Froggy mouth: a new myofunctional approach towards atypical swallowing
Abstract
Introduction: Atypical swallowing has a high incidence in adult and child populations. The treatment of the latter is generally achieved by the adoption of orthodontic appliances in conjunction with speech therapy. The aim of this article is to describe the clinical protocol of Froggy Mouth, an innovative myofunctional appliance designed to correct the atypical swallowing.
Materials and methods: The Froggy Mouth appliance has been tested by the authors Di Vecchio at the Orthognatodontics department of Fatebenefratelli San Pietro Hospital in Rome, Italy, and by Mancini at the Orthodontics department of Carlo Poma Hospital in Mantova, Italy. This article will illustrate the clinical protocol of the appliance with therapeutic indications, clinical phases, instruction and patients and parents motivation and follow-up results.
Results: Froggy Mouth has proven effective in the correction of atypical swallowing, from both the clinical and the functional standpoints. The fastest and most predictable results were obtained in patients during their physiological developmental age. This appliance, compared to the traditional logopaedic therapy, requires less commitment in terms of time for the patient (only 15 minutes per day), with more predictable and durable results over time.
Conclusions: The clinical evidences indicate that the Froggy Mouth is effective in the myofunctional correction of the atypical swallowing mechanism, providing the clinician a new therapeutic approach for neuromuscular retraining of atypical deglutition and dysfunctional deglutition in patients during their growth phase. However, further scientific evidences are needed to support the results of this investigation.
Introduction
Atypical swallowing is a myofunctional problem, characterised by an altered lingual posture during swallowing. Primary infantile deglutition develops around the 12th week of intrauterine life and it is characterised by a forward tongue posture [Bernandi et al., 2013] and contraction of the perioral muscles [Tecco et al., 2015] (orbicular and buccinator), leading to a higher negative pressure in the oral cavity. In normal conditions, around the age of 3 and with the development of alternate unilateral mastication [Mummolo et al., 2014], the infantile deglutition pattern changes into a so-called mature deglutition pattern [Condò et al., 2012].
During adult or mature swallowing, dental arches are in contact and tongue is elevated, resting in the posterior- superior part of the palatine vault [Suàrez et al., 2014]. During this phase the tongue pressure stimulates the anteroposterior and transversal growth of the maxilla [Eichenberger et al., 2014; Mummolo et al., 2014]. If transition from the infantile to the adult swallowing does not take place, the former triggers a pathological mechanism, defined as atypical swallowing [Giuca et al., 2008].
The aetiology is multifactorial.
- Altered lifestyle such as prolonged bottle feeding, late weaning, consistency of food (lack of solid food).
- Bad habits such as finger or dummy sucking, onycophagy, labial interposition.
- Respiratory problems such as oral breathing, adenoid hypertrophy, tonsillar hypertrophy, rhinitis, bronchial asthma.
- Congenital oral anomalies (short lingual frenulum or ankyloglossy).
- Atypical deglutition is frequently correlated with the following.
- Dental malocclusions [Tecco et al., 2014]: proclined maxillary anteriors, increased overjet, openbite, flaring and spaced dentition.
- Skeletal malocclusions [Tecco et al., 2011]: sagittal and transversal discrepancies with a narrow and protruded maxillary arch, mandibular retroposition.
The high prevalence of malocclusions related to atypical swallowing makes this a subject of strong interest in scientific researches. Because of the multifactorial aetiopathogenesis, high incidence and the correlation with dento-skeletal malocclusions, this topic is not only very interesting for clinicians, but is also strongly debated among healthcare providers. A literature review on this subject confirms that orthodontic treatment alone is not sufficient to solve the problem in patients with atypical swallowing. This requires a multidisciplinary therapy, orthodontic and myofunctional approach, to ensure optimal and long-lasting results [Maspero et al., 2014].
To obtain an adequate myofunctional correction [Mummolo et al., 2014] of atypical swallowing has been treated with appliances such as palatal tongue crib, fixed or removable, the Tucat pearl or speech therapy exercises, requiring a high compliance from the patient, and giving unpredictable and unstable results.
Eric Kandel, Nobel-prize winner in 2000, in his research on the physiological basis of memory storage in neurons has proved that new information is acquired and stored promptly, because the memory cerebral systems are easily modifiable. His studies have proven that when working on subconscious levels it is important not just the duration of treatment but also consistency. Synaptic connections in various brain circuits can be reinforced or slowed down by the engrammatic mechanism and mnemonic traces formed during the learning process and experience, determining in this way definitive biochemical and structural changes [Kandel, 2007].
The learning process occurs through:
- Voluntary pathway, with the stimulation of cortical zones causing synaptic excitation only;
- Involuntary pathway, with modification of synapses structure and increase in their numeric value (permanent stabilisation of new acquisitions); here stimulation origins from the subcortical region, in which automatisms are developed.
Following Kandel’s research, Patric Fellus (expert in Dentofacial Orthopaedics) designed the Froggy Mouth appliance, which triggers the involuntary pathway, inhibiting bilabial contact and eliminating negative pressure inside oral cavity, enabling the tongue to protrude and retract through styloglossus muscle contraction, thus achieving proper deglutition. Fellus states that the attention of the patient should not be focused on tongue tip, as it usually happens during myofunctional therapy, but on the posterior portion of the tongue. The patient, engaged in tongue tip elevation trying to reach the retroincisal papilla, triggers a lower position of the posterior portion of the tongue, inhibiting elevation of the posterior portion of the tongue by styloglossus muscle action, which would consequently place the tongue tip in its physiological position [Fellus, 2006; Fellus, 2014; Fellus, 2016; Ortu et al., 2016].
The aim of this article is to describe the clinical protocol of Froggy Mouth, an innovative and simple myofunctional appliance used in order to solve atypical swallowing and to allow myofunctional correction of altered tongue position. Benefits and limits of this appliance will be confronted with the traditional logopaedic therapy and other appliances traditionally used for the resolution of this condition.
Materials and methods
The Froggy Mouth appliance has been tested in 370 patients at the Orthognatodontics Department of Fatebenefratelli San Pietro Hospital in Rome and at the Orthodontics department of Carlo Poma Hospital in Mantova (Italy).
Froggy Mouth is a small removable appliance made of a flexible thermoplastic elastomer, without latex or phthalates. It is available in 3 sizes of different colour orthoboxes S (Blue), M (red) and L (Violet) (Fig. 1). The appliance has a small stamped letter in the inferior portion and a dot in the superior portion. In order to choose the right size, the appliance has a specific dedicated caliber. The Froggy Mouth should be positioned between the lips and the teeth leaving about 2 mm from the labial commisure on both sides.

The Froggy Mouth should be used 15 minutes every day (in order to activate the neural circuits that generate the automatic movements controlled by the trigeminal nerve) always during a playful activity (in order to activate the lymbic system that facilitates and accelerates the learning process) [Kandel, 2007]: preferably watching TV, while playing videogames or using the computer. The protocol requires to maintain a correct head position parallel to the floor.
Indications of Froggy Mouth are: atypical sawllowing, tongue interposition between dental arches, anterior and posterior openbite, trasversal contraction, anterior or posterior crossbite, increased overjet, proclined front teeth, deep bite, mandibular protrusion, dyslalia, bruxism, posture alteration, oral breathing and adenoid disorders,snoring, drooling.
Before delivery of the appliance, the following was required:
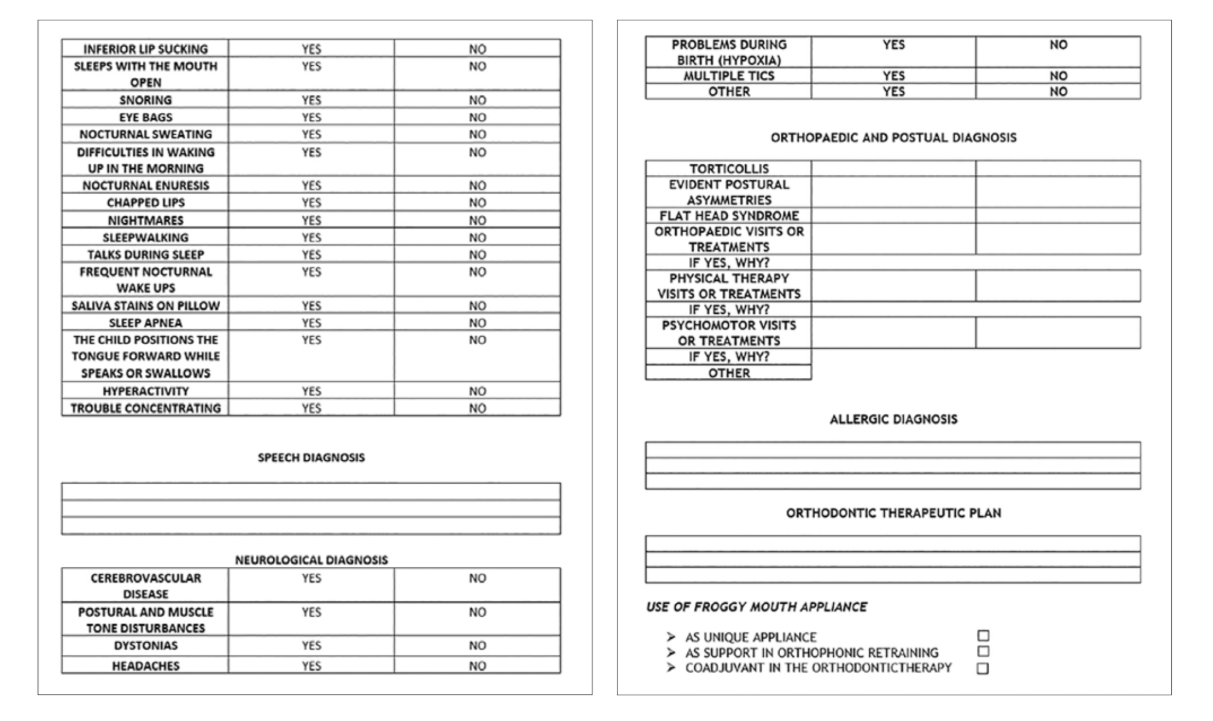
- Filling of the Clinical record (Fig. 2-4).
This ad hoc Clinical record was created in collaboration with different health care providers that followed this group of patients during their growth phase (logopaedists, ostheopathic doctors, allergologists).

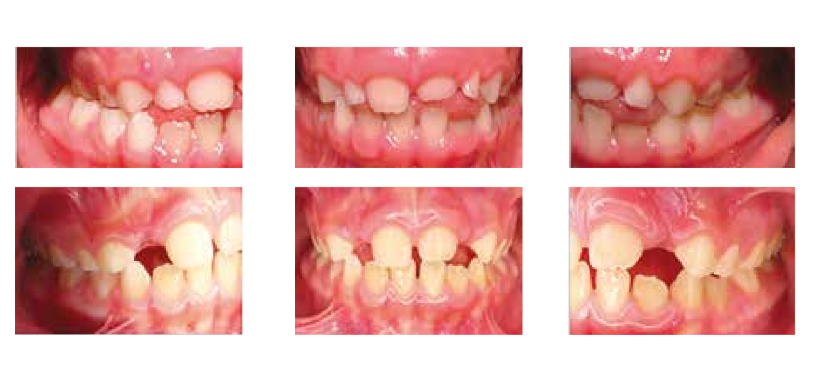
2. Collection of intraoral and extraoral photos of the patients (Fig. 5, 6), impressions, ortopantomographs and lateral cephalograms.


3. Instructions were given to patients and their parents; motivated to maintain a proper hygiene.
4. Follow-up appointments were scheduled every 6–8 weeks, and the orthodontist established the duration of treatment based on the clinical results.
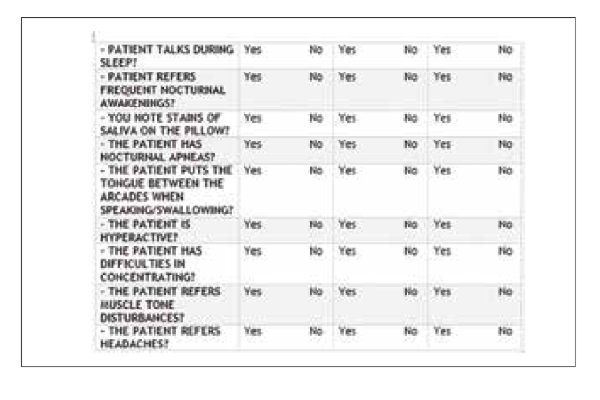
5. At the follow-up appointments, intraoral and extraoral photos were taken. Patients or guardians were asked to fill in a treatment progress questionnaire, in order to evaluate the response to the treatment (Table 1).

This questionnaire is very important because it helps clinicians to record data that can not be observed during the follow-up appointment (i.e. snoring, sleeping with mouth open, sleep apnoea, somnambulism, etc.).
Results
Froggy Mouth resulted effective in the correction of atypical swallowing. This appliance showed positive clinical results in resolving malocclusions such as open bite (Fig. 7), transverse palatal contraction, cross bite (Fig. 9) and deep bite (Fig. 10) in patients during their physiological growth phase. From the evaluation of the treatment progress questionnaire, it can be observed that the Froggy Mouth helped in resolving other issues such as snoring, drooling, sleep apnoea, and difficulty breathing through nose (Table 2).



Extraoral photos (Fig. 11) show the change in the face, neck and shoulder position immediately after wearing the device.

These clinical results can point out a direct correlation between an altered contraction of perioral and masticatory musculature and an asymmetrical contraction of cervical musculature, with TMJ and posture implications [Saccomanno et al., 2014; Ortu et. al., 2018]. This requires a good cooperation with the osteopath, to monitor and elaborate these early results [Ottria et al., 2018; Ottria et al., 2018; Ottria et al., 2018]. The device also requires less compliance from the patient (only 15 minutes per day) compared to traditional speech therapy alone and, as established by the studies of Kandel [2007], the results are more predictable and long-lasting.
Conclusions
Clinical evidences indicate that the clinical protocol of Froggy Mouth is effective in the myofunctional correction of the atypical swallowing mechanism, providing the clinician a new therapeutic approach for atypical swallowing and dysfunctional deglutition in patients during their growth phase. However, it should be underscored that the concomitant speech therapy is crucial for faster and effective results. However, further scientific evidence should support these early results.
Authors: S. Di Vecchio, P. Manzini, E.Candida, Gargari M.
References
- Bernardi S, Zeka K, Mummolo S, Marzo G, Continenza MA. Development of a new protocol: a macroscopic study of the tongue dorsal surface. It J Anatom Embriol 2013; 118(2):24.
- Tecco S, Baldini A, Mummolo S, Marchetti E, Giuca MR, Marzo G, Gherlone EF. Frenulectomy of the tongue and the influence of rehabilitation exercises on the sEMG activity of masticatory mucles. J Electromyogr Kinesiol 2015; 25(4):619-628.
- Mummolo S, Ortu E, Necozione S, Monaco A, Marzo G. Relationship between mastication and cognitive function in elderly in L’Aquila. Int J Clin Exp Med 2014; 7(4):1040-6.
- Condò R, Costacurta M, Perugia C, Docimo R. Atypical deglutition: diagnosis and interceptive treatment.
- A clinical study. Eur J Paediatr Dent 2012; 13(3):209-14.
- Suàrez C, Antonarakis GS, Pham D. Occlusal characteristics in subjects with or without the ability to roll the tongue. Eur J Paediatr Dent 2014; 15(2):147-150.
- Eichenberger M, Baumgartner S. The impact of rapid palatal expansion on children’s general healt: a literature review. Eur J Paediatr Dent 2014; 15(1):67-71.
- Mummolo S, Marchetti E, Albani F, Campanella V, Pugliese F, Di Martino S, Tecco S, Marzo G. Comparison between rapid and slow palatal expansion: evaluation of selected periodontal indices. Head Face Med 2014; 10:30.
- Giuca MR, Pasini M, Pagano A, Mummolo S, Vanni A. Longitudinal study on a rehabilitative model for correction of atypical swallowing. Eur J Paediatr Dent 2008; 9(4):170-4.
- Tecco S, Lacarbonara M, Dinoi MT, Gallusi G, Marchetti E, Mummolo S, Campanella V, Marzo G. The retrieval of unerupted teeth in pedodontics: two case reports. J Med Case Rep 2014; 8:334.
- Tecco S, Mummolo S, Marchetti E, Tetè S, Campanella V, Gatto R, Gallusi G, Tagliabue A, Marzo G. sEMG activity of masticatory, neck, and trunk muscles during the treatment of scoliosis with functional braces. A longitudinal controlled study. J Electromyogr Kinesiol 2011; 21(6):885-92.
- Maspero, C., et al. Atypical swallowing: a review. Minerva Stomatol 2014 63(6): 217-227.
- Mummolo S, Tieri M, Tecco S, Mattei A, Albani F, Giuca MR, Marzo G. Clinical evaluation of salivary indices and levels of Streptococcus Mutans and Lactobacillus in patients treated with Occlus-o-Guide. Eur J Paediatr Dent 2014; 15(4):367-70.
- Kandel E. Alla ricerca della memoria. La storia di una nuova scienza della mente 2007, Codice edizioni, Torino.
- Felus P. Dysfuctions linguale et dysmorphies Orthod Fr 2006; 77: 105-12
- Fellus P. Succion et dèglutition Revue d’Orthopedie Dentofacial 2014; vol 48; 4 : 425-8
- Fellus P. De la succion-dèglutition à la dèglutition du subject dentè Orthod Fr 2016; 87: 89-90
- Ortu E, Lacarbonara M, Cattaneo R, Marzo G, Gatto R, Monaco A. Electromyographic evaluation of a patient treated with extraoral traction:a case report. Eur J Paediatr Dent 2016; 17(2):123-128.
- Saccomanno S, Antonini G, D’Alatri L, D’Angeloantonio M, Fiorita A, Deli R. Case report of patients treated with an orthodontic and myofunctional protocol. Eur J Paediatr Dent 2014; 15(2):184-186.
- Ortu E, Pietropaoli D, Marchetti E, Marchili N, Marzo G, Monaco A. Bruxism in children: use of the Functional Plane of Monaco (FPM). Eur J Paediatr Dent 2018; 19(4):287-294
- Ottria L, Candotto V, Guzzo F, Gargari M, Barlattani A. “Temporomandibular joint and related structures: anatomical and Histological aspects”. J Biol Regul Homeost Agents. 2018 Jan-Feb; 32(2 Suppl. 1):203- 207.
- Ottria L, Lauritano D, Guzzo F, Gargari M, Barlattani A. “Anatomic relationship between temporomandibular joint and middle ear”. J Biol Regul Homeost Agents. 2018 Jan-Feb;32(2 Suppl. 1):209-212.
- Ottria L, Candotto V, Guzzo F, Gargari M, Barlattani A. “TMJ’s capsule histological and macroscopical study: relationship between ligamentous laxity and TMI dysfunctions”. J Biol Regul Homeost Agents. 2018 Jan-Feb; 32(2 Suppl. 1):213-216.
