and compared the data to outcomes reported for the same materials in clinical trials [47]. Moderately positive correlations between clinical and laboratory outcomes were observed, with fracture toughness being mostly correlated with clinical fractures and fexural strength with clinical wear. However, the high risk of bias in the original studies was again an issue raised by the authors. Prospective clinical studies investigating variables related to dental composites and restorative techniques generally show overall good performance and no signifcant efect for the variables tested, often due to short follow-up times or lack of power, which could be related to the high costs involved in these studies [48]. Most materials perform well, especially in the short term, and factors related to patients and operators addressed in previous chapters play leading roles in the clinical behavior of resin composites. The infuence of light polymerization on the clinical performance of resin composite restorations has not been sufficiently explored in the current literature.
Studies on the use of composites for the rehabilitation of patients with tooth wear are more prevalent in recent literature and have the advantage that high-risk patients are included, leading to more expected failures and a higher chance to observe diferences in primary outcomes. A randomized trial with patients presenting moderate to severe tooth wear restored with resin composites showed poorer performance for indirect compared to direct materials after 3.5 years [49]. A recent clinical trial with patients with severe tooth wear followed up for 5 years observed that different composites showed distinct behaviors: a nanoflled showed less wear in load-bearing cusps, whereas a microhybrid showed less wear in non-bearing cusps and anterior maxillary teeth [21]. Another study reported that increased vertical dimension of occlusion was associated with a lower risk of failure in anterior but not in posterior restorations in patients with tooth wear [35]. The authors suggested that if possible, direct composite restorations performed in these patients should be made as voluminous as possible.
Concerning isolation of the operative feld, a 2012 review reported that restorations placed with rubber dam isolation showed the best performance in clinical studies [50], but failed to address the question of studies without rubber dam isolation were likely to include more high-risk patients than those using rubber dam. A more recent systematic review suggested that the use of rubber dam in direct restorative treatments may lead to a lower failure rate of restorations than isolation using cotton rolls only in the frst 6 months, whereas the evidence was uncertain for longer clinical service times [51]. Another aspect that has been revisited in recent literature is the use of liners in deep restorations. In a meta-analysis, a calcium hydroxide lining did not infuence the clinical performance of restorations placed in deep caries lesions [52]. This fnding agrees with those from a critical article addressing the importance of continuing education for dentists, highlighting that not everything dental students are taught, even if state of the art at the time, should remain valid throughout a professional lifetime [53]. Another topic that appears to have room for further long-term clinical investigation is the comparison between direct and indirect composites. A network meta-analysis on treatment options for large posterior restorations observed that indirect materials generally performed better, but direct composites were also feasible for teeth with large structure losses [54].
Clinical Signs of Restoration Aging
We understand that in dentistry, it is time to eliminate the idea that performing procedures on restorations, such as sealing margins or repairing minor defects, is always benefcial.
In several cases, doing nothing may be the best approach to increase the longevity of restorations [12, 55, 56]. Consider the images presented in Fig. 2. During the clinical service of restorations, the challenges imposed by the oral environment will leave marks on the restorative materials. Surface and marginal staining may occur, in addition to the loss of anatomical shape and translucency, wear, chipping fractures, and other minor defects. A long-term multicenter trial with direct anterior resin composite restorations reported that chipping was a frequent clinical fnding [57]. Aging signs are likely to appear sooner or later. Note that all imperfections observed in an intermediate analysis in Fig. 2 did not progress in later images, meaning that any intervention would have been premature and mostly unnecessary. Aging defects will not necessarily lead to the replacement of a flling in the future. Ultimately, replacing restorations due to minor blemishes will not prevent real problems such as new caries lesions or tooth fractures.
A scenario in which restorations show even greater signs of clinical aging is presented in Fig. 3. These restorations, photographed in 2020, were placed between 1986 and 1992 using restorative materials and techniques that were state of the art at the time. Marginal staining, generalized wear, loss of anatomical shape, discoloration, and marginal breakdown are among the possible defects that any dentist could observe in the photographs. Would those restorations last as long as they did if the dentist had been proactive and decided to intervene earlier? Another aspect visible in Fig. 3 is the presence of restoration repairs, a minimally invasive procedure that has been shown to positively infuence durability [12, 58–60]. A clinical study conducted over a period of 12 years reported that repair should be seen as a good clinical option because it consistently increased the longevity of posterior restorations [58]. Corroborating this fnding, another clinical study with a 15-year period of follow-up observed that the repair could improve the survival of Class III, Class IV, and veneer resin composite restorations [59]. A practice-based study with 24 dentists and almost 22 thousand patients reported that repairs increased the survival of restorations and that there was substantial variation in the frequency of repair among the professionals [60].
We have sufcient evidence to claim that aged restorations should be left untouched as far as possible, even when signs of aging are present. Clinicians should always consider monitoring restorations to be the best option for extending the longevity of teeth and restorations. When a clear sign of failure is shown and intervention is needed, restorations should preferably be repaired rather than replaced. Clear signs of failure involve fractures, cavitated lesions, pain, and patient demands, including esthetic issues and wear. Radiographic examination of restorations should not be routine and should be seen as a complementary analysis. In a recent randomized clinical trial with preschool children, the use of radiographs in the diagnostic strategy for caries detection led to the occurrence of false-positive results, overdiagnosis, and lead-time bias [61].
 Fig. 2 Resin composite restorations photographed immediately after being prepared (baseline) and clinical images captured in further appointments up to 27 years later. The challenges imposed by the oral environment left their marks on restorations (arrows). The aging signs may appear sooner or later. Note that the imperfections observed in an intermediate analysis did not progress in the later pictures to justify intervention. Cases by Dr. José R. Moura
Fig. 2 Resin composite restorations photographed immediately after being prepared (baseline) and clinical images captured in further appointments up to 27 years later. The challenges imposed by the oral environment left their marks on restorations (arrows). The aging signs may appear sooner or later. Note that the imperfections observed in an intermediate analysis did not progress in the later pictures to justify intervention. Cases by Dr. José R. Moura
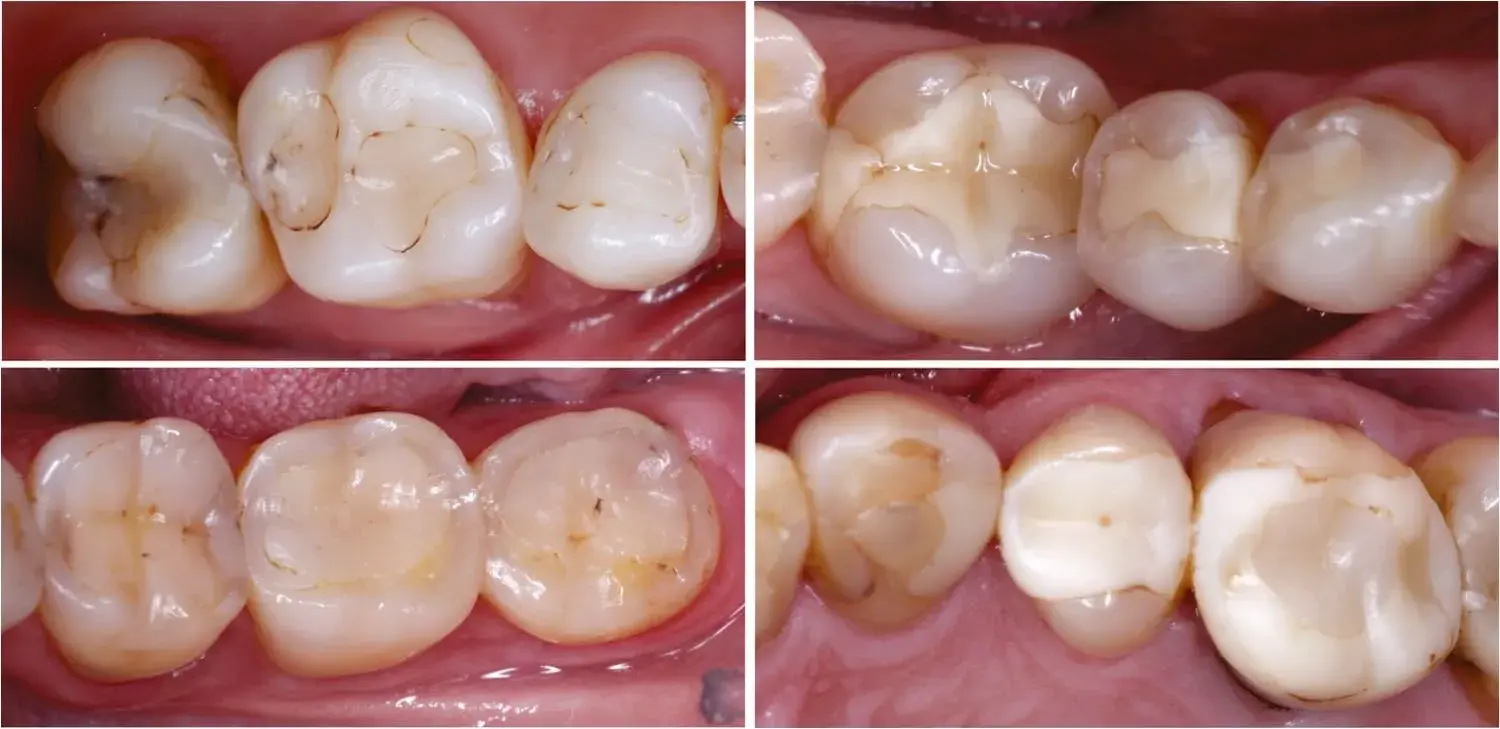 Fig. 3 Restorations with signs of clinical aging after 29–33 years in service. Marginal staining, wear, loss of anatomical shape, discoloration, and marginal breakdown are visible, but the restorations function well, and patients had no complaints. Some restorations were repaired during the follow-up period. Cases by Dr. Paullo da Rosa Rodolpho, Brazil
Fig. 3 Restorations with signs of clinical aging after 29–33 years in service. Marginal staining, wear, loss of anatomical shape, discoloration, and marginal breakdown are visible, but the restorations function well, and patients had no complaints. Some restorations were repaired during the follow-up period. Cases by Dr. Paullo da Rosa Rodolpho, Brazil
Conclusions
The clinical service of resin composite restorations is a challenging aspect for their longevity, but posterior and anterior composites can present long-lasting clinical durability.
Among the several variables that may be associated with the clinical failure of restorations, patient-related risks appear to be the most predominant factors for the overall longevity of resin composites, as has been supported by clinical studies. Dentists and their decisions may also play signifcant roles in the clinical performance of restorations. However, decision-making, professional practices, and the infuence of operator skills on the durability of restorations are topics still relatively seldom explored in research studies. State of the art restorative techniques and materials have limited infuence on the durability of resin composite restorations. In general, the longevity of restorations would be longer if dentists were to use a more conservative approach when dealing with aging restorations and avoided overtreatment by respecting the aged appearance of restorations in service.
There are additional details about direct restorations that you can gain on our website.
Authors:
Rafael R. Moraes, Maximiliano S. Cenci, José R. Moura, Flavio F. Demarco, Bas Loomans, Niek Opdam
References
Worthington HV, Khangura S, Seal K, Mierzwinski-Urban M, Veitz-Keenan A, Sahrmann P, et al. Direct composite resin fllings versus amalgam fllings for permanent posterior teeth. Cochrane Database Syst Rev. 2021;8:CD005620.
Da Rosa Rodolpho PA, Donassollo TA, Cenci MS, Loguércio AD, Moraes RR, Bronkhorst EM, et al. 22-Year clinical evaluation of the performance of two posterior composites with different fller characteristics. Dent Mater. 2011;27:955–63.
Pallesen U, van Dijken J. A randomized controlled 27 years follow up of three resin composites in class II restorations. J Dent. 2015;43:1547–58.
Pallesen U, van Dijken J. A randomized controlled 30 years follow up of three conventional resin composites in class II restorations. Dent Mater. 2015;31:1232–44.
Laske M, Opdam NJ, Bronkhorst EM, Braspenning JC, Huysmans MC. Longevity of direct restorations in Dutch dental practices. Descriptive study out of a practice based research network. J Dent. 2016;46:12–7.
Collares K, Opdam NJ, Laske M, Bronkhorst EM, Demarco FF, Correa MB, et al. Longevity of anterior composite restorations in a general dental practice-based network. J Dent Res. 2017;96:1092–9.
Montag R, Dietz W, Nietzsche S, Lang T, Weich K, Sigusch BW, et al. Clinical and micromorphologic 29-year results of posterior composite restorations. J Dent Res. 2018;97:1431–7.
Baldissera RA, Corrêa MB, Schuch HS, Collares K, Nascimento GG, Jardim PS, et al. Are there universal restorative composites for anterior and posterior teeth? J Dent. 2013;41:1027–35.
Burke FJ, Lucarotti PS. The ultimate guide to restoration longevity in England and Wales. Part 4: resin composite restorations: time to next intervention and to extraction of the restored tooth. Br Dent J. 2018;224:945–6.
Burke FJ, Lucarotti PS. The ultimate guide to restoration longevity in England and Wales. Part 10: key fndings from a ten million restoration dataset. Br Dent J. 2018;225:1011–8.
This study analyzed a large dataset of restorations and reported that the patient treatment history is one of the main factors afecting longevity.
Laske M, Opdam NJ, Bronkhorst EM, Braspenning JCC, Huysmans MC. Risk factors for dental restoration survival: a practice-based study. J Dent Res. 2019;98:414–22.
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87–101. https://doi.org/10.1016/j.dental.2011.09.003. This classic review article explored several factors other than material-related variables that may afect the clinical performance of posterior resin composite restorations.
Laske M, Opdam NJ, Bronkhorst EM, Braspenning JC, Huysmans MC. Ten-year survival of class ii restorations placed by general practitioners. JDR Clin Trans Res. 2016;1:292–9.
Montagner AF, Sande FHV, Müller C, Cenci MS, Susin AH. Survival, reasons for failure and clinical characteristics of anterior/posterior composites: 8-year fndings. Braz Dent J. 2018;29:547–54.
Fan J, Xu Y, Si L, Li X, Fu B, Hannig M. Long-term clinical performance of composite resin or ceramic inlays, onlays, and overlays: a systematic review and meta-analysis. Oper Dent. 2021;46:25–44.
Kang SH, Kim BS, Kim Y. Cracked teeth: Distribution, characteristics, and survival after root canal treatment. J Endod. 2016;42:557–62.
Nuamwisudhi P, Jearanaiphaisarn T. Oral functional behaviors and tooth factors associated with cracked teeth in asymptomatic patients. J Endod. 2021;47:1383–90.
Kuper NK, Opdam NJ, Bronkhorst EM, Huysmans MC. The infuence of approximal restoration extension on the development of secondary caries. J Dent. 2012;40:241–7.
Van Meerbeek B, Yoshihara K, Van Landuyt K, Yoshida Y, Peumans M. From Buonocore’s pioneering acid-etch technique to self-adhering restoratives. A status perspective of rapidly advancing dental adhesive technology. J Adhes Dent. 2020;22:7–34.
Linnemann T, Kramer EJ, Schwendicke F, Wolf TG, Meyer-Lueckel H, Wierichs RJ. Longevity and risk factors of post restorations after up to 15 years: a practice-based study. J Endod. 2021;47:577–84.
Ning K, Bronkhorst E, Bremers A, Bronkhorst H, van der Meer W, Yang F, et al. Wear behavior of a microhybrid composite vs. a nanocomposite in the treatment of severe tooth wear patients: a 5-year clinical study. Dent Mater. 2021;37:1819–27.
Lempel E, Lovász BV, Bihari E, Krajczár K, Jeges S, Tóth Á, et al. Long-term clinical evaluation of direct resin composite restorations in vital vs. endodontically treated posterior teeth — retrospective study up to 13 years. Dent Mater. 2019;35:1308–18.
Pontoriero DI, Grandini S, Spagnuolo G, Discepoli N, Benedicenti S, Maccagnola V, et al. Clinical outcomes of endodontic treatments and restorations with and without posts up to 18 years. J Clin Med. 2021;10:908.
Girotto LP, Dotto L, Pereira GK, Bacchi A, Sarkis-Onofre R. Restorative preferences and choices of dentists and students for restoring endodontically treated teeth: a systematic review of survey studies. J Prosthet Dent. 2021;126:489.e5.
Naumann M, Schmitter M, Frankenberger R, Krastl G. “Ferrule comes frst. Post is second!” Fake news and alternative facts? A systematic review. J Endod. 2018;44:212–9.
Wierichs RJ, Kramer EJ, Wolf TG, Naumann M, Meyer-Lueckel H. Longevity of composite build-ups without posts—10-year results of a practice-based study. Clin Oral Investig. 2019;23:1435–42.
Schwendicke F, Kramer EJ, Krois J, Meyer-Lueckel H, Wierichs RJ. Long-term costs of post-restorations: 7-year practice-based results from Germany. Clin Oral Investig. 2021;25:2175–81.
van de Sande FH, Opdam NJ, Rodolpho PA, Correa MB, Demarco FF, Cenci MS. Patient risk factors’ infuence on survival of posterior composites. J Dent Res. 2013;92:78S-83S.
Demarco FF, Collares K, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Should my composite restorations last forever? Why are they failing? Braz Oral Res. 2017;31:e56.
Collares K, Opdam NJ, Peres KG, Peres MA, Horta BL, Demarco FF, et al. Higher experience of caries and lower income trajectory infuence the quality of restorations: a multilevel analysis in a birth cohort. J Dent. 2018;68:79–84.
Wierichs RJ, Kramer EJ, Meyer-Lueckel H. Risk factors for failure of direct restorations in general dental practices. J Dent Res. 2020;99:1039–46.
This long-term, multicenter study showed that restorations submitted to more frequent check-ups per year showed higher failure rates than those with fewer check-ups.
Wong C, Blum IR, Louca C, Sparrius M, Wanyonyi K. A retrospective clinical study on the survival of posterior composite restorations in a primary care dental outreach setting over 11 years. J Dent. 2021;106:103586.
Skupien JA, Opdam NJ, Winnen R, Bronkhorst EM, Kreulen CM, Pereira-Cenci T, et al. Survival of restored endodontically treated teeth in relation to periodontal status. Braz Dent J. 2016;27:37–40.
Jukka L, Hannu V, Ellinoora R, Laura J, Ritva N, Vuokko A. The survival time of restorations is shortened in patients with dry mouth. J Dent. 2021;113:103794.
Mehta SB, Bronkhorst EM, Lima VP, Crins L, Bronkhorst H, Opdam NJ, et al. The efect of pre-treatment levels of tooth wear and the applied increase in the vertical dimension of occlusion (VDO) on the survival of direct resin composite restorations. J Dent. 2021;111:103712.
Palmier NR, Madrid Troconis CC, Normando AG, Guerra EN, Araújo AL, Arboleda LP, et al. Impact of head and neck radiotherapy on the longevity of dental adhesive restorations: a systematic review and meta-analysis. J Prosthet Dent. 2021.
Nedeljkovic I, De Munck J, Ungureanu AA, Slomka V, Bartic C, Vananroye A, et al. Bioflm-induced changes to the composite surface. J Dent. 2017;63:36–43.
Nedeljkovic I, Teughels W, De Munck J, Van Meerbeek B, Van Landuyt KL. Is secondary caries with composites a material-based problem? Dent Mater. 2015;31:e247–77.
Moro BL, Freitas RD, Pontes LR, Passaro AL, Lenzi TL, Tedesco TK, et al. Infuence of diferent clinical criteria on the decision to replace restorations in primary teeth. J Dent. 2020;101:103421.
Freitas BN, Pintado-Palomino K, de Almeida CV, Cruvinel PB, Souza-Gabriel AE, Corona SA, et al. Clinical decision-making in anterior resin composite restorations: a multicenter evaluation. J Dent. 2021;113:103757.
Espíndola-Castro LF, Guimarães RP, Souza FB, Monteiro GQ, Menezes Filho PF, Fernandes LO, et al. A 14-year follow-up of resin composite occlusal restorations: split mouth randomised clinical trial and wear evaluation by optical coherence tomography. J Clin Diagnostic Res. 2019;13:ZC10-15.
Gurgan S, Koc Vural U, Kutuk ZB, Cakir FY. Does a new formula have an input in the clinical success of posterior composite restorations? A chat study. Clin Oral Investig. 2021;25:1715–27.
Tardem C, Albuquerque EG, Lopes LS, Marins SS, Calazans FS, Poubel LA, et al. Clinical time and postoperative sensitivity after use of bulk-fll (syringe and capsule) vs. incremental flling composites: a randomized clinical trial. Braz Oral Res. 2019;33:e089.
Yazici AR, Kutuk ZB, Ergin E, Karahan S, Antonson SA. Six-year clinical evaluation of bulk-fll and nanofll resin composite restorations. Clin Oral Investig. 2021.
Schwendicke F, Göstemeyer G, Blunck U, Paris S, Hsu LY, Tu YK. Directly placed restorative materials: review and network meta-analysis. J Dent Res. 2016;95:613–22.
Dreweck FD, Burey A, de Oliveira DM, Loguercio AD, Reis A. Adhesive strategies in cervical lesions: systematic review and a network meta-analysis of randomized controlled trials. Clin Oral Investig. 2021;25:2495–510.
Heintze SD, Ilie N, Hickel R, Reis A, Loguercio A, Rousson V. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials-a systematic review. Dent Mater. 2017;33:e101–14.
Opdam NJ, Collares K, Hickel R, Bayne SC, Loomans BA, Cenci MS, et al. Clinical studies in restorative dentistry: new directions and new demands. Dent Mater. 2018;34:1–12.
Crins LA, Opdam NJ, Kreulen CM, Bronkhorst EM, Sterenborg BA, Huysmans MC, et al. Randomized controlled trial on the performance of direct and indirect composite restorations in patients with severe tooth wear. Dent Mater. 2021;37:1645–54.
Heintze SD, Rousson V. Clinical efectiveness of direct class II restorations - a meta-analysis. J Adhes Dent. 2012;14:407–31.
Miao C, Yang X, Wong MC, Zou J, Zhou X, Li C, Wang Y. Rubber dam isolation for restorative treatment in dental patients. Cochrane Database Syst Rev. 2021;5:CD009858.
da Rosa WL, Lima VP, Moraes RR, Piva E, da Silva AF. Is a calcium hydroxide liner necessary in the treatment of deep caries lesions? A systematic review and meta-analysis. Int Endod J. 2019;52:588–603.
Blum IR, Wilson NH. An end to linings under posterior composites? J Am Dent Assoc. 2018;149:209–13.
Vetromilla BM, Opdam NJ, Leida FL, Sarkis-Onofre R, Demarco FF, van der Loo MP, et al. Treatment options for large posterior restorations: a systematic review and network meta-analysis. J Am Dent Assoc. 2020;151:614-24.e18.
Estay J, Martin J, Vildósola P, Villablanca C, Mjör I, de Oliveira Jr OB, et al. Sealing of restorations with marginal defects does not afect their longevity. Am J Dent. 2018;31:107–12.
Fernández E, Vildósola P, Bersezio C, Gordan VV, Mjör IA, Oliveira OB, et al. Does refurbishing composites lead to short-term efects or long-lasting improvement? Am J Dent. 2015;28:203–8.
Frese C, Wohlrab T, Soliman S, Hahn B, Büsch C, Babai A, et al. A multicenter trial on the long-term performance of direct composite buildups in the anterior dentition - survival and quality outcome. J Adhes Dent. 2020;22:573–80.
Estay J, Martín J, Viera V, Valdivieso J, Bersezio C, Vildosola P, et al. 12 Years of repair of amalgam and composite resins: a clinical study. Oper Dent. 2018;43:12–21.
van de Sande FH, Moraes RR, Elias RV, Montagner AF, Rodolpho PA, Demarco FF, et al. Is composite repair suitable for anterior restorations? A long-term practice-based clinical study. Clin Oral Investig. 2019;23:2795–803.
Casagrande L, Laske M, Bronkhorst EM, Huysmans MC, Opdam NJ. Repair may increase survival of direct posterior restorations – a practice based study. J Dent. 2017;64:30–6.
Pontes LR, Lara JS, Novaes TF, Freitas JG, Gimenez T, Moro BL, et al. Negligible therapeutic impact, false-positives, over-diagnosis and lead-time are the reasons why radiographs bring more harm than benefts in the caries diagnosis of preschool children. BMC Oral Health. 2021;21:168.


