Indirect bonding technique
Machine translation
Original article is written in ES language (link to read it) .
Summary
The purpose of this article is to describe the management of two clinical procedures in the indirect bonding technique, using double acetate (soft - rigid) and silicone in the positioning of brackets following the protocol established in the Postgraduate Course in Orthodontics at the Unit of Dental Specialties.
With the aim of minimizing or eliminating the parallax error factor and achieving excellence in clinical procedures within the placement of fixed orthodontic appliances, it is found that the indirect technique provides benefits such as reduced chair time, increased precision in the positioning of fixed appliances (brackets), and consequently, a decrease in visual errors in positioning relative to the center of the clinical crown.
Introduction
The cutting-edge Orthodontics that has seen a significant resurgence in recent years since the emergence of pre-adjusted appliances generates in the clinician the concern and need to consider the correct positioning of bands and brackets, as with the development of the pre-adjusted system, the center of the clinical or anatomical crown became the vertical and horizontal reference for the placement of the brackets.
However, many orthodontists began to overlook the visual errors due to appreciation direction that arise, either due to a deficiency in the use of positioners or a lack of ergonomics in their clinical practice by not properly positioning the patient in the chair. Similarly, various factors such as excessive crowding, gingival inflammation, partially erupted teeth, crowns displaced towards the palatal or lingual that condition an imprecise placement of the brackets, generate the need in many orthodontists to seek and implement a procedure that reduces these errors.
Although less than 10% of orthodontists use an indirect bonding technique, there is a general acceptance that brackets can be placed accurately outside the mouth, on study models rather than directly on the teeth.
This statement is even more important when using pre-adjusted brackets, and it is through indirect bonding that a significant reward is found in terms of quality of care, system benefit, and treatment efficiency, always supported by an accurate diagnosis.
In the 1970s, Cohen, Silverman et al. Newman, Moin Dogon, Simmons, and later Thomas, first described the indirect technique, where self-polymerizing materials were used. It wasn't until 1999 that Dr. Sondhi published a method based on self-curing resins and incorporated the use of acetate for the correct positioning of fixed appliances.
There are two problems that are usually associated with indirect bonding:
- An additional and precise procedure is needed in the laboratory.
- The difficulty in achieving a quick and flawless adhesion of the brackets to the teeth.
However, we can consider that the additional laboratory procedures can be delegated to well-trained laboratory personnel, avoiding consuming the orthodontist's time, and that the introduction of new adhesive systems added to the procedures proposed in this work contributes to reducing the uncertainty associated with this type of indirect bonding technique.
Based on the aforementioned considerations and with a firm commitment to providing our patients with excellent treatments, the following work aims to describe step by step two different procedures (double soft-rigid acetate and silicone), where the stage corresponding to the placement of brackets was carried out using an indirect technique, with the goal of achieving precise positioning of each of the brackets and consequently avoiding the repositioning of brackets in more advanced orthodontic phases, having a direct effect on the reduction of chair time and on the correct evolution of orthodontic treatment.
Clinical Aspects
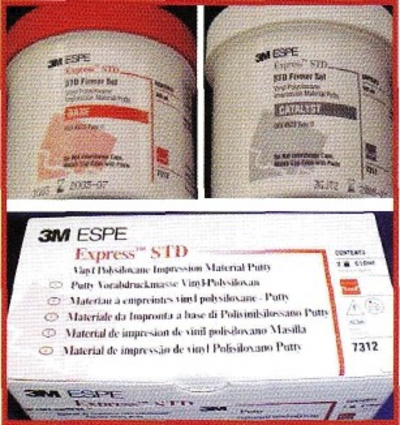
The clinical procedures with double acetate and silicone are very similar to each other, as they aim to achieve the same objectives and only differ from one another in the preparation and materials used for the transfer matrix. In both procedures, the use of Vacuum is employed; in the silicone technique, it is only necessary to mix the base and catalyst of the silicone (3M ESPE Vinyl Polysiloxane Putty). Fig.2.a.
Indirect bonding technique
The placement of brackets indirectly carried out in the Dental Specialties Unit is based on the review of various procedures employed by different clinicians, but due to their complexity in development and lack of practicality, aspects are revisited that make this technique a simpler, ergonomic, and straightforward approach, allowing the clinician to apply it in their practice. While it is increasingly being introduced into daily consultations, it is an alternative that offers promising results and helps ensure that the clinician does NOT make errors in the positioning of the brackets and benefits the mechanics of the philosophy practiced in their private practice.
Once the diagnosis of our patient is finalized and addressing the clinical and biomechanical aspects of the treatment, the first step in both procedures is to take impressions to obtain plaster models for orthodontics. Once these are retrieved, they undergo a dehydration and hydration process for 15 minutes, followed by a drying process at room temperature.
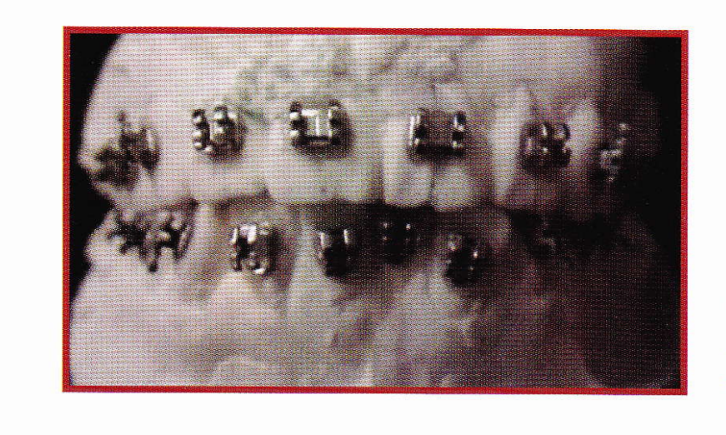
Next, we proceed to crucify each tooth in the axial and horizontal models, in order to determine the height of each tube and brackets, using Dougherty MBT positioners to reduce errors in the placement of fixed orthodontic appliances. (figure 1-b)
A thin layer of gypsum separator is applied to the entire palatine and vestibular surface of the teeth and should be left to dry for 15 minutes.
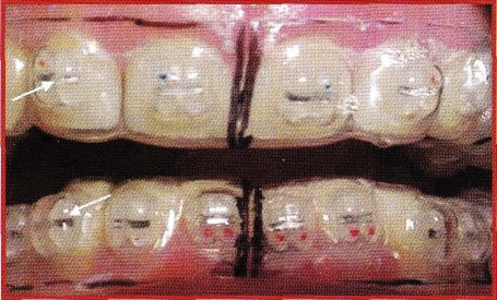
The brackets are properly placed on the models using light-curing resin. (figures 1.c.1 and 1.c.2)
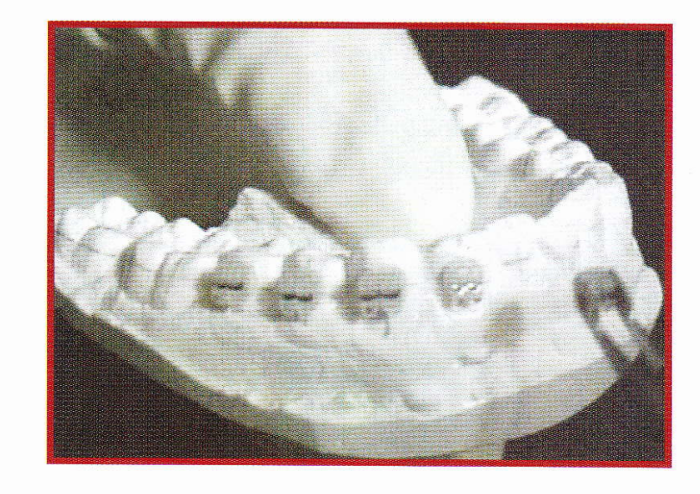
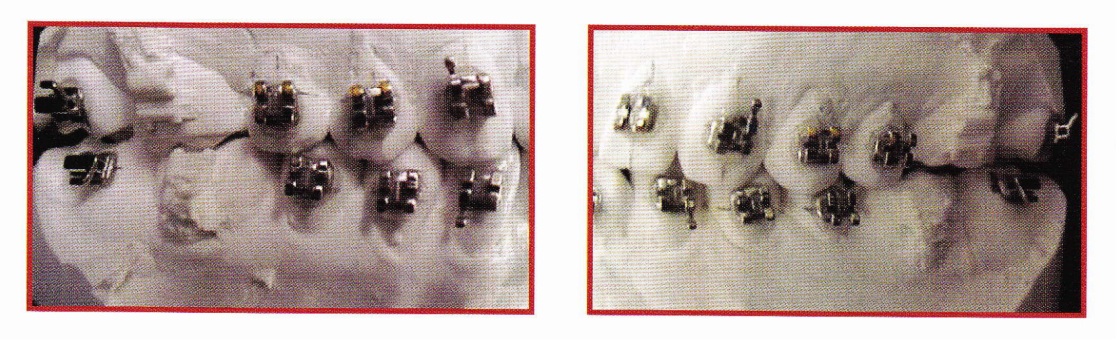
Each of the brackets and bondable tubes are placed according to the bracket positioning guide table of the MBT system, and are photopolymerized for a period of 15 seconds for each bracket and tube.
Double acetate procedure
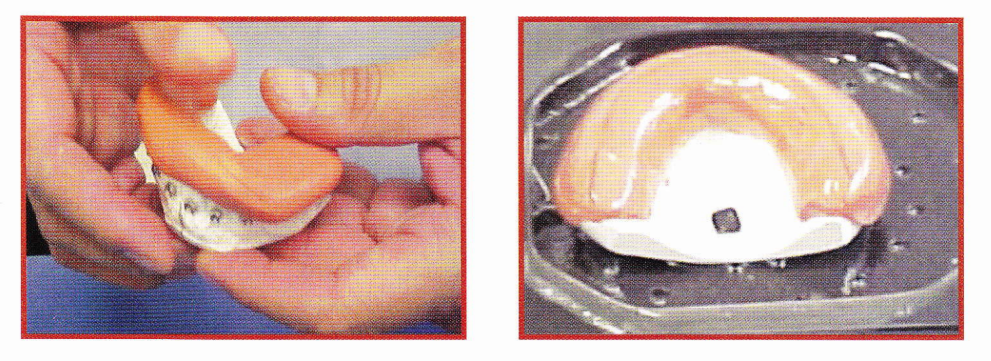
In the double acetate technique, each of the models is placed in the vacuum machine and the application of the soft acetate gauge 35 is first carried out, followed by the rigid gauge 30 acetate. It is important to place petroleum jelly between one acetate and another as it will allow for separation during the transfer sequence. (figure 1.d)
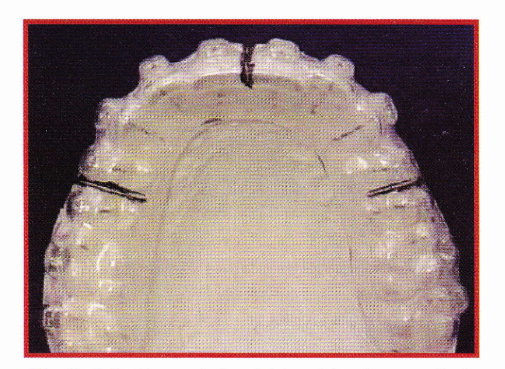
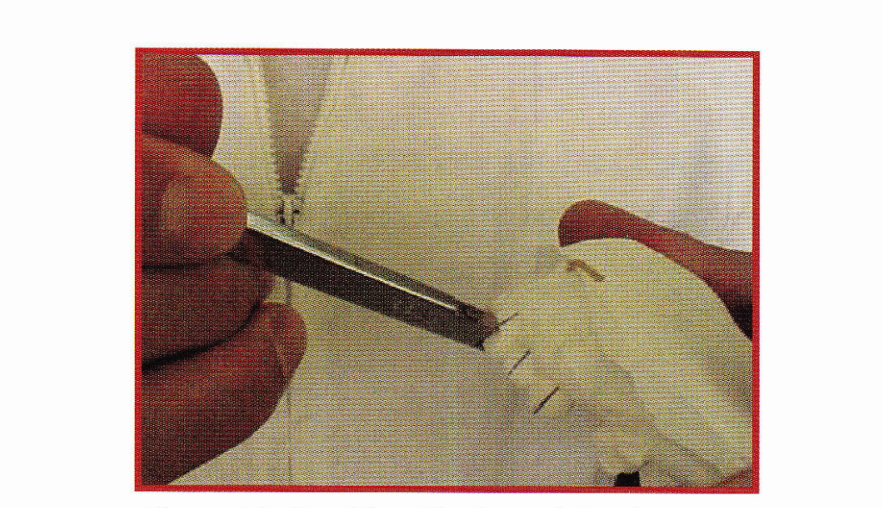
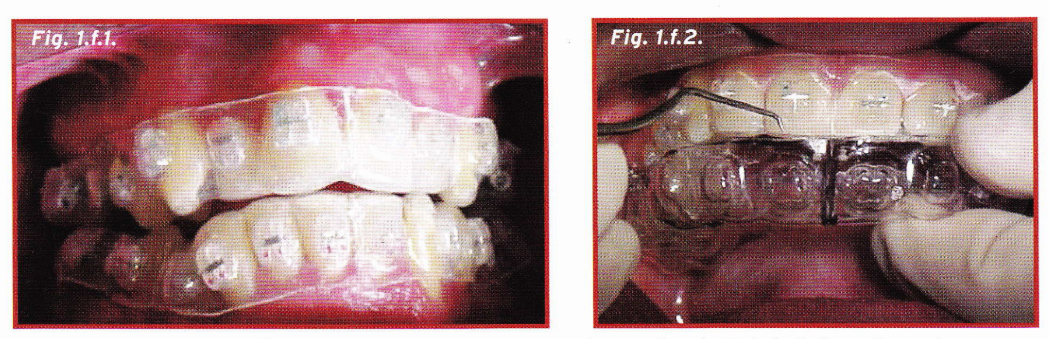
The acetates are then trimmed with No. 17 SS. WHITE discs at the level of the central incisors and premolars on the buccal side, and once this is completed, the transfer matrices with the brackets trapped inside the acetate are retrieved. (fig.1.e.1 and 1.e.2).
The base of the brackets and tubes of both matrices are micro-etched and taken to a system for impurity removal using ultrasonic equipment for 15 minutes.
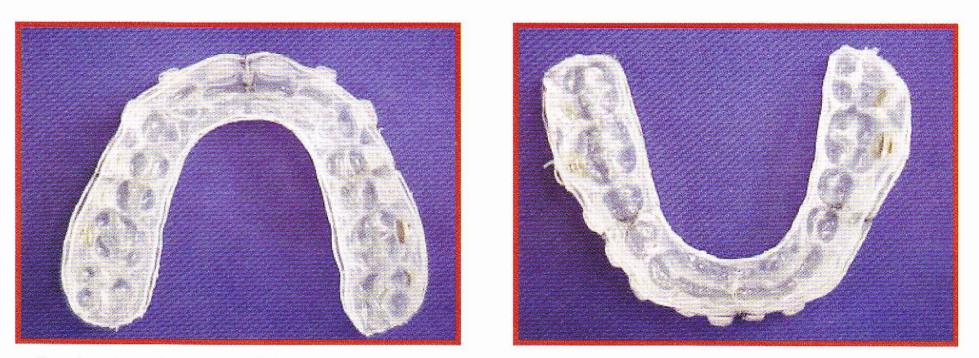
Silicone Procedure
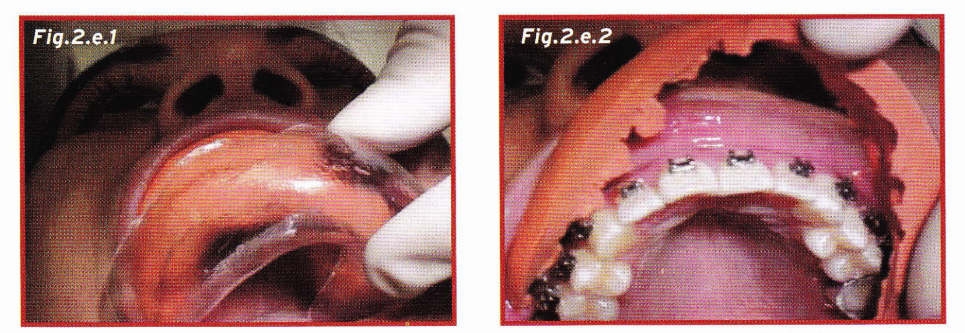
In the silicone procedure, the 3M ESPE Vinyl Polysiloxane Putty base and catalyst are mixed and applied to the model where the brackets were positioned (Fig. 2.b.). The next step involves taking the model with the silicone matrix to the vacuum machine and applying a rigid 30 gauge acetate (Figure 2.b.2).
The transfer in the mouth is done through the following sequence, where both dental arches are first isolated and perfectly recorded. In this step, isolation plays an important role, as it is recommended to have a double suction to avoid saliva contamination.
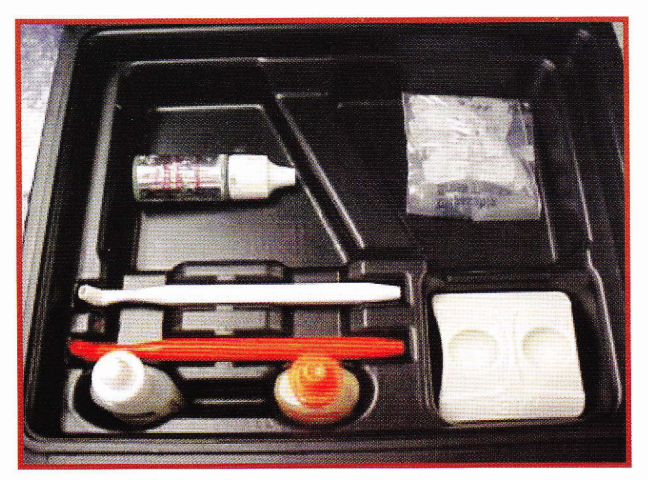
Thus, from this step, the liquid resin kit from Dr. Sondi, 3M Unitek (fig.3.a), is used, which consists of two resins A and B. Resin A is placed on the dental surface, and Resin B is placed on the mesh of the base of tubes and brackets of the transfer matrix in a non-excessive amount, and it is immediately transferred to the mouth, where it must be inserted and pressed evenly for 5 minutes, a sufficient time for the chemical reaction of both resins to occur, verifying that the matrix fits properly over the teeth. This will generate a slight ischemia on the gum, a favorable detail that guarantees a correct fit between the acetate matrix and the dental structures.
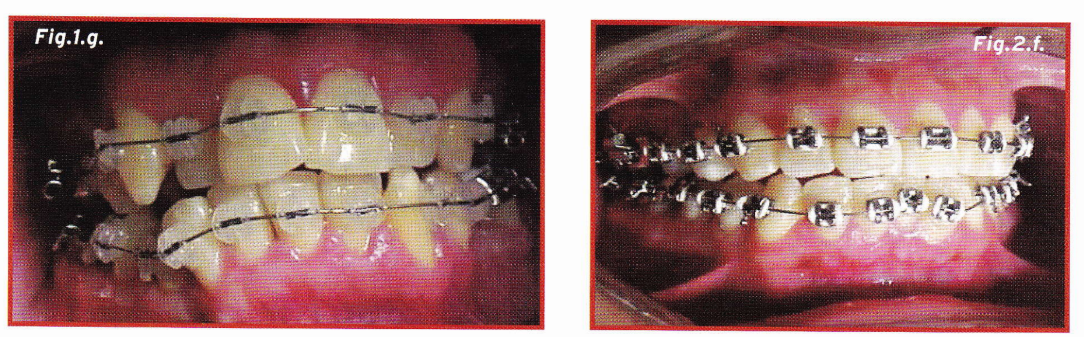
The removal of the acetates is carried out with the help of an explorer, and thanks to the vertical cuts made in the double acetate technique (figure 1.a), and cuts on the center of the occlusal surface of the teeth with a scalpel; in the silicone technique, it allows us to easily remove the hard and soft silicone or acetate. (figures 1-f.2, 2-e.1 and 2.e.2)
Final considerations
The indirect bonding technique for brackets is an excellent alternative aimed at compensating for the limitations that the orthodontic clinician has regarding the correct positioning of their fixed appliances. Currently, whether using acetates or silicone, it is a technique that does not require excessive expenses and its preparation is easy to execute in the office, allowing for faster patient care and, like any technique, it requires perfection and mechanization to achieve the best results for the benefit of the patient and the biomechanics.
"In the past, the best results were achieved by orthodontists who made the best wire bends. In the future, the best results will be from orthodontists who are the best bracket positioners."
Authors: Franco Fonseca Balcazan, Ricardo Riquelme Ortiz.
References:
- Sondhi A. Efficient and effective indirect bonding. Am J Orthod Dentofac Orthop 1999; 4:1.352 359.
- Hickam J.H. Predictable indirect bonding. J Clin Orthod 1993; 27:215-218.
- White L.W. A new improved indirect bonding technique. J Clin Orthod 1999; 33: 17-23.
- Kalange J.T. Ideal Appliance placement with APC brackets and Indirect bonding. J Clin Orthod 1999; 33: 516-524.
- Gottlieb E.L, Nelson A.H. Vogels D.S. 1996 JCO study of orthodontic Diagnosis and treatment procedures, Part I: results and trends. J Clin Orthod 1996; 30: 615-630.
- Sondhi, Anoop: "Efficient and effective Indirect Bonding" Am J Orthod Dentofacial Orthop, 1999; 115:352-9.
- Orthodontic Perspective. “A Clinical Review of the MBT Orthodontic Treatment Program”. 1999; 03-10.
