Treatment of a Patient with Progressive Periodontal Disease
Machine translation
Original article is written in RU language (link to read it) .
The worsening prognosis for a dental arch with numerous periodontal diseases poses a serious problem for both the dentist and the patient. For the patient facing the reality of transitioning from a natural, hopeless dental arch to a removable denture, it is probably the biggest change in the oral cavity they will ever experience.
The set of protocols for rehabilitating patients with complete edentulism is presented in the online course Prosthodontics on Implants. Implantation + Orthopedics.
Psychological issues and functional problems due to tooth loss and the need to adapt to a new chewing system are compounded by additional problems such as deterioration in taste and temperature. It is extremely important for the treating physician to conduct a thorough and frank discussion with the patient, explaining the differences and expectations associated with chewing natural teeth and dental prostheses. Moreover, a full understanding of the differences between tissue-adhering prostheses and implant-supported dental prostheses will help patients make an informed choice for their future. The following case demonstrates a method of treatment planning using various ways to treat a patient with progressive periodontal diseases.
While reducing overall risk and improving prognosis should always guide treatment decisions, orthodontics and restorative dentistry can provide means to delay the gradual loss of periodontally involved teeth and ensure acceptable interim results.
Clinical Case Review
Patient History and Main Complaint
A 54-year-old woman complained that she could not eat properly. She added that she was embarrassed by her upper teeth, as they had shifted and turned, and was also concerned about a missing front tooth on her lower jaw.


Being an employee at a local grocery store, she had a limited income. Throughout her life, she had irregular dental visits, which were usually prompted by pain and often led to tooth extractions.
The patient was treated 1 year ago for tooth 2.1. The tooth was endodontically treated and capped with a crown. At that time, the patient was informed about periodontal diseases and was recommended a comprehensive treatment plan for many teeth.

The patient was somatically healthy without any medical contraindications to dental care, therefore her medical risk was considered low and the prognosis was good.
Diagnosis, Risk Assessment, and Prognosis
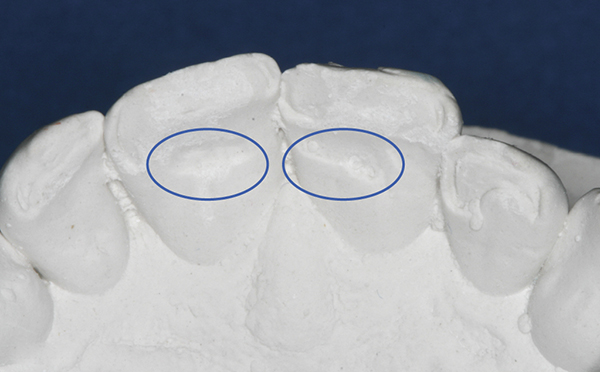
Periodontium: during the examination, severe bleeding on probing was detected. The probing depth ranged from 5 mm to 8 mm around teeth 1.2-2.2 and 4.6. Radiographic bone loss of more than 4 mm, with intrabony defects in the area of teeth 1.2-2.2, 4.4, and 4.6. Teeth 1.2-2.2 had a mobility of grade 3, while teeth 1.3, 4.2, 4.4, 4.6 had a mobility of grade 1. Gum recession of more than 2 mm was noted in the area of teeth 1.3-1.1, 2.3, 3.5, 3.3, 3.1, 4.4, 4.6.
Risk: high
prognosis: hopeless for teeth 1.2-2.2 and 4.6.
Biomechanically: after clinical examination, two acceptable amalgam restorations were found. The filling of tooth 4.4 had a small overhanging edge, while tooth 4.6 had an extensive amalgam restoration that compromised the structural integrity of the tooth. There were no signs of active caries.
Risk: moderate
forecast: unfavorable
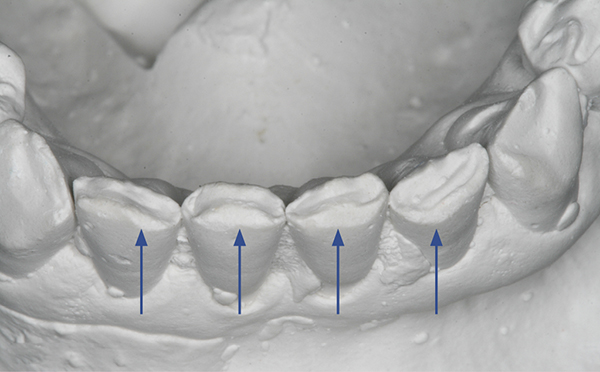
Functionally: the patient had minimal exhaustion. Secondary occlusal trauma was noted on teeth №№ 3.1, 4.2, and 4.4. Clinical examination revealed the presence of a unilateral click on the right when opening the mouth. Due to the absence of lateral teeth, the patient developed a malocclusion with loss of height.

Initial diagnosis — occlusal dysfunction.
Risk: moderate
forecast: unfavorable
Dentofacially: in a resting state, teeth 1.2, 1.1 were positioned labially compared to the adjacent teeth.
It was found that the upper lip has medium mobility dynamics, whereas the lower lip demonstrates high dynamics.
Risk: from medium to high
Treatment Goals
After discussing with the patient about the high risk of periodontal disease, being attentive and understanding to her financial, aesthetic, and functional concerns, the doctor and the patient together developed treatment goals. For the lower jaw, the goal was to stabilize the periodontal condition and create favorable conditions for future prosthetics. For the upper jaw, the goal was to eliminate the periodontal hopeless situation by removing all remaining teeth and allowing the bone and tissue to heal, thereby creating a stable healthy environment for placing implants. The prosthetic plan involved placing implants followed by upper jaw prosthetics.

Treatment Plan
Upon informing the patient, the following treatment plan was developed, which must be carried out in stages.
- Remove all remaining upper teeth and fabricate a full denture with immediate loading.
- Remove tooth 4.6 and start orthodontic treatment on the lower dental arch.
- Place four implants in the upper jaw and one implant in the lower jaw.
- Attach an abutment and crown to the secured implant at tooth 4.5.
- Create a composite structure to temporarily fill the space of the missing tooth 3.2.
Stages of Treatment
Stage 1: Extractions, Immediate Denture, and Orthodontics
In the first stage of treatment, all teeth in the upper jaw were removed, and a full dental prosthesis was fabricated, which reduced the periodontal risk for the patient in the upper jaw. This procedure was accompanied by all the records necessary to ensure a successful outcome. Additionally, tooth 4.6 was removed, which reduced the patient's biomechanical risk from moderate to low.
Limited orthodontic treatment on the lower jaw began simultaneously with the extraction on the upper jaw. The purpose of the limited orthodontic treatment was to close the gaps between the lower teeth and preliminarily stabilize the periodontal condition by reducing the vertical load on the periodontium.

Orthodontic treatment also provided optimal alignment of the teeth on the lower jaw. This was intentionally planned to prepare for and gradually transition to implants due to periodontal risk and poor prognosis. The transition, when necessary, may involve fixed implant-supported prosthetics with a crown or bridge, or a removable prosthesis on implants. The decision will depend on the patient's desires and financial capabilities.
Stage 2: Planning and Placement of the Implant
After a 4-month waiting period using a denture, a scan of the upper jaw was conducted to determine the optimal location for four upper jaw implants. The plan was to place the implants in the area of the canines and second premolars.

Anatomical landmarks, especially on the upper jaw, usually do not allow for parallelism of implants. However, the template used in this case (Locator™, ZEST Anchors, www.zestanchors.com), shows some expected divergence, although achieving the maximum possible parallelism between implants when placing is still ideal.

The greater the parallelism between the implants, the easier it becomes to apply the dental prosthesis, and there is less wear on the plastic retaining liners that fit the Locator attachments. Clearly, reducing the wear of the liners will lead to improved durability and less need for prosthesis replacement.
Once the planning was completed, four implants were placed on the upper jaw, and one implant in the bone layer was positioned at tooth 4.5.
Stage 3: Completion of orthodontic treatment
After the completion of the orthodontic treatment, a lingual wire was placed on the lower front teeth. This wire served three purposes: (1) it prevented relapse after orthodontic treatment; (2) acted as a periodontal splint for teeth affected by periodontitis, and (3) provided fixation for the composite structure replacing tooth 3.2.
As soon as the wire was in place, the straight composite structure was attached to teeth 3.3 and 3.1 and the lingual wire as a temporary aesthetic solution until the patient was ready to proceed with further treatment.
Stage 4: Final Prosthesis
Final prosthesis. In the last phase of treatment, a prosthesis was placed with fixation on the upper jaw implants, as well as an implant abutment and a metal-ceramic crown for tooth 4.5.
The height was improved as a result of local orthodontics. The efficiency of the patient's masticatory system improved before the continuity of the dental rows was restored by the implant-supported prosthesis.
Discussion
The patient had two long-term options available: (1) to receive a fixed bridge prosthesis supported by implants in the area of teeth 3.1 and 4.2 or (2) to choose a removable prosthesis held by implants. Both options were significantly better than a conventional removable partial or full denture. If she had opted to have a bridge prosthesis on four implants, she could have avoided a removable prosthesis. This future treatment plan can also be staged, which is extremely important for a patient with a limited budget.
An additional consideration was the high dynamics of the lower lip, where during a maximum smile it showed all the lower front teeth and gum tissues. This revealed a high aesthetic risk with a fair and unfavorable prognosis for the restoration of the lower jaw.

Transition to a Removable Denture
The transition from natural teeth to a removable denture is quite traumatic for most patients. This can be mitigated by frank discussion and careful consideration of options and expectations. When possible, it is best to recommend patients restore their broken dental prostheses with implant-supported prostheses, because they do not interfere with daily functions such as eating, talking, and smiling. By avoiding the removal of all remaining teeth at once during treatment, the condition of patients can be alleviated. It is rare that the dental arch is in such a severe condition that it requires the removal of all remaining teeth at once. By choosing teeth that can be maintained for several additional years, with greater collaboration and periodontal monitoring, it is possible to organize and provide an optimal treatment plan for the future.
For patients who are experiencing severe financial difficulties and are on a limited budget and cannot afford the ideal treatment plan immediately, this solution meets urgent needs and provides stability until long-term alternative options are found.
Learn more about the principles of occlusion on implants in the webinar Biomechanical aspects of prosthetics on implants.
http://aegisdentalnetwork.com/
