All about peri-implantitis
Machine translation
Original article is written in RU language (link to read it).
This article is devoted to the problem of peri-implatitis - a common complication that occurs in the practice of every implantologist, and therefore requires detailed study.
Peri-implantitis is a progressive resorption of bone tissue adjacent to the implant, caused by inflammatory phenomena in the soft tissues surrounding the implant, the formation of bone pockets, followed by filling of the resorbed fragment with granulations in the area of inflammation.
Learn more about the risk factors and causes of the development of peri-implantitis at the webinar Prevention of peri-implantitis: integration of the soft tissues surrounding the implant .
Classification of perimplantitis
Peri-implantitis, depending on the area and depth of resorption of bone tissue adjacent to the implant, is usually divided into the following classes:
Class I – horizontal slight loss of bone tissue, which leads to the formation of a minimal defect in the bone adjacent to the implant;
Class II – moderate horizontal loss of bone tissue, leading to the formation of a unilateral vertical bone defect in the implant area;
Class III – horizontal loss of bone tissue with the formation of a vertical bone defect along the perimeter of the implant;
Class IV – pronounced horizontal loss of bone tissue and the formation of a vertical defect around the implant with alveolar bone resorption.
Peri-implantitis, depending on the time of appearance, is divided into:
Early, due to the lack of osseointegration, which normally starts immediately after implantation.
Late – develops around a functioning implant and is associated with the loss of established osseointegration.

Figure 1. Peri-implantitis.
Etiology of peri-implantitis
It is customary to identify the following reasons for the development of peri-implantitis:
poor hygiene;
formation and subsequent suppuration of a hematoma over the plug;
the principles of atraumatic preparation of bone tissue were not followed;
small vestibule and scars;
inadequate healing of the surgical wound;
pathological load distribution;
insufficient bone volume;
periodontal diseases;
foci of odontogenic infection in the area of neighboring teeth.
Symptoms of peri-implantitis
Peri-implantitis is accompanied by progressive bone loss.
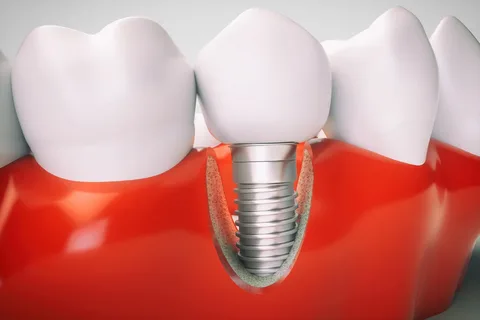
Figure 2. Peri-implantitis clinic.
Patients complain:
for pain in the implant area,
redness, swelling,
addition of peri-implant gum bleeding;
the formation of fistulas and gum pockets, the appearance of purulent discharge.
The gradual progression of the inflammatory process and the addition of bone tissue resorption causes the implant to become mobile and its function is lost.
Peri-implantitis occurs either immediately after implantation or in the long term, months and years after placement.
Objectively, during clinical examination, the following symptoms are determined:
redness and swelling of surrounding soft tissues;
the gums bleed when probed;
purulent exudate is released from the peri-implant pocket upon palpation;
the implant is movable;
The accumulation of plaque on adjacent teeth is determined.
Diagnostic principles
In diagnosing the presence and severity of peri-implantitis, various X-ray examination techniques are of decisive importance:
orthopantomography,
dental radiography,
cone beam computed tomography.
All of these methods make it possible to identify the degree and prevalence of bone tissue resorption.

Figure 3. Peri-implantitis on radiograph.
Additionally, laboratory tests are carried out, which are of auxiliary value:
microscopic,
morphological,
bacteriological,
biochemical,
pH-metry of oral fluid,
PCR.
Clinical symptoms:
soreness, discomfort;
redness of the mucous membrane or cyanosis around the implant;
the appearance of edema;
formation of a fistula tract with purulent discharge;
formation of a gum or bone pocket in the implant area;
implant mobility;
signs of bone resorption around the implant, which are revealed during x-ray examination.
Principles of peri-implantitis therapy
The goal of treating peri-implantitis is to prevent further loss of bone tissue, and in the long term, “reosteointegration” of the implant (formation of new bone in place of previously damaged one).
High-quality treatment of peri-implantitis involves performing two stages, where it is first necessary to eliminate gingival inflammation, and then carry out surgical sanitation of the pathological focus, followed by targeted osteoregeneration. The most important stage in the treatment of peri-implantitis is to stop the progressive loss of bone tissue by eliminating the plaque and eliminating the pocket.

Figure 4. Osseointegration is normal.
Stages of treatment for peri-implantitis
The initial phase of treatment for peri-implantitis is characterized by the elimination of plaque and tartar. As a result, the symptoms of gingival inflammation disappear.
The conservative phase involves professional hygiene, treatment of peri-implant pockets with an ozonized solution, oral applications and baths, and laser therapy. Careful control of the presence of dental plaque, especially on the crown and abutment. In some cases, it is necessary to modify the superstructures, which helps to level out the biomechanical overload of the implant.
Sometimes you can try to restore the loss of bone tissue using surgical techniques (guided osteoregeneration).
With the successful implementation of the initial phase of treatment, you can proceed to the second phase (surgical), which corresponds to periodontal therapy for rapidly progressing periodontal diseases.
During the surgical phase, it is extremely important to thoroughly clean the infected implant surface.
Sequence of stages of the surgical phase of treatment of peri-implantitis
An incision is made and the periodontal flap is raised.
The bone pocket is inspected, peri-implant granulations are carefully scraped out, the surface of the implant is cleaned using curettes or Perio-Flow, then detoxification treatment with a citric acid solution takes place on the surface of the implant, and the pocket is washed generously.
The operation ends with the introduction of a barrier membrane and osteoconductive material into the pocket.
The surgical wound is sutured.
A periodontal protective bandage is applied.
The postoperative period is accompanied by antiseptic rinses and antibiotics.
If recurrent or advanced peri-implantitis occurs, treatment requires removal of the implant and reimplantation.
Schematically, peri-implantitis therapy looks like this:
Assessment of oral hygiene.
Correction of individual oral hygiene of the patient.
It is important to achieve stable hygiene levels in the patient, to teach him to use toothpastes, rinses, and additional hygiene products every day.
Performing professional hygiene, using air abrasive systems and special tools.
Disinfection of abutments using chlorhexidine, Perio-Flow, laser, photodynamic therapy.
Anti-inflammatory drug therapy, in particular antibiotics.
Surgical sanitation of the peri-implant lesion.
Osteoregeneration.
Maintenance therapy
This stage is a set of measures that are necessary to consolidate the results of treatment over a long period of time; the goal of maintenance therapy is to achieve stable remission.
In periodontology, primary prevention involves preventing the occurrence of a pathological process, and secondary prevention, or maintenance therapy, includes measures to prevent the recurrence of the disease.
Maintenance therapy is a mandatory continuation of active treatment.

Figure 5. Healthy gums in the implant area.
Maintenance treatment in implantology is aimed at preventing recurrence of peri-implantitis or the occurrence of secondary complications.
Principles of supportive care
The patient maintains a satisfactory level of hygiene.
Regular examinations, strict adherence to the doctor’s recommendations.
Using not only a toothbrush, but also additional means to clean the interdental spaces and remove bacterial plaque as thoroughly as possible.
Antibacterial rinses.
During treatment planning, in order to ensure simplicity and convenience of individual hygiene, it is necessary to carefully consider the placement of implants, the choice of prosthesis design and abutments.
Due to the fact that inflammatory lesions cause destruction of bone tissue around implants, supportive treatment is an integral part of implant treatment.
More relevant information about the treatment of peri-implantitis at the webinar Treatment of peri-implantitis: surgical and non-surgical methods .

