An in vivo comparison of working length determination of two frequency-based electronic apex locators
Abstract
Aim: To compare in vivo the accuracy of two electronic apex locators (EALs) by means of digital radiographic imaging system.
Methodology: Electronic working lengths of 831 canals were determined with the DentaPort ZX and Raypex 5 apex locators and confirmed radiographically. The radiographic images acquired with the aid of a digital radiographic imaging system (VisualiX eHD; Gendex Dental Systems, Des Plaines, IL, USA) were blindly analysed by two independent evaluators. The distance between the file tip and the radiographic apex was measured using dedicated software (VixWin Pro, Gendex Dental Systems, Des Plaines, IL, USA) and the mean distance achieved between different tooth type and EALs were compared statistically. Statistical analyses were performed using the t-test for independent samples and one-way anova with the null hypothesis set as 5%. Positive or negative values were recorded when the file tip was detected beyond or short of the radiographic apex, respectively.
Results: The mean distance between file tip and radiographic apex were –1.08 ± 0.73 and –1.0 ± 0.67 mm considering DentaPort ZX and Raypex 5 groups, respectively, with no significant differences (P > 0.05). No statistically significant differences were found amongst the same tooth type when comparing both groups (P > 0.05) or amongst different teeth type in the same group (P > 0.05).
Conclusions: Within the limitations of this in vivo study, the DentaPort ZX and Raypex 5 were similar in terms of accuracy.
Introduction
Accurate determination of working length (WL) during root canal treatment is a challenge. Although there are different opinions on the apical limit of root canal instrumentation and filling (Nekoofar et al. 2006), the apical constriction, where the pulp tissue is connected to the apical periodontal tissue, is recommended by some as the appropriate landmark. The constriction is the narrowest part of the root canal in the apical region and is also referred to as the minor diameter (Ricucci & Langeland 1998).
Clinically, locating the tip of the endodontic file at the constriction is difficult. The usual method to determine the WL has been a combination of knowledge of root lengths, assessment of a preoperative radiograph, tactile discrimination, and assessment of a radiograph exposed with an adequate-size instrument placed into the root canal as a means of calibration against image projection distortion (Heo et al. 2008).
Nevertheless, those methods of WL determination may prove inaccurate, depending on the direction and the extent of the root curvature and the position of the apical foramen (Stein & Corcoran 1992, Williams et al. 2006). Hence, digital radiography and electronic apex locators (EALs) have the potential to facilitate the recognition of the instrument inside the canal, allowing more precise in vivo determination of WL (Gordon & Chandler 2004, Nekoofar et al. 2006, Nair & Nair 2007).
Digital intraoral imaging system have many advantages compared with conventional film-based radiography, including the potential for lower radiation exposure to the patient, the ability to enhance the acquired image, time saving between exposure and display, ease of maintenance of the radiographic data and, particularly in endodontics, the almost instant display of the image (Heo et al. 2008).
Although Custer (1918) was the first to propose an electrical method to estimate the root canal length, the first such device was constructed by Sunada (1962). Since then, various types of EALs have been developed (Gordon & Chandler 2004, Nekoofar et al. 2006).
Advances in technology have led to the development of EALs, such as the DentaPort ZX (J. Morita Mfg. Corp., Kyoto, Japan), which determines the position of the minor diameter by simultaneous measurement of impedance at two different frequencies (8 and 0.4 kHz) (Ebrahim et al. 2007a,b, Stavrianos et al. 2007, Versiani et al. 2009). A quotient of impedance (‘ratio method’) is then calculated, which expresses the position of the file in the canal (Kobayashi & Suda 1994). This device works on the same principle as the original Root ZX, which has been tested in several studies and subsequently became a reference in electronic WL investigation (Shabahang et al. 1996, Dunlap et al. 1998, Pagavino et al. 1998, Welk et al. 2003, Haffner et al. 2005, Venturi & Breschi 2005, Wrbas et al. 2007, Kim et al. 2008).
The Raypex 5 (VDW, Munich, Germany) also uses two different frequencies (8 and 0.4 kHz) and its measurements are based on the root mean square values of the signals (Gordon & Chandler 2004, Nekoofar et al. 2006).
To date, few in vivo studies have been conducted to analyse the accuracy of these EALs (ElAyouti et al. 2002, Hör et al. 2005, Ebrahim et al. 2007a,b, Stavrianos et al. 2007, Wrbas et al. 2007, Briseño-Marroquin et al. 2008, Pascon et al. 2009). Hence, the purpose of this in vivo investigation was to compare the performance of the DentaPort ZX and Raypex 5 in establishing the WL in 831 canals (362 patients), in combination with a digital radiographic imaging system.
Material and methods
Three hundred and sixty-two healthy patients, aged 21–68 years, with a total of 491 teeth (831 canals) planned for root canal treatment in the Calabrodental Centro Odontriatrico (Crotone, Italy), participated. Informed written consent in full accordance with ethical principles was obtained from each patient before the treatment was initiated (World Medical Association 2004). All teeth had completely formed apices confirmed by standard preoperative periapical radiographs. The digital radiographic images were acquired using a dental X-ray generator (Oralix AC; Dentsply Italy, Gendex Division, Milano, Italy) with a charge-coupled device detector (VisualiX eHD; Gendex Dental Systems, Des Plaines, IL, USA) and the aid of a digital sensor-positioning device (Endo Ray Rinn, Dentsply, Weybridge, UK). The optimal exposure time (0.16 s) was established in a pilot study.
Under local anaesthesia (2% mepivacaine hydrochloride with adrenaline 1 : 100 000; Parke-Davis, Milan, Italy), the teeth were isolated with rubber dam. Caries and existing metal restorations were removed, and standard access preparations were carried out using high-speed diamond round burs under water coolant in such a way that a straight-line access to the root canals was achieved. The incisal or occlusal edges were ground lightly to create flat surfaces for reproducible reference points. After location of canal orifices, the coronal and middle portions were flared with Gates Glidden drills sizes 2–3 and the contents of the canals removed with a barbed broach. After that, the canals were irrigated with 5 mL of 1% NaOCl.
The pulp chamber was dried gently with air and sterile cotton pellets were used to dry the tooth surface and eliminate excess irrigant, with no attempt at drying the canal. The WL was independently determined using DentaPort ZX or Raypex 5, according to manufacturers’ instructions. Four endodontists, previously trained in the use of both devices, working individually on their own patients, gathered the data. The length was electronically checked in each canal using one of the EALs selected by draw. First, the lip clip was attached to the patient’s lip and a stainless steel size 15 reamer was connected to the file holder of the EAL. Using the DentaPort ZX, the file was advanced within the root canal to just beyond the foramen, as indicated by the flashing APEX bar and the continuous tone. The file was then withdrawn until a flashing bar between ‘APEX’ and ‘1’ had been reached. Using the Raypex 5, a file was advanced in the same manner to just beyond the foramen (red light), and then it was withdrawn until all flashing green bars were visible.
Measurements were considered suitable if the instrument remained stable for at least 5 s. Upon completion of electronic measurement, the largest file that could be placed securely at the established electronic WL was positioned and the silicone stopper adjusted to the coronal reference point. Digital radiographic images were acquired, as previously described, and stored in DICOM format before being analysed using image processing software (VixWin Pro Digital Imaging Software; Gendex Dental Systems, Des Plaines, IL, USA), that had been developed for optimizing radiographic images, ensuring a precise measurement of the distance between the instrument tip and the tooth radiographic apex, in millimetres, with a degree of accuracy of 0.01. Positive or negative values were recorded when the file tip was detected beyond or short of the radiographic apex, respectively. All measurements were registered blindly by two endodontists, not familiar with the group assignment of the patients, and averaged. The image reading sessions were performed twice, with an interval of 15 days, in a dark room. All digital images were viewed on a high-resolution monochrome TFT-LCD monitor (ME315L; Totoku Electric Co., Tokyo, Japan) at a resolution of 1536 · 2048. Observers were instructed to let their eyes adapt to the darkness before viewing images and each one, independently, measured the images in a different order to avoid bias.
Intra- and inter-operator variations were estimated using Student’s t-test (P = 0.05). The Kolmogorov– Smirnov test was applied to show whether the results of measurement were consistent with a normal distribution. Distribution of difference values showed that electronic measurements followed normal distributions thus, parametric statistical analysis was possible (t-test for independent samples), and the null hypothesis was set as 5%. One-way anova test (P = 0.05) was performed to compare the distance values recorded in different tooth types in the same experimental group. All analyses were carried out with the statistical package SPSS version 15 (SPSS Inc., Chicago, IL, USA).
Results
Intra- and inter-operator variations revealed no difference significance within the measurements of a given operator or between operators (Student’s t-test In a total of 831 canals (491 teeth), the WL was measured by the DentaPort ZX in 416 canals (127 anteriors, 54 premolars and 235 molars), whilst the Raypex 5 was used in 415 canals (164 anteriors, 65 premolars and 186 molars).
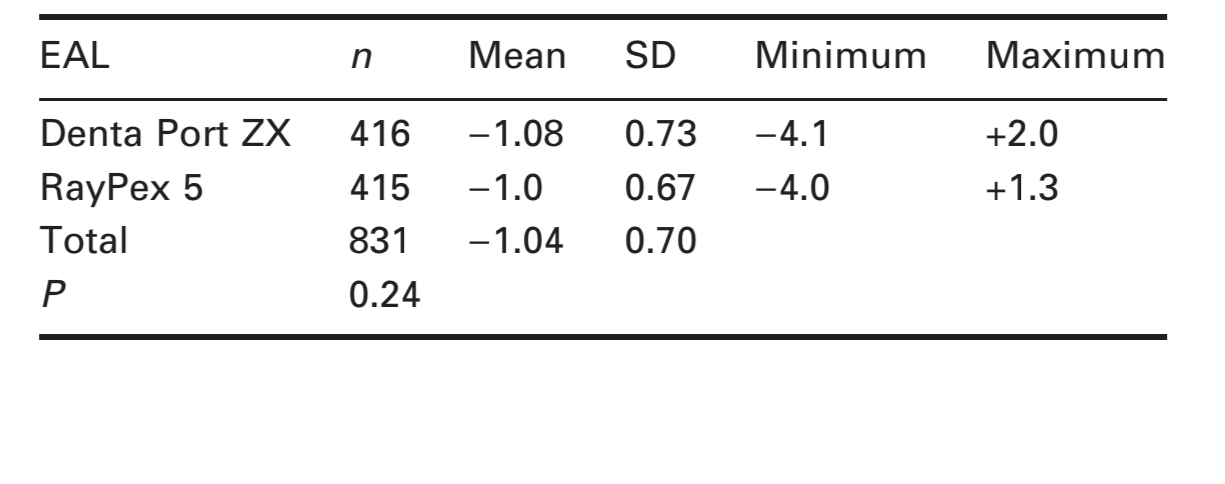
Data in Table 1 indicate that the distance between the file tip and the radiographic apex achieved during WL determination ranged from –4.1 to 2.0 and –4.0 to 1.3 mm in the DentaPort ZX and Raypex groups, respectively. Moreover, the mean distances were –1.08 ± 0.73 and –1.0 ± 0.67 mm in the DentaPort ZX and Raypex groups, respectively, with no significant differences (t-test for independent samples, P > 0.05).
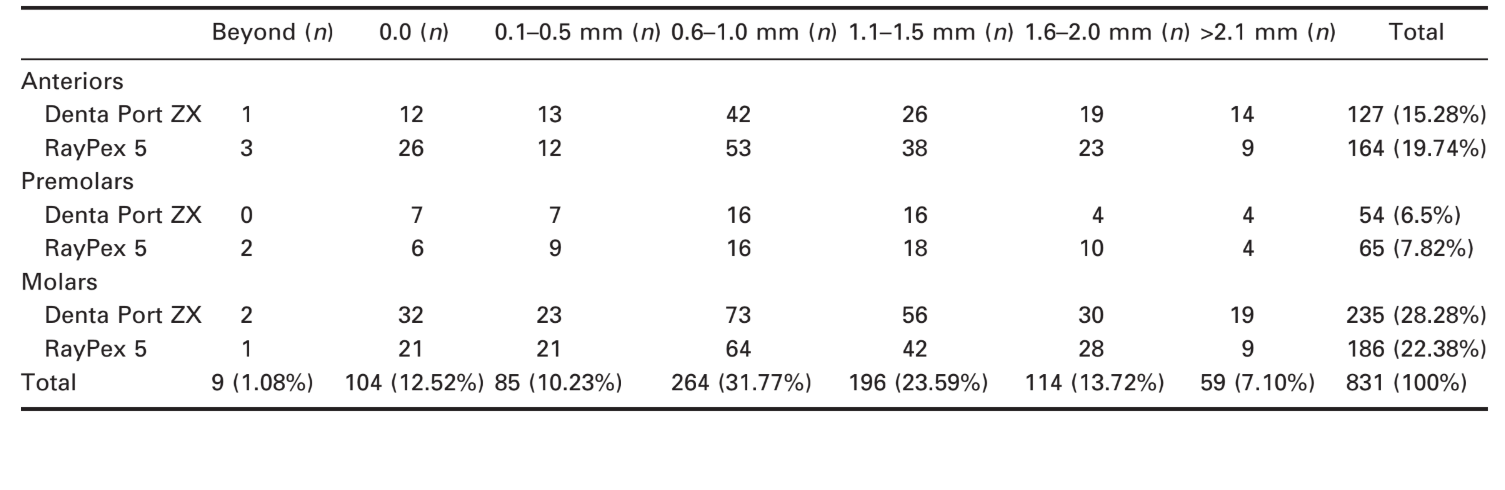
The effect of WL determinations by tooth types with the DentaPort ZX and Raypex are outlined in Table 2. Considering all cases, 1.08% (n = 9) and 7.1% (n = 59) resulted in overestimated and underestimated WL, respectively, whilst 73.5% of the readings (n = 611) were between 0.5 and 2.0 mm. In 12.5% of the sample (n = 104), the file tip was flush with the external root surface at the apex.
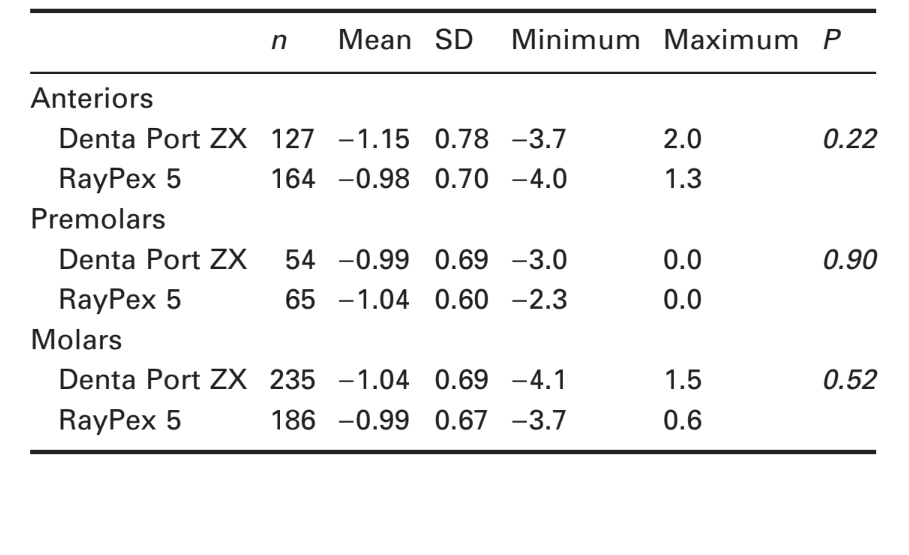
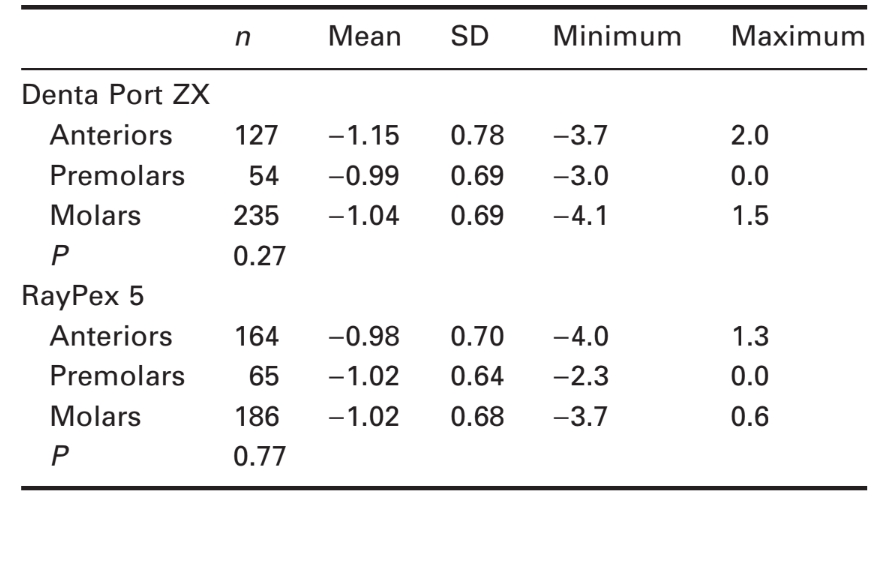
No statistically significant difference was found amongst the same tooth type when comparing the EALs (t-test for independent samples, P > 0.05) (Table 3), or amongst different tooth types in the same group (one-way anova, P > 0.05) (Table 4)., P > 0.05).
Discussion
The goal of the present study was to compare the clinical accuracy of two EALs in a large sample and not their reliability regarding determination of the distance between the electronically located canal terminus and the minor foramen.
As it has been reported that pulp diagnosis does not affect the accuracy of EALs (Dunlap et al. 1998, Pagavino et al. 1998, Venturi & Breschi 2005), the present study did not take account of the pulp condition. The root canals were rinsed with 1% NaOCl and all electronic measurements were performed using a stainless steel size 15 reamer (Briseño-Marroquin et al. 2008).
Stavrianos et al. (2007) comparing the in vivo accuracy of WL determination in 80 single-rooted teeth with vital pulp tissue, planned for extraction, reported that the DentaPort ZX located the apical foramen in 95% of cases and the Raypex 4 in 92.5%. Wrbas et al. (2007) compared the in vivo accuracy of the Root ZX and Raypex 5 in 20 single-rooted teeth scheduled for extraction and demonstrated that the minor foramen was located within the limits of ±0.5 mm in 75% and 80% of the cases, respectively. Taking into account a tolerance level of ±0.5 mm, in vivo studies have also demonstrated an accuracy of the Root ZX in determining the apical constriction or apical foramen in 82.3% (Dunlap et al. 1998), 82.75% (Pagavino et al. 1998), 90.7% (Welk et al. 2003), 78% (Haffner et al. 2005), and 86.6% (Venturi & Breschi 2005). Similarly, the Raypex has been reported to have an accuracy of 80% (Wrbas et al. 2007) and 92.5% (Stavrianos et al. 2007). In the present work, although teeth were not extracted, the results (Tables 1 and 3) were in accordance with those of Stavrianos et al. (2007) and Wrbas et al. (2007) that demonstrated no statistical difference between the DentaPort ZX and Raypex.
In 1.08% (n = 9) and 12.5% (n = 104) of the sample, the file tips were beyond or at the radiographic apex, respectively (Table 2). Considering previous studies of root apex anatomy (Kuttler 1958, Ricucci & Langeland 1998) and the evidence demonstrated by Welk et al. (2003) that 28.5% of the WL that appeared radiographically acceptable revealed the file tip beyond the foramen, it is reasonable to presume that many of these cases were through the foramen. Likewise, Dunlap et al. (1998), using the Root ZX to compare the canal length to the actual apical constriction, in vital and necrotic cases, reported that in 26% of the readings the file tips were beyond the radiographic apex. Pagavino et al. (1998), testing the Root ZX in order to locate the root canal foramen, observed that the file tip protruded beyond the most coronal border of the foramen in all sample. Welk et al. (2003), comparing the accuracy of the Root ZX and Endo Analyzer Model 8005, found 6.2% of cases were encountered with an overestimated WL determination in the Root ZX group. Wrbas et al. (2007) when comparing the accuracy of two electronic EALs in the same teeth found that the file tip was beyond the major foramen in eight cases for Root ZX and in four cases for Raypex. Kim et al. (2008), comparing the in vivo accuracy of WL determination using the Root ZX, showed that file tips were extruded beyond the apical constriction in 15 canals.
Under clinical conditions, a greater variation of measurements is expected, because the favourable laboratory circumstances for precise measurements are not available and, in consequence, an overestimated WL and a potential overextended root filling could lead to a poor prognosis (de Chevigny et al. 2008). Besides, these findings raise the question of whether the WL should be established at the point where the EAL indicates the constriction, or some distance coronal to that point (Dunlap et al. 1998, Tselnik et al. 2005, Pascon et al. 2009, Versiani et al. 2009). Some authors have proposed that, when using the ‘0.5’ mark on the display of Root ZX, an adjustment of the file is required to ensure that its tip does not protrude beyond the apical constriction. So, they have recommended a withdrawal of the instrument of between 0.5 and 1.0 mm to avoid over-preparation (Pagavino et al. 1998, Haffner et al. 2005, Wrbas et al. 2007, Versiani et al. 2009). Thus, completing root canal treatment with only the length determination as provided by DentaPort ZX or Raypex 5 would have, in some cases, likely placed the root canal filling material into the periodontal ligament and bone.
Conclusion
Within the limitations of the study, no statistically significant difference was found when comparing clinical accuracy of the DentaPort ZX and Raypex 5, even considering different tooth types in the same experimental group. A number of the readings would have resulted in a WL that was too long.
Authors: E. A. Pascon, M. Marrelli, O. Congi, R. Ciancio, F. Miceli, M. A. Versiani
References:
- Briseño-Marroquin B, Frajlich S, Goldberg F, Willershausen B (2008) Influence of instrument size on the accuracy of different apex locators: an in vitro study. Journal of Endodontics 34, 698–702.
- de Chevigny C, Dao TT, Basrani BR et al. (2008) Treatment outcome in endodontics: the Toronto study–phase 4: initial treatment. Journal of Endodontics 34, 258–63.
- Custer LE (1918) Exact methods of locating the apical foramen. Journal of the National Dental Association 5, 815–9.
- Dunlap CA, Remeikis NA, BeGole EA, Rauschenberger CR (1998) An in vivo evaluation of an electronic apex locator that uses the ratio method in vital and necrotic canals. Journal of Endodontics 24, 48–50.
- Ebrahim AK, Wadachi R, Suda H (2007a) An in vitro evaluation of the accuracy of Dentaport ZX apex locator in enlarged root canals. Australian Dental Journal 52, 193–7. Ebrahim AK, Wadachi R, Suda H (2007b) In vitro evaluation of the accuracy of five different electronic apex locators for determining the working length of endodontically retreated teeth. Australian Endodontic Journal 33, 7–12.
- ElAyouti A, Weiger R, Lost C (2002) The ability of root ZX apex locator to reduce the frequency of overestimated radiographic working length. Journal of Endodontics 28, 116–9.
- Gordon MP, Chandler NP (2004) Electronic apex locators. International Endodontic Journal 37, 425–37.
- Haffner C, Folwaczny M, Galler K, Hickel R (2005) Accuracy of electronic apex locators in comparison to actual length – an in vivo study. Journal of Dentistry 33, 619–25.
- Heo MS, Han DH, An BM et al. (2008) Effect of ambient light and bit depth of digital radiograph on observer performance in determination of endodontic file positioning. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 105, 239–44.
- Hör D, Krusy S, Attin T (2005) Ex vivo comparison of two electronic apex locators with different scales and frequencies. International Endodontic Journal 38, 855–9.
- Kim E, Marmo M, Lee CY, Oh NS, Kim IK (2008) An in vivo comparison of working length determination by only root-ZX apex locator versus combining root-ZX apex locator with radiographs using a new impression technique. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 105, e79–83.
- Kobayashi C, Suda H (1994) New electronic canal measuring device based on the ratio method. Journal of Endodontics 20, 111–4.
- Kuttler Y (1958) Microscopic investigation of root apexes. Journal of the American Dental Association 50, 544–52.
- Nair MK, Nair UP (2007) Digital and advanced imaging in endodontics: a review. Journal of Endodontics 33, 1–6.
- Nekoofar MH, Ghandi MM, Hayes SJ, Dummer PMH (2006) The fundamental operating principles of electronic root canal length measurement devices. International Endodontic Journal 39, 595–609.
- Pagavino G, Pace R, Baccetti T (1998) A SEM study of in vivo accuracy of the Root ZX electronic apex locator. Journal of Endodontics 24, 438–41.
- Pascon EA, Marrelli M, Congi O, Ciancio R, Miceli F, Versiani MA (2009) An ex vivo comparison of working length determination by three electronic apex locators. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 108, (in press).
- Ricucci D, Langeland K (1998) Apical limit of root canal instrumentation and obturation, part 2. A histological study. International Endodontic Journal 31, 394–409.
- Shabahang S, Goon WW, Gluskin AH (1996) An in vivo evaluation of Root ZX electronic apex locator. Journal of Endodontics 22, 616–8.
- Stavrianos C, Vladimirov SB, Vangelov LS, Papadopoulos C, Bouzala A (2007) Evaluation of the accuracy of electronic apex locators Dentaport ZX and Ray Pex 4 under clinical conditions. Folia Medica 49, 75–9.
- Stein TJ, Corcoran JF (1992) Radiographic ‘‘working length’’ revisited. Oral Surgery, Oral Medicine, and Oral Pathology 74, 796–800.
- Sunada I (1962) New method for measuring the length of the root canals. Journal of Dental Research 41, 375–87.
- Tselnik M, Baumgartner JC, Marshall JG (2005) An evaluation of Root ZX and Elements Diagnostic apex locators. Journal of Endodontics 31, 507–9.
- Venturi M, Breschi L (2005) A comparison between two electronic apex locators: an in vivo investigation. International Endodontic Journal 38, 36–45.
- Versiani MA, Santana BP, Caram CM, Pascon EA, Sousa CJA, Biffi JCG (2009) Ex vivo comparison of the accuracy of Root ZX II in detecting apical constriction using different meter’s reading. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 108, e41–5.
- Welk AR, Baumgartner JC, Marshall JG (2003) An in vivo comparison of two frequency-based electronic apex locators. Journal of Endodontics 29, 497–500.
- Williams CB, Joyce AP, Roberts S (2006) A comparison between in vivo radiographic working length determination and measurement after extraction. Journal of Endodontics 32, 624–7.
- World Medical Association (2004) Declaration of Helsinki: ethical principles for medical research involving human subjects. International Journal of Bioethics 15, 124–9.
- Wrbas KT, Ziegler AA, Altenburger MJ, Schirrmeister JF (2007) In vivo comparison of working length determination with two electronic apex locators. International Endodontic Journal 40, 133–8.

