CAD/CAM Technology for Restoration of Lower Jaw Teeth
Machine translation
Original article is written in RU language (link to read it) .
This case demonstrates how CAD/CAM technology was used to restore proper function and improve the aesthetics of the lower jaw teeth. The initial treatment plan involved installing implants to replace the lower right molars. However, it was changed due to a lack of space. The computer-aided design system was used for the digital creation and manufacturing of implant-supported/abutment lithium disilicate crowns and screw-retained hybrid abutment lithium disilicate crowns in a single visit.
Learn more about the technique automated design-milling (CAD/CAM) in the online course Ceramic Inlays. Complete Guide.

Preoperative diagnostics and planning strategy helped achieve a predictable result in one visit for a patient who traveled several hundred kilometers for help. Before her visit and treatment, studying her dental records revealed the presence of minimal interocclusal space, so the following treatment plan was developed: two implant-supported hybrid abutments/crowns with screw fixation. During digital scanning, it became clear that an alternative, more comprehensive treatment plan was needed to ensure the result in one visit. A team of three dentists who were involved in the treatment planning, another dentist responsible for the digital support of the process, and a Patterson dental specialist responsible for digital design and laboratory support, worked together. The bite height was increased, and the necessary space for restoring tooth 22 was created.
Clinical Case Review
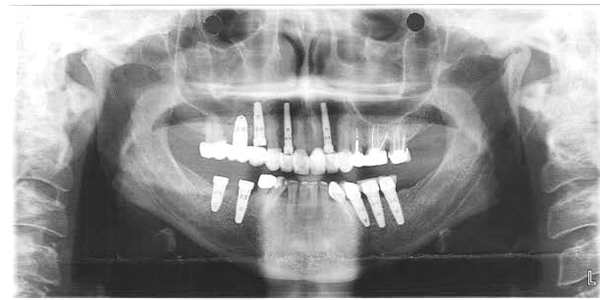
A 59-year-old patient traveled 500 kilometers to consult a dentist and receive the necessary treatment. Her upper dental arch was restored in 2012. The patient was fitted with temporary screws on implants №№ 30 and 31 (5.0 NobelReplace Select ™, Nobel Biocare, nobelbiocare.com). Given that the patient lived far away, it was decided to use digital scanning and milling to create restorations on implants №№ 30 and 31 in one visit.
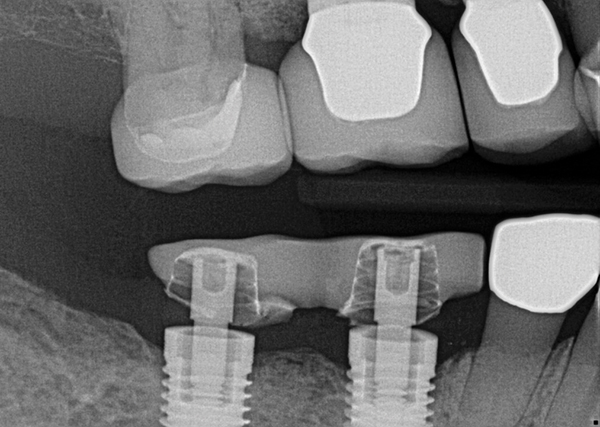
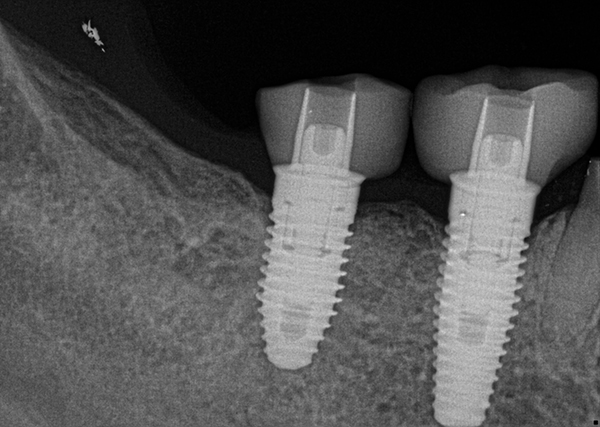
X-rays (figure 2) and emails from her regular dentist raised concerns about the lack of adequate interocclusal space for the final restorations. Due to limited space, hybrid abutments/crowns with screw retention were planned.
Diagnosis
Medical History
The patient is a somatically healthy 59-year-old woman who underwent an emergency hip replacement surgery in 2011. She regularly takes levothyroxine sodium and estradiol. She has a mild systemic disease without functional limitation (hypothyroidism).
Oral Health Status
The patient was satisfied with the condition of her oral cavity, having been treated by the same specialist for the last 4 years. There was slight gum recession, poor family periodontal history. The patient often had food stuck between her teeth and experienced tooth chipping. She noticed that her front teeth had become shorter and were significantly worn down over the last 5 years. She frequently used chewing gum and had worn a night guard over 6 years ago because her dentist thought she had bruxism. She was pleased with her smile after the restoration of her upper teeth in 2012 but was only concerned about the dark shade of her lower teeth and crowns. However, addressing this issue was not her urgent priority.
Diagnosis, Risk Assessment, and Prognosis
Periodontium: General horizontal resorption of less than 3 mm was noted, except for teeth Nos. 14 and 15, where it was 5mm.
Risk: medium
Prognosis: generally favorable
Biomechanics:
Except for teeth Nos. 23-26, all other teeth had been previously treated. Tooth loss, except for third molars and first premolars, was caused by biomechanical reasons. The upper dental arch was restored in 2012. Restorations of teeth Nos. 18, 22, and 29 were defective, and teeth Nos. 25 and 27 were questionable. Erosion of tooth No. 24.
Risk: high
Prognosis: Poor for teeth Nos. 14, 15, 18, 22, 27, and 29. Favorable for teeth Nos. 23-26.

Functionally: according to the patient, the lower front teeth had worn down over the last 5 years, but a 2008 photograph showed minimal changes. It was assumed that the tissue loss on teeth #23-27 was caused by erosion and physiological wear. The temporary restoration on implants #30 and #31 was thin; information about the original design and boundaries of the restoration is missing. The patient did not report any difficulties with chewing and had no dysfunction of the temporomandibular joint. Full range of TMJ movements, negative functional tests.

Risk: low
Prognosis: generally favorable
Treatment Plan
The treatment plan involved removing the temporary restorations on implants №№ 30 and 31, then designing and fabricating two restorations. If necessary, the occlusal height will be adjusted.
If an adjustment of the occlusal height is required, milled e.max® porcelain crowns (Ivoclar Vivadent, ivoclarvivadent.com) will be needed for implants №№ 18-20 and teeth №№ 22 and 29, made using CAD/CAM technology. For an efficient workflow, implants №№ 18-20 will be restored first, as completing these restorations will require less time than for the hybrid abutment crowns on implants № 30 and 31 with screw retention.
Treatment Sequence
Stage 1
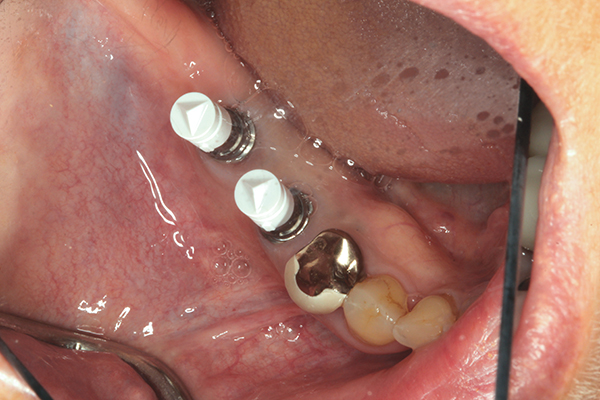
Treatment began with preoperative photography and clinical examination. After removing the lower right temporary structure and placing ScanPosts (Dentsply Sirona, sironausa.com) and ScanBodies (Dentsply Sirona), a digital image of both dental arches was obtained and the occlusion was registered. Using CEREC™ automated design (Dentsply Sirona), the space deficiency was compensated. Hybrid abutment crowns were modeled with the current occlusal height. It was decided to increase the area by raising the occlusal height, using the revised treatment plan. Then, the preliminary structure was screwed back onto implants № 30 and 31 to prevent tissue damage during treatment.

Stage 2
The second stage in creating cemented crowns with abutments on implants for teeth №№ 18-20. The existing crowns were removed, and the tissues were retracted with a retraction cord for better access. CEREC Omnicam (Dentsply Sirona) was used to capture digital images of the upper and lower left quadrants and to record the bite.

The crowns were manufactured using a CEREC block and e.max crowns, milled using CEREC MC XL (Dentsply Sirona) in a milling machine with CAD/CAM Technology. The milled crowns were tested in an uncrystallized state; contacts and occlusion were checked and adjusted as necessary. The crowns were given the necessary surface relief to match existing restorations followed by the application of a solid glaze layer and crystallization in a Programat oven (Ivoclar Vivadent). A 15-minute firing allows achieving the correct shade and significantly increases the flexural strength of the restoration to 400 MPa, which is more than 2.5 times higher compared to other ceramics.

After 5 minutes of cooling, the crowns are cleaned with steam; they are adjusted, their function and aesthetics are evaluated, and they are cemented onto the existing implants using Premier® Implant Cement ™ (Premier, premusa.com), which allows for reuse. On the left side, a correct, stable occlusion was established at the proper bite height.
Stage 3
Stage 3 involved hybrid abutment crowns on implants No. 30 and 31 with a screw-retained e.max crown on tooth No. 29. The temporary restoration on implants No. 30 and 31 was removed, and an impression was taken to obtain high-quality final restorations. Two ScanPosts were placed into the implants. The corresponding ScanBody was positioned over the ScanPost.
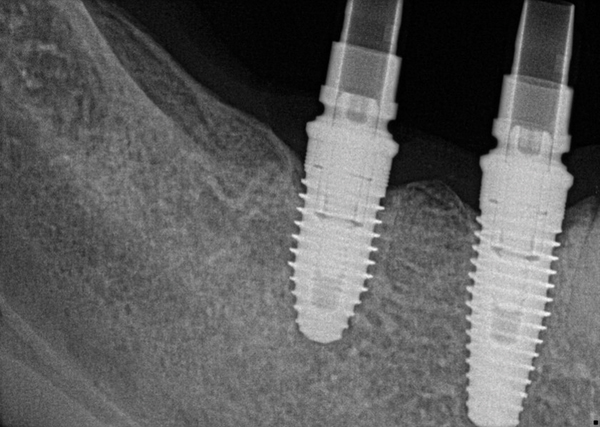
Similarly, on the right side, digital images of the upper and lower right quadrants were obtained and bite registration was performed. E.max restorations for #29-31 were manufactured using CAD/CAM technology.
The occlusion was checked to confirm bilateral, simultaneous, full contacts.
Stage 4
The final stage involved replacing the defective crown on tooth #22.
The final occlusion assessment was performed. Stable occlusion was confirmed using thin articulation paper. The patient was seated at a 45-degree angle. Minor adjustments were made, and the ceramics were polished. After the anesthesia wore off, the patient felt that she could fully bite and chew. The patient is satisfied with the treatment results both functionally and aesthetically.



Functional and Aesthetic Outcome
At any stage of the work, the dentist must be ready to change the treatment plan to avoid disappointing the patient. By combining rational principles of diagnostics and treatment planning with automated production technology, a systematic workflow can be developed that ensures a predictable and successful outcome. In this case, the result exceeded the expectations of both the patient and the doctor. In a single visit, occlusal relationships were restored. A functional and aesthetic outcome was achieved. The total treatment took about 6 hours. It has been 19 months since the treatment, and the result is stable.
Learn more about this topic at the webinar Combined Use of CAD/CAM Technologies and Manual Techniques for Applying Ceramic Masses.
http://aegisdentalnetwork.com/
