Arthrocentesis with or without additional drugs in temporomandibular joint inflammatory-degenerative disease: comparison of six treatment protocols
SUMMARY
The aim of the present pilot investigation was to compare the effectiveness of six treatment protocols providing temporomandibular joint (TMJ) arthrocentesis with or without additional drugs to manage symptoms in patients with inflammatory-degenerative TMJ disease. A consecutive series of 72 patients with TMJ osteoarthritis (axis group IIIb) with pain lasting from more than 6 months were randomly assigned to one of the groups receiving the following treatment protocols: single-session two-needle arthrocentesis (A), single-session two-needle arthrocentesis plus corticosteroid (B), single-session two-needle arthrocentesis plus low molecular weight hyaluronic acid (HA) (C), single-session two-needle arthrocentesis plus high molecular weight HA (D), 5 weekly two-needle arthrocenteses plus low molecular weight HA (E) and 5 weekly single-needle arthrocenteses plus low molecular weight HA (F). At the 3-month follow-up, improvement with respect to mean baseline values was recorded in all the five treatment groups completing the protocol. No significant differences emerged between groups in any outcome variable. The protocol providing five sessions of two-needle arthrocenteses plus low molecular weight HA allowed achieving the highest improvement in almost all the outcome variables. Findings suggested that no statistically significant differences existed between the treatment groups. The clinical significance of these findings needs to be tested with future studies on larger samples with longer follow-up periods.
You have the opportunity to gather more in-depth information about temporomandibular disorders diagnosis and treatment in our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
INTRODUCTION
Literature data suggested that arthrocentesis may be of some benefit to manage symptoms of temporomandib- ular joint (TMJ) disorders, even though findings are not conclusive as for the potential additional effectiveness achieved with drugs injected immediately following joint lavage (1, 2).
The first works on TMJ arthrocentesis focused on its application to increase jaw function and achieve relief from pain in patients with restricted mouth opening (3, 4). Then, with the increase in knowledge on the role of joint lubrication impairment as a risk factor for TMJ internal derangements, viscosupplementation with sodium hyaluronate, viz., hyaluronic acid (HA), became an option for the management of symptoms in the clinical setting (5). This led to the progressive expansion of potential clinical indications for the use of arthrocentesis plus HA injections, with particular regard to joints with inflammatory-degenerative disorders (6, 7). Protocols for symptoms management in larger joints provided the adoption of a cycle of 5 weekly HA injections immediately following arthrocentesis (8, 9), and encouraging findings emerged also from long-term case series on patients with TMJ disorders (10, 11).
Positive outcomes have also been described after TMJ injections with corticosteroid (12) and also with arthrocentesis alone (13), thus suggesting that definitive information on the most suitable protocol as concerns the number of injections, the ideal HA molecular weight and, more in general, on the most effective approach, viz., arthrocentesis alone or combined with drugs, is still lacking. In view of these considerations, in line with the need to perform exploratory trials on the issue, the aim of the present investigation was to compare the effectiveness of six treatment protocols providing TMJ arthrocentesis with or without additional drugs to manage symptoms in patients with inflammatory-degenerative TMJ disease.
MATHERIALS AND METHODS
A consecutive series of 72 patients with a Research Diagnostic Criteria for Temporomandibular Disorders (RDC ⁄ TMD) version 1.0 (14) diagnosis of osteoarthritis (axis I group IIIb) with joint pain lasting from more than 6 months seeking for treatment at the TMD Clinic, Department of Maxillofacial Surgery, University of Padova, Italy, were randomly assigned to one of the groups receiving the following treatment protocols: single-session two-needle arthrocentesis (A), single-session two-needle arthrocentesis plus corticosteroid (B), single-session two-needle arthrocentesis plus low molecular weight HA (C), single-session two-needle arthrocentesis plus high molecular weight HA (D), 5 weekly two-needle arthrocenteses plus low molecular weight HA (E) and 5 weekly single-needle arthrocenteses plus low molecular weight HA (F). Patients were instructed to have a 2-week wash-out period before starting the treatment protocol and to not use medications on routine basis during the active treatment and follow-up periods.
The two-needle techniques refer to the approach first described by Nitzan et al. (3), with a needle dedicated to the inflow of physiological saline into the upper joint compartment and a second needle for the outflow. The joint lavage was performed with at least 300 mL of saline (15). After joint lavage, patients of protocol B received additional 1-mL triamcinolone injection*, patients of protocols C, E and F received 1 mL low molecular weight HA†, and the patients of protocol D received 1 mL high molecular weight hylauronic acid‡.
For protocols providing the injection of a drug after arthrocentesis, one needle was removed after joint lavage, and the remaining one was used to inject the drug into the joint space. The single-needle technique, first introduced by Guarda-Nardini et al. (16), adopted only one needle for both fluid injection and aspiration. Randomisation of patients between groups was achieved according to a [A-B-C-D-E-F-F-E-D-C-B-A] sequence for inclusion in the different groups. For each patient, a number of outcome parameters, viz., maximum pain at rest and maximum pain at chewing on a 10-point VAS scale with 0 being absence of pain and 10 being the worst pain ever, subjective chewing efficiency (0–10 VAS scale with 0 being the worst efficiency ever and 10 the best efficiency ever), treatment tolerability and perceived treatment effectiveness on a 5-point Likert-type scale with 0 being the lowest and 4 the maximum values, jaw range of motion function in millimetres, were assessed at baseline, at the end of treatment and at a 3-month follow-up. All interventions were conducted by one of the two main investigators (D.M.; L.G.N.) in accordance with the above-described random sequence of intervention, and the outcome parameters were recorded by the same trained dental student (D.R.) blinded to the treatment protocol for all patients. As far as practically possible, patients were blinded to the treatment modality; that is, a generic explanation of the potential benefit of administering arthrocentesis was provided as well as an explanation that the specific intervention they were undergoing was indicated for their disease. All patients gave their written consent after being informed on the study’s aims and design.
Power analysis based on literature data (11) and assuming a mean VAS value of 6 ⁄ 10 - 3 ⁄ 10 in the main outcome variable, viz., pain at chewing, revealed that the study design was able to detect a 57Æ1% between-group difference in mean pain at chewing VAS values with a statistical power of 5% for type I error, viz., false-positive results, and 20% for type II error, viz., false-negative results. VAS pain levels and jaw range of motion values were managed as continuous variables, while data on subjective efficacy and tolerability levels were managed as ordinal variables.
The existence of differences between groups as for percentage changes over time in all the outcome variables was assessed by means of analysis of variance (ANOVA) for continuous variables and Kruskal–Wallis’ test for ordinal variables. The percentage of patients of each group reporting an improvement was compared by Fisher’s exact test. Also, ANOVA and Fisher’s exact test were performed to investigate, respectively, for differences in the mean age and to compare sex distribution between groups. For all comparisons, statistical significance for between group differences was set at P < 0Æ05.
RESULTS
A total of 60 patients (mean age, 50Æ1 years; 51 women, nine men) completed the study. The treatment protocol D (arthrocentesis plus high molecular weight HA) was interrupted after five patients owing to the occurrence of unpleasant side effects, viz., joint swelling and strong post-injection increase in pain, in two of five subjects. So, the outcomes for such protocol were not described. No side effects were observed in any patients belonging to the other treatment groups. Five patients dropped out from the study owing to different reasons, mainly because of work related or other difficulties to attend the study sessions.
The number of patients completing treatment protocols A, B, C, E and F, ranged from 9 to 12 (protocol A: 11 patients; B: 9; C: 11; E: 12; F: 12), and no differences emerged between groups as for the mean age (P = 0Æ346) and sex distribution (P = 0Æ333). Baseline values of the five treatment groups were not significantly different in any of the outcome variables (P-values ranging from 0Æ471 to 0Æ702) (Table 1). At the 3-month follow-up, improvement with respect to mean baseline values was recorded in all the five treatment groups completing the protocol.
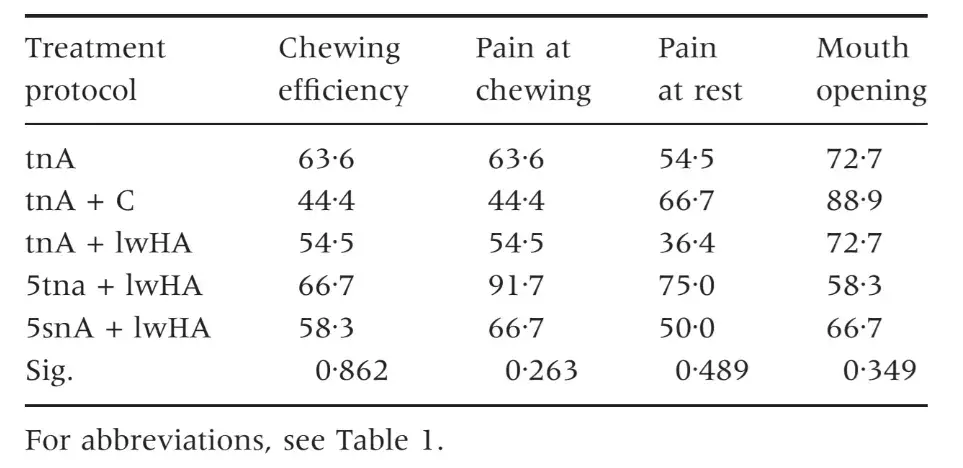
No significant differences emerged between groups in any outcome variable (P-values ranging from 0Æ056 to 0Æ989) (Table 2). Despite being not significant with respect to improvement achieved with other treatments, the protocol providing five sessions of two-needle arthrocenteses plus low molecular weight HA (protocol E) allowed achieving the highest improvement in almost all the outcome variables, among which maximum pain at chewing (64Æ9% decrease in VAS pain levels versus 11Æ5–41Æ3%; F = 1Æ727; P = 0Æ096). Protocol E was also the most tolerable by the patients (2Æ5 versus 2Æ1–2Æ2 on a four-point Likert-type ordinal scale; F = 0Æ299; P = 0Æ877), while protocol B, viz., arthrocentesis plus corticosteroids injection, endorsed the higher scores in subjectively perceived efficacy (3Æ0 versus 2Æ1–2Æ6; F = 0Æ753; P = 0Æ561) (Table 3). Differences between groups in the percentage of patients reporting an improvement in the outcome variables were not significant (P-values ranging from 0Æ263 to 0Æ862) (Table 4). The highest percentage of improvers in pain variables was shown in patients belonging to groups E (91Æ6%), F (66Æ6%) and C (63Æ6%), while groups receiving arthrocentesis alone (A) or with corticosteroids (B) had about a 50% percentage of patients who improved with respect to baseline pain values. Protocol E also had the highest percentage of patients referring an improvement in chewing efficiency (66Æ7%). Treatment protocol B included the highest percentage of subjects improving in mouth opening values (88Æ9%).
Table 1. Baseline values for the main outcome parameters. Comparison between the treatment groups (one-way ANOVA)
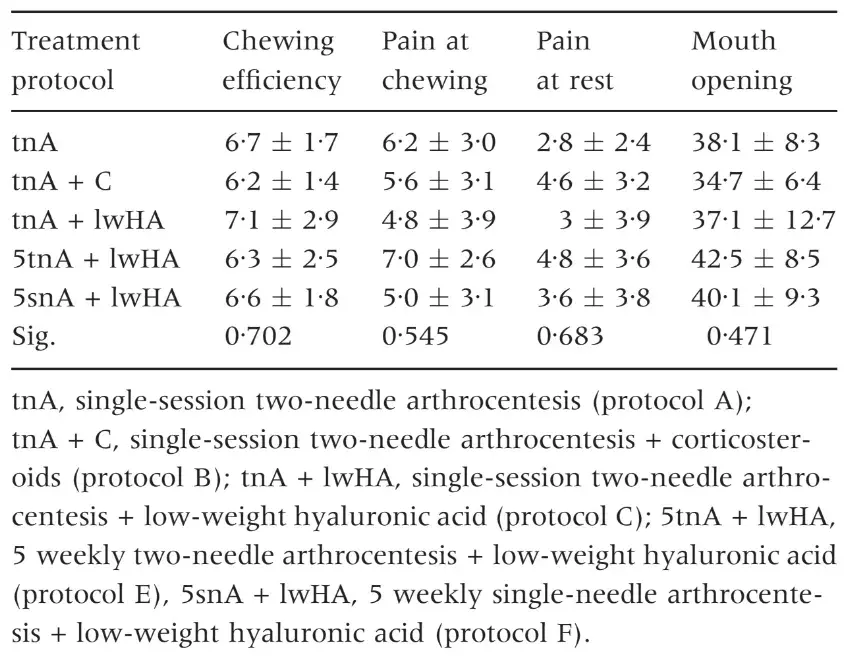
Table 2. Percentage changes at the end of the follow-up period with respect to baseline values. Comparison between the treatment groups (one-way ANOVA). In parentheses, the expected sign for improvement
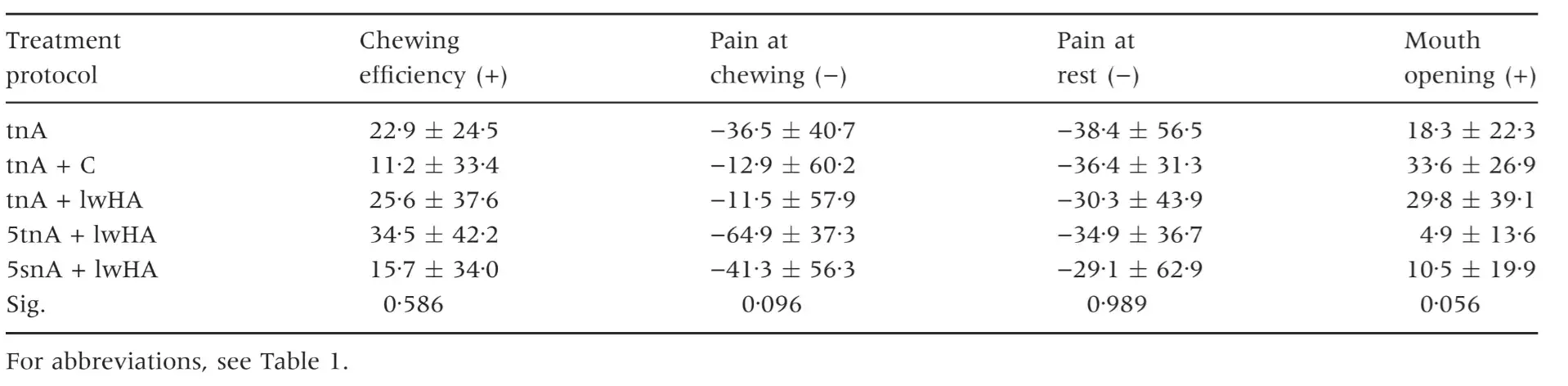
Table 3. Subjective efficacy and tolerability of the treatment on a 0–4 Likert scale. Comparison between the treatment groups (Kruskal–Wallis’ test)
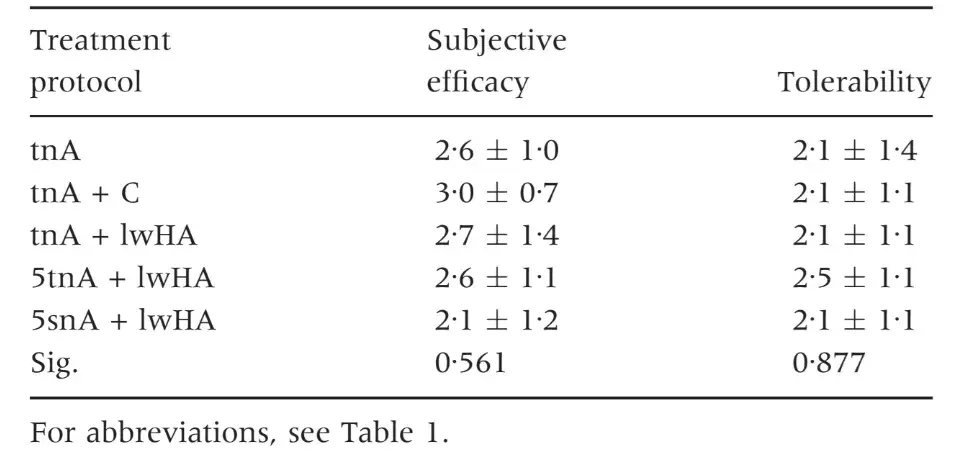
Table 4. Percentage of subjects within each treatment group referring an improvement in their outcome parameters at the end of the follow-up. Comparison between the treatment groups (Fisher’s exact test)
DISCUSSION
The present investigation was specifically designed in the attempt to get deeper into the knowledge on the effectiveness of arthrocentesis and injections in the management of inflammatory-degenerative disorders of the TMJ. The available literature has been not conclusive so far to indicate which is the most suitable treatment protocol to achieve pain relief and restore jaw function. Early papers suggested that the long-term benefit of corticosteroid injections in patients with TMJ pain was equally effective than occlusal splints on subjective symptoms and allowed achieving a better improvement in clinical signs (17); also, their short-term effects were similar to HA injections (18). Later on, very few clinical trials have been performed to compare treatment effects of different joint lavage and injections protocol. In one study, the effects of a cycle of five HA injections immediately following arthrocentesis were similar to those of occlusal splints and superior to no treatment at 6 months (7); in a couple of investigations performed on the same study sample, no significantly different treatment effects at 6 months were detected between two HA and corticosteroid injections performed 2 weeks apart (12, 19); in another trial, a single HA injection proved to be superior to oral anti-inflammatory drugs over a 3-month follow-up (20). In view of the paucity of investigations conducted on the issue, the two most recent systematic reviews of the literature, one dealing with the effectiveness of arthrocentesis (1) and the other one of HA (2), concluded that more research is needed to define better the indications and the risk-to-benefit ratio of the different injections protocol. Considering the absence of a standard of reference technique for administering arthrocentesis, exploratory research is needed to gather data on the argument. The lack of a reference treatment made difficult to adhere strictly to the criteria for conducting randomised and controlled trials (CONSORT statement) (21). The present investigation was the first to compare all the main available options for washing and injecting the TMJ, ranging from the single-session two-needle arthrocentesis technique described by Nitzan et al. (3) to the extensive protocol of 5 weekly HA injections immediately following arthrocentesis adopted by Guarda-Nardini et al. (6) and including single-session drug injections after arthrocentesis (22) as well as a single-needle technique for arthrocentesis (16). Findings did not support the clear superiority of one treatment protocol over the others to achieve pain management in TMJ inflammatory-degenerative joint disease over a short-term, viz., 3-month follow-up period. All protocols were associated with positive outcomes, in line with the TMD literature suggesting that improvement is, at least to some extent, partly because of unspecific treatment effects and to regression to the mean phenomena (23).Notwithstanding that, some suggestions can be drawn on the potential inter-protocol effect differences.
First, the protocol providing high molecular weight HA injections after arthrocentesis was withdrawn after two subjects experienced joint swelling and post-injection pain increase. This may suggest that such HA preparation is too viscous and has a too large steric interaction that prevents from achieving a quick diffusion within the small TMJ intra-articular space. The rationale for the adoption of high-viscosity HA stood in its potential longer-lasting effects with respect to low molecular weight preparations, but the present investigation did not provide encouraging findings on its potential applications in TMJ disorders. Such finding has to be further investigated with future studies.
Second, despite the absence of significant between-group differences, a tendency towards a better improvement in patients included in protocol E, viz., 5 weekly two-needle arthrocenteses plus low molecular weight HA injections, was detectable.
Patients receiving such treatment referred the most improvement in pain at chewing as well as chewing efficiency levels. In particular, the mean change in the pain at chewing scale was 5 ⁄ 10 on the VAS scale, accounting for more than a 64% improvement with respect to baseline values. All the other protocols allowed an improvement of pain at chewing levels comprised between the 11% and 41% range. Also, the protocol E group included the highest percentage of improved patients as for pain at chewing (91Æ7%), pain at rest (75%) and chewing efficiency levels (66Æ7%). The absence of statistically significant differences might be partly because of the statistical power of the study, which was designed to detect between-group differences of more than 50% in the treatment-related improvement. Much larger sample sizes might have been necessary to detect lower threshold differences: on the basis of data collected in this investigation that may serve as a guide for power analysis of future studies, up to 24, 43, and 97 patients per group needed to detect a 40%, 30%, and 20% difference, respectively. The low sample size may explain also the tendency towards significance for differences in mouth opening values, as baseline values of patients included in the various treatment protocols were not equal, even if not significantly different. Thus, an enlargement of sample in future studies would allow reducing ⁄ avoiding potential shortcomings owing to unequal patients’ allocation within the treatment groups. Also, the risk for type II error, viz., missing a significant difference owing to the low statistical power, should be diminished by the inclusion of larger samples. In any case, an appropriate a priori sample size analysis must be based on the selection of the post-treatment changes that are expected to be clinically relevant, and this is a very complex issue to deal with in pain studies. Indeed, considering the clinical and logistic difficulties to perform large sample clinical trials on this issue, studies attempting to identify the clinically significant VAS change threshold in patients with chronic TMJ pain have to be designed in the near future as a compelling requisite to avoid type II errors in the field of research on TMD treatment.
Third, protocol B, providing a single-session arthrocentesis plus corticosteroid injection, endorsed the highest improvement in mouth opening values. Such findings seem to be explainable with the lowest baseline range of motion in that treatment group, even if not clinically significant from the other groups. Patients included in protocol B also referred a higher subjective efficacy of the treatment, may be due to the positive effects perceived on mouth opening range and to the analgesic properties of corticosteroids.
Fourth, quite surprisingly, protocol E was tolerated better than the others, even if differences with the other treatments were not significant. In any case, such findings are interesting as far as concern the risk of being an approach too much invasive and less tolerated by the patients. Also, the single-needle approach, that was specifically introduced as a potentially better-tolerated variance of the two-needle technique, provided no positive outcomes in terms of patients’ tolerability of the treatment.
The above considerations may be open to several interpretations, the most important of which being that, despite the 3-month follow-up did not evidence significant differences between groups, studies on longer follow-up periods and enlarged sample sizes are needed to confirm findings. The short-term follow-up period of this investigation is indeed a limit to generalisation of findings, and longer periods of post-treatment observation may help confirming or refuting the tendencies described in this investigation.
Also, in the light of the absence of statistical significance for apparently large between-group differences as those detected for the percentage of improved subjects and the post-treatment changes in pain at chewing levels, researches assessing the clinically significant VAS changes in chronic TMJ pain have to be performed, because the risk for type II errors appears to be too high for investigations on this issue.
The present exploratory investigation has allowed gathering interesting data that could be useful to design future researches in accordance with suggestions to present high-quality randomised and controlled trials (21). On the basis of these findings, it might be assumed that a protocol providing 5 weekly two-needle arthrocentesis plus HA injections is a potential reference for comparison with other methods ⁄ protocol for administering arthrocentesis. Specific study designs comparing such protocol with other treatments must be adopted on the basis of the CONSORT guidelines for reporting clinical trials (21), and some strategies for controlling bias could be added with respect to the present exploratory study. In particular, a multidimensional assessment of pain measures, a measure of the temporal change in pain, the evaluation of comorbid conditions and the adoption of daily pain diaries over longer follow-up periods seems to be promising strategies to increase the internal validity of the research and to control for the fluctuation of symptoms over time.
Notwithstanding that, it should be kept in mind that the peculiar nature of the treatments under investigation prevents from achieving a full double-blind design, as the operators were blind with respect to the patients’ outcome parameters but they could not obviously be blind with respect to the technique they were performing. Actually, the expertise of the investigators performing the interventions and the single-examiner recording of the patients’ outcome parameters seem to be key factors to warrant the validity of the results and should be taken into account also in future studies.
Further details about treatment of TMD are accessible for you to learn in our course "Treatment of severe forms of TMJ diseases" by David Angelo and Sylvian Chamberland.
CONCLUSIONS
The present investigation was designed to get deeper into the study of the effectiveness of TMJ arthrocentesis and was the first attempt to compare six different treatment protocols in an exploratory clinical trial. Findings suggested that neither statistically nor clinically significant differences existed between the treatment groups, even if a protocol providing 5 weekly low molecular weight HA injections immediately following a classical two-needle arthrocentesis showed a tendency to a greater reduction of symptoms than all the other treatments to reduce pain-related symptoms in patients with inflammatory-degenerative TMJ disease over a 3-month period. The clinical significance and the external validity of these findings need to be confirmed with future studies on larger samples with longer follow-up periods.
References
Guo C, Shi Z, Revington P. Arthrocentesis and lavage for treating temporomandibular joint disorders. Cochrane Database Syst Rev. 2009;4:Art. No.:CD004973.
Manfredini D, Piccotti F, Guarda-Nardini L. Hyaluronic acid in the treatment of TMJ disorders. A systematic review of the literature. Cranio. 2010;28:166–176.
Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified method for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49:1163–1167.
Nitzan DW, Samson B, Better H. Long-term outcome of arthrocentesis for sudden-onset, persistent, severe closed lock of the temporomandibular joint. J Oral Maxillofac Surg. 1997;55:151–157.
Nitzan DW. ‘‘Friction and adhesive forces’’: possible underlying causes for temporomandibular joint internal derangement. Cells Tissues Organs. 2003;174:6–16.
Guarda-Nardini L, Tito R, Staffieri A, Beltrame A. Treatment of patients with arthrosis of the temporomandibular joint by infiltration of sodium hyaluronate: a preliminary study. Eur Arch Otorhinolaryngol. 2002;259:279–284.
Guarda-Nardini L, Masiero S, Marioni G. Conservative treatment of temporomandibularjoint osteoarthrosis:intra-articular injection of hyaluronic acid. J Oral Rehabil. 2005;32:729–734.
Axe MJ, Shields CL. Potential applications of hyaluronans in orthopaedics. Sports Med. 2005;35:853–864.
Ehrlich GE. Osteoarthritis. In: Rakel BE, Bope ET, eds. Conn’s current therapy, 58th edn. New York: Elsevier, 2006:921–925.
Guarda-Nardini L, Stifano M, Brombin C, Salmaso L, Manfredini D. A one-year case series of arthrocentesis with hyaluronic acid injections for temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:14–22.
Manfredini D, Bonnini S, Arboretti R, Guarda-Nardini L. Temporomandibular joint osteoarthritis: an open label trial of 76 patients treated with arthrocentesis plus hyaluronic acid injections. Int J Oral Maxillofac Surg. 2009;38:827–834.
Bjørnland T, Gjærum AA, Møystad A. Osteoarthritis of the temporomandibular joint: an evaluation of the effects and complications of corticosteroid injection compared with injection with sodium hyaluronate. J Oral Rehabil. 2007;34:583–589.
Nitzan DW, Price A. The use of arthrocentesis for the treatment of osteoarthritic temporomandibular joints. J Oral Maxillofac Surg. 2001;59:1154–1159.
Dworkin S, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria examinations and specifications, critique. J Craniomandib Disord. 1992;6: 301–355.
Kaneyama K, Segami N, Nishimura M, Sato J, Fujimura K, Yoshimura H. The ideal lavage volume for removing bradykinin, interleukin-6, and protein from the temporomandibular joint by arthrocentesis. J Oral Maxillofacial Surg. 2004;62: 657–661.
Guarda-Nardini L, Manfredini D, Ferronato G. Arthrocentesis of the temporomandibular joint: a proposal for a single-needle technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:483–486.
Kopp S, Wenneberg B. Effects of occlusal treatment and intraarticular injections on temporomandibular joint pain and dysfunction. Acta Odontol Scand. 1981;39:87–96.
Kopp S, Wenneberg B, Haraldson T, Carlsson GE. The short-term effect of intra-articular injections of sodium hyaluronate and corticosteroid on temporomandibular joint pain and dysfunction. J Oral Maxillofac Surg. 1985;43:429–435.
Møystad A, Mork-Knutsen BB, Bjørnland T. Injection of sodium hyaluronate compared to a corticosteroid in the treatment of patients with temporomandibular joint osteoarthritis: a CT evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e53–e60.
Oliveras-Moreno JM, Hernandez-Pacheco E, Oliveras-Quintana T, Infante-Cossio P, Gutierrez-Perez JL. Efficacy and safety of sodium hyaluronate in the treatment of Wilkes Stage II Disease. J Oral Maxillofac Surg. 2008;66:2243–2246.
Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134:663–694.
Alpaslan GH, Alpaslan C. Efficacy of temporomandibular joint arthrocentesis with and without injection of hyaluronic acid in treatment of internal derangements. J Oral Maxillofac Surg. 2001;59:613–618.
Manfredini D. Fundamentals of TMD management. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing, 2010:305–318.
/social-network-service/media/default/6707/045a2260.jpg)
