Structure of Periodontal Tissues
Machine translation
Original article is written in RU language (link to read it).
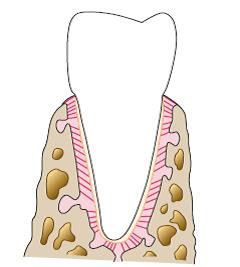
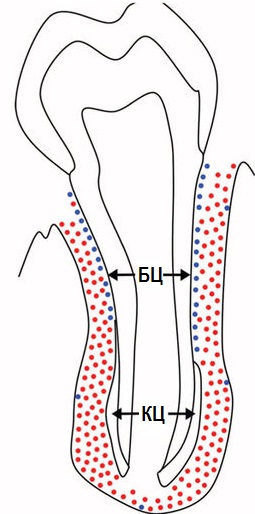
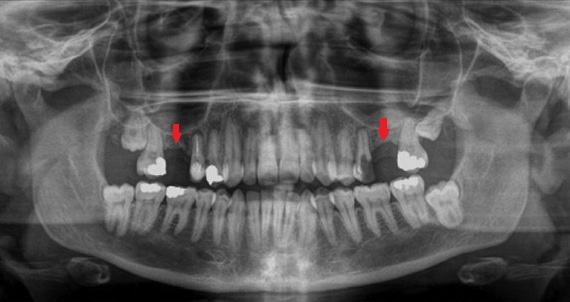
This article is dedicated to the structure of periodontal tissues. The structure of periodontal tissues. Highlighted in red in the image:
- gum;
- periodontal ligament;
- root cementum;
- alveolar bone.
Learn more about the periodontium and its treatment tactics at the webinar Periodontal Regeneration: GTR Technique.
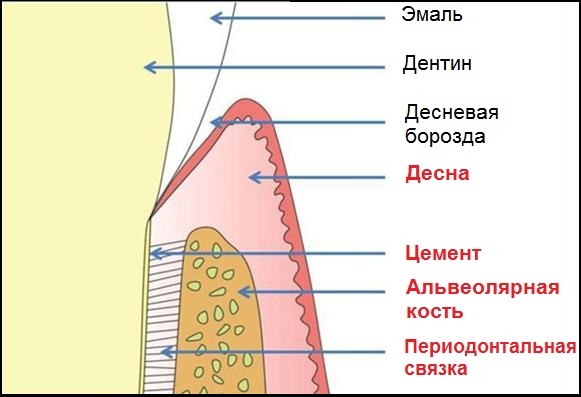
It is important that the gum and other periodontal tissues have different functions. The main role of the gum is protection. Protection of the underlying tissues from external influences. Cementum, alveolar bone, and the periodontal ligament together form what is called the "tooth-supporting apparatus." Thanks to these tissues, the main function of the periodontium is performed - to keep the tooth in its rightful place, in the socket.
Periodontal Ligament
The periodontal ligament is a connective tissue that surrounds the tooth and connects it to the inner wall of the alveolar bone.
It starts 1-1.5 mm below the cementoenamel junction.
It's hard to believe, but its width (on average) is only 0.2 mm. The clarification "on average" is explained not only by individual characteristics of the periodontal ligament in different people, but also by changes in the load on the tooth. The relationship is direct: the greater the load, the wider the ligament.
The main components of the periodontal ligament are:
- periodontal fibers;
- cells;
- intercellular (basic) substance;
- vessels, nerves.
The connective tissue of the gums has a similar composition:

The similarity is not accidental, as the periodontal ligament is an extension of the gum's connective tissue with its unique characteristics, which enable its unique function.
A few words about each of the components of the periodontal ligament.
Periodontal fibers
The majority of periodontal fibers are made of type I collagen. It is synthesized in fibroblasts. Then, tropocollagen molecules are formed, which create microfibrils, then fibrils, threads, and bundles:
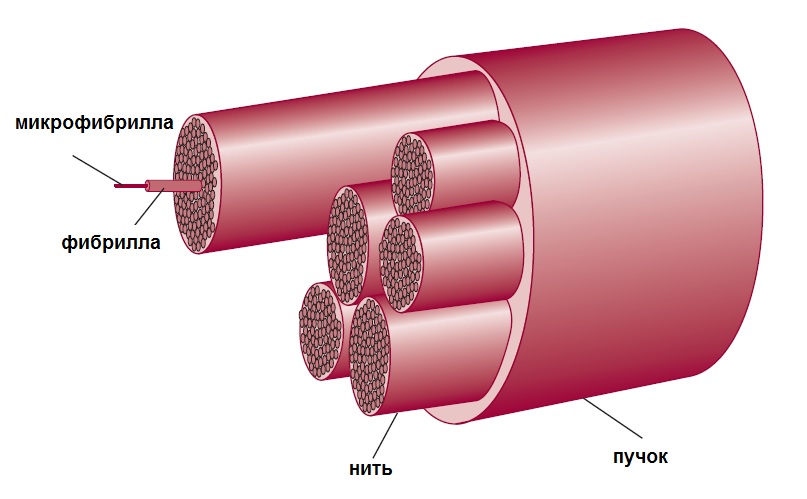
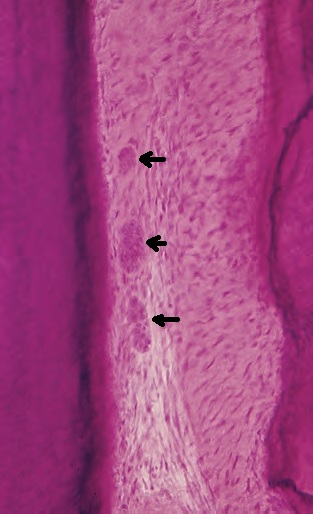
This structure of collagen fibers allows them to be both strong and flexible. In a longitudinal section, they have a wavy shape:
As in the case of the gingival fibers, numerous classifications of periodontal fibers have been proposed. According to one, there are 6 groups of periodontal fibers:
- transseptal;
- alveolar crest fibers;
- horizontal;
- oblique;
- apical;
- interradicular (between the roots).
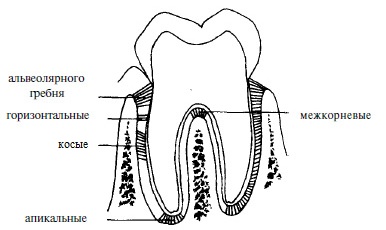
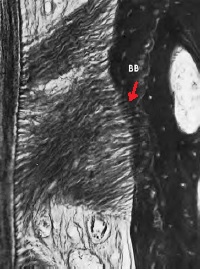
The term "Sharpey's fibers" is also often encountered in the literature, but this is not another group. These are the terminal, partially or fully calcified parts of periodontal fibers from all 6 groups, which interweave, penetrate the cementum and alveolar bone. Additionally, Sharpey's fibers are associated with non-collagenous proteins (osteopontin, bone sialoprotein) in the bone and cementum (red arrow in the image), which provides such a strong connection.
Transseptal Fibers
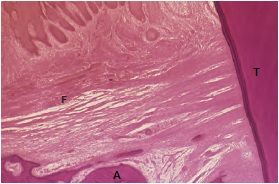
Transseptal fibers (F) run over the alveolar ridge (A) and connect two adjacent teeth (T). They are often referred to as gingival fibers and do not interweave into the bone.
Alveolar Crest Fibers
They originate in the area of the tooth root cementum just below the attachment epithelium, go obliquely, and attach to the alveolar crest or periosteum.
Horizontal, oblique, and apical fibers also extend from the cementum to the bone. The difference is in the angle at which they are directed and in which part of the periodontal ligament they are located. Horizontal fibers are positioned at a right angle closer to the edge of the tooth socket, apical fibers are in the area of the root apex. Oblique fibers are between them, and they are the most numerous. They bear the vertical load that occurs during chewing and "transfer" it to the bone.
Inter-radicular fibers (as the name suggests) pass between the roots of a multi-rooted tooth (from the furcation) to the bone.
In addition to the main groups in the periodontal ligament, there are also other, less organized collagen and elastic fibers. Elastic fibers are mainly located parallel to the tooth in the cervical third of the root. They regulate blood flow in the vessels of the ligament.
The fibers of the periodontium are constantly renewed thanks to the work of cellular elements.
Periodontal Cells
Periodontal cells include:
- connective tissue cells;
- Malassez epithelial rests;
- defensive cells (neutrophils, lymphocytes, macrophages, eosinophils, mast cells);
- cellular elements of nerves, vessels.
Connective tissue cells are mainly fibroblasts, which synthesize collagen. They are also capable, if necessary, of protective reactions – phagocytosis, hydrolysis.
Closer to the bone, osteoblasts and osteoclasts, cementoclasts, -blasts, odontoclasts are found near the tooth.
Malassez epithelial rests – remnants of epithelium embedded next to the cementum, which were destroyed during tooth eruption. Overall, their role has not yet been studied. It is only known that with age, they may either disappear without a trace or turn into cementicles or cysts.
The main substance fills the space between cells and fibers. Its main difference from the intercellular substance of the adjacent gingival connective tissue is the possible presence of cementicles. They can attach to the tooth (1) or freely exist in the ligament (2):
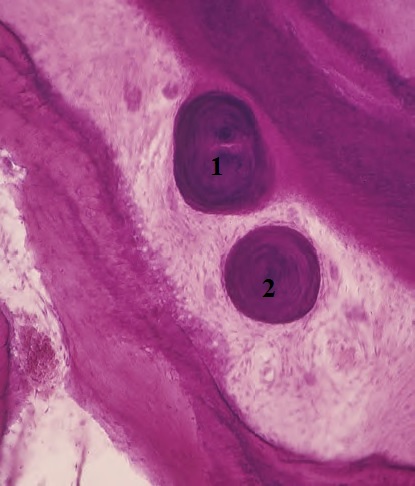
We already know that they can form from Malassez epithelial rests. But there are other sources of their development, for example:
- particles of cement or bone;
- Sharpey's fibers;
- calcified blood vessels.
The periodontal ligament is a key component of the periodontium. It is responsible for most of its functions. We will talk about the functions later, but for now, let's move on.
Tooth Cementum
Cementum covers the root of the tooth externally. It consists of
- collagen fibers and
- calcified intercellular substance.
- (+ cells).
There are no vessels in the cementum.
External fibers – Sharpey's, from the periodontal ligament, are distinguished. And the internal ones, which are directly formed in the cementum by cementoblasts, as well as the intercellular substance.
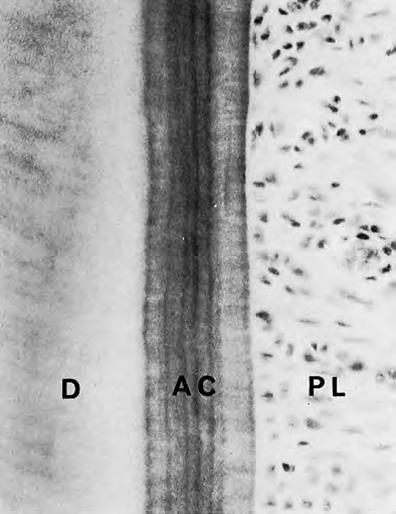
Cells in cement are not present everywhere. Where they are – there is cellular cement (CC). Where they are not – there is acellular cement (AC).
Acellular Cement
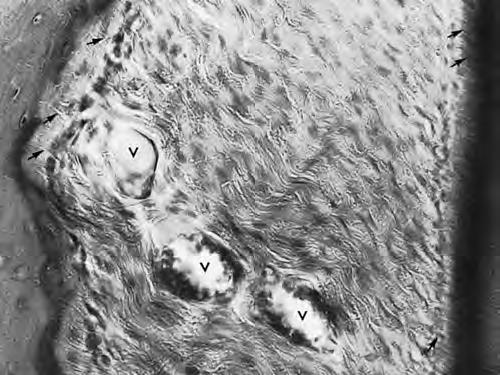
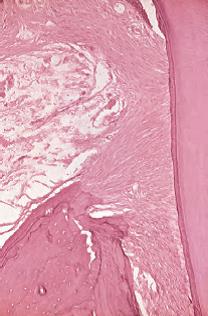
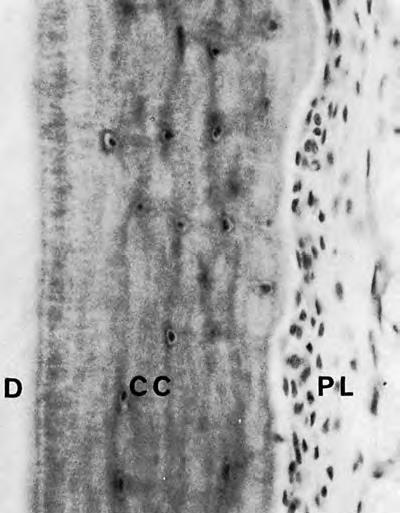
Acellular cement is also called primary. It forms earlier than cellular cement and until the tooth reaches its antagonist, does not come into occlusion. It covers the root up to halfway (from the crown towards the apex). In the image, AC – acellular cement, is located between the dentin (D) and the periodontal ligament (PL). You can notice that it is "striped". These stripes, like rings on a cross-section of a tree trunk, indicate the periods of cement formation.
Cellular Cement
Cellular cement is formed after the tooth reaches the occlusal plane. It is found in the apical third of the root and in the bifurcation area. Cellular cement is less mineralized and contains fewer Sharpey's fibers. In it (CC), individual spaces (lacunae) with cementocytes inside are found. Cementocytes are interconnected through special canaliculi. Note the cluster of cells in the ligament (PL). These are none other than cementoblasts:
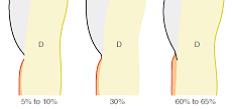
From the illustrations, it is noticeable that the width of the cement is greater towards the apical part of the root (approximately from 0.1 to 1 mm). The age-related pattern is interesting: in a 70-year-old, the cement is three times wider than in an 11-year-old child.
Cement connects with enamel in different ways:
- there is a gap between them (sensitivity may be a concern);
- it connects edge-to-edge;
- it overlaps the enamel.
Compared to enamel, cement is much less mineralized. Cement is generally "the softest" among the hard tissues of the dental system: it contains only about 50% hydroxyapatite. This figure is small compared to bone (65%), dentin (70%), and enamel (97%).
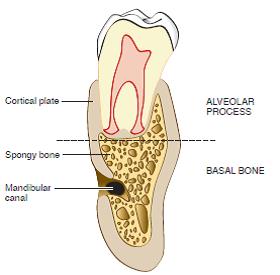
Alveolar Bone
The alveolar bone is part of the alveolar process of the upper and the alveolar part of the lower jaw. It is located just below the enamel-cement junction (by 1-1.5 mm).
The alveolar bone consists of:
- the actual alveolar bone – forms the wall of the tooth socket, surrounds the tooth. It serves as a support for the periodontal ligament, into which Sharpey's fibers are embedded. It has numerous openings – Volkmann's canals, through which nerves and vessels pass.
- the supporting alveolar bone – cancellous substance covered with an outer plate of compact substance. The outer cortical plate covers the bone externally. It consists of osteons and is connected to the periosteum.
In the spongy substance, initially in childhood, there is red bone marrow: many blood vessels needed for jaw growth. With age, it is replaced by inactive yellow bone marrow. There is very little spongy substance on the oral and vestibular surfaces, the main mass is located near the apexes and between the roots.
Beneath the alveolar is the basal bone, which is not connected to the teeth at all.
The alveolar bone consists of
- 2/3 inorganic material (hydroxyapatite)
- 1/3 organic (collagen fibers, proteins, growth factors).
Main cells: osteoblasts, -cytes, -clasts.
Osteocytes are embedded in lacunae similar to cementocytes.
Osteoblasts create osteoid – unmineralized bone, which over time "matures" and becomes mineralized.
Osteoclasts are responsible for the resorption of bone tissue. Using enzymes, they cause the breakdown of the organic matrix, followed by the sequestration of mineral ions.
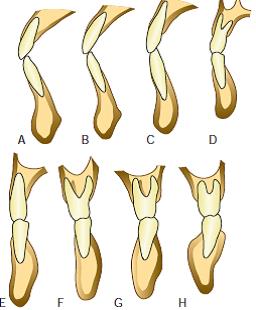
Bone is a "tooth-dependent" structure. It forms when a tooth erupts, and disappears when it is gone:
Also, interdental septa are identified as a separate topographic zone. Essentially, this is spongy bone, which is bordered on both sides by cortical plates of the dental alveolus. Depending on the distance between the teeth, their shape varies: from pointed (white arrow) to trapezoidal (red arrow).
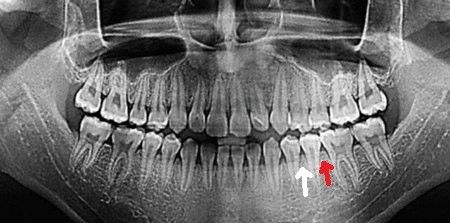
It is also interesting that in some areas near the tooth, there may normally be no bone, or there may be a bone pathology. The defect sometimes reaches the edge of the bone:

The structure of the periodontal tissues is determined by the important functions they perform. Disruption of the integrity of such a complex leads to periodontal diseases, and conversely, diseases destroy periodontal tissues.
Up-to-date information on the treatment of periodontal diseases in the online course Advanced Treatment of Periodontal Diseases.


