The Minimally Invasive Restorative Approach (MIRA): A 10-Step protocol
Abstract
This article describes a step-by-step protocol for obtaining predictable and repeatable outcomes in adhesive restorative treatment planning. The key elements of the protocol, which the authors call the Minimally Invasive Restorative Approach (MIRA), are to identify patients’ expectations, evaluate risk factors, establish proper communication between the interdisciplinary team and the laboratory technician, previsualize the desired result, and utilize tools to effectively guide the clinical procedures. This straightforward protocol is designed to help clinicians achieve the desired outcome in restorative cases at all levels of complexity.
You have the opportunity to gather more in-depth information about MIRA approach in our course "Indirect restoration in the biomimetic concept".
Introduction
One of the most challenging procedures in restorative dentistry is to reestablish compromised structures’ function and esthetics through the use of biocompatible restorations, either direct or indirect. Esthetic and functional results can be achieved with a variety of restorative treatments; the decision about which to use for individual cases should be driven by the treatment’s ability to preserve as much of the natural tooth structure’s quantity and quality as possible while still ensuring predictable outcomes.
Thanks to continually evolving restorative materials and adhesive technology, prosthetic restorations in the form of laminate veneers, sectional veneers, inlays, onlays, overlays, and full-coverage crowns can be bonded onto both natural dental tissue and manufactured materials with minimal or no tooth preparation. To achieve the desired outcome and minimize the risk of errors in planning, the details of the treatment plan must be discussed with the interdisciplinary team and an effective line of communication established with the laboratory technician before commencing the clinical procedures.
Computer-aided design/computer-aided manufacturing (CAD/CAM) technologies offer several advantages in terms of patient comfort and the efficacy, efficiency, and predictability of treatments. CAM fabrication has improved several mechanical properties of the materials used in fixed prosthodontics.
More digital protocols of total rehabilitation you can find on our website.
However, whether optical properties also have been enhanced is less clear when comparing CAM blocks to layered ceramics (Figs 1a-1h). Nevertheless, there are still various clinical and laboratory workflows available for restorative procedures; the decision about which to use depends on the desired final outcome. Analog, digital, and hybrid working systems are all valid, but because some are more appropriate in certain clinical situations, the advantages and disadvantages of each must be considered during the selection process (Figs 2a-2g). The following straightforward step-by-step protocol is intended to help clinicians achieve the desired outcome in restorative treatments at all levels of complexity.



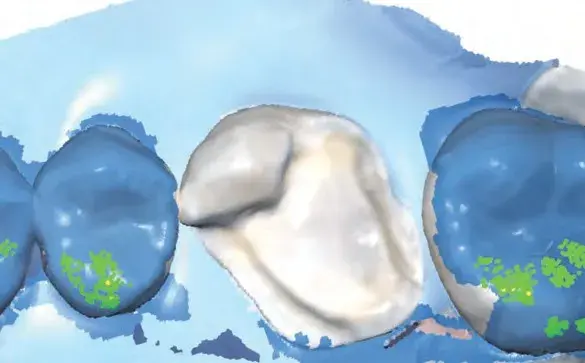
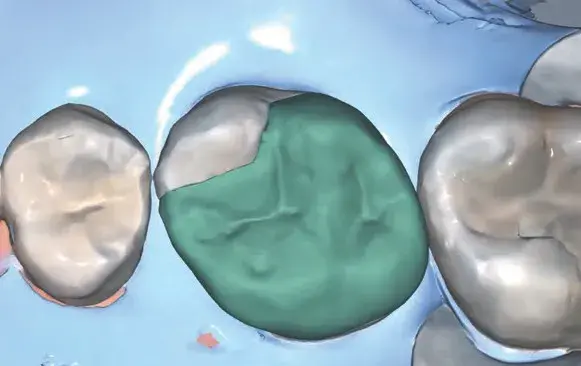


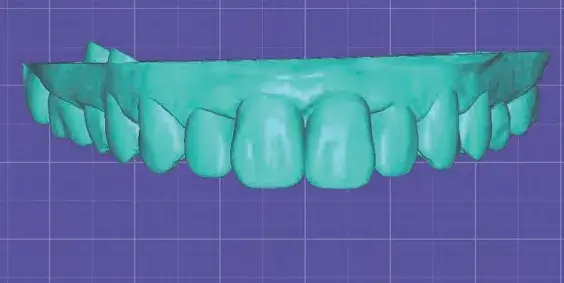
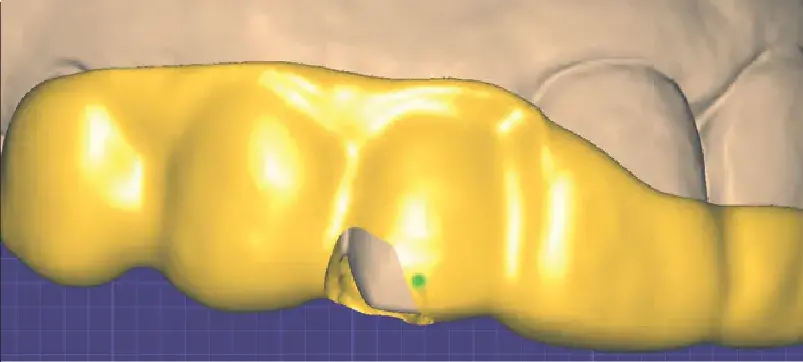
 Figures 1a-1h: (a) Stereolithography (STL) view of dental preparation; (b) initial situation; (c) tooth preparation; (d) prosthetic space analysis; (e) restoration design; (f) lithium disilicate milled restoration; (g) cementation; and (h) final situation.
Figures 1a-1h: (a) Stereolithography (STL) view of dental preparation; (b) initial situation; (c) tooth preparation; (d) prosthetic space analysis; (e) restoration design; (f) lithium disilicate milled restoration; (g) cementation; and (h) final situation.





 Figures 2a-2g: Views of (a) initial situation; (b) residual substrate after restoration removal; (c) feldspathic layered restoration; (d) restoration try-in; (e, f) final result; (g) feldspathic restoration.
Figures 2a-2g: Views of (a) initial situation; (b) residual substrate after restoration removal; (c) feldspathic layered restoration; (d) restoration try-in; (e, f) final result; (g) feldspathic restoration.
The Minimally Invasive Restorative Approach (MIRA)
The MIRA concept’s purpose is to guide clinicians through a 10-step protocol to ensure predictable and repeatable outcomes in adhesive restorative treatments. Each step is detailed here.
Step 1: Patient Profile
An accurate diagnosis is essential to treatment success. Early detection of any systemic and dental problems significantly influences the overall treatment plan. Prior to the clinical examination, validated questionnaires are useful for collecting the patient’s medical history and self-declared dental condition data, which help to identify their expectations and psychological profile.
Throughout the clinical examination, the objective is to categorize the individual patient under groups of risk factors, such as the following:
- periodontal
- biomechanical
- functional (In patients with compromised dental structure and loss of vertical dimension of occlusion [VDO], an appropriate VDO must be registered to guide the forthcoming wax-up to determine the final treatment plan. Several techniques are described in the literature to obtain a repeatable occlusal scheme by means of a jig, leaf gauges, or deprogram splint devices.)
- dentofacial.
Step 2: Treatment Plan
Outcome predictability, efficient communication among specialists, and patient satisfaction are the main benefits of establishing a correct treatment plan and sequence. During the initial visit, the collected data must first be analyzed and processed by creating a set-up and/or wax-up to establish and communicate the definitive treatment plan to the patient. The wax-up and the clinical and radiographic examinations will guide the interdisciplinary team through the tooth-by-tooth prognosis in terms of the prosthetic criteria. For this purpose, team meetings are strongly recommended (Figs 3a-3e).
The treatment phases can be classified into four steps:
- biological: periodontal, endodontic, operative (e.g., caries removal), and restorative (e.g., buildup, deep margin elevation) therapy
- functional: orthodontic therapy, maxillofacial surgery, and implant placement
- esthetic: prosthetic intervention
- maintenance: biological, functional, and esthetic follow-up.




 Figures 3a-3e: Views of (a, b) initial situation; (c) retracted intraoral; (d) retracted maxillary arch; and (e) analog wax-up.
Figures 3a-3e: Views of (a, b) initial situation; (c) retracted intraoral; (d) retracted maxillary arch; and (e) analog wax-up.
Step 3. Mock-Up and Prototype
A diagnostic mock-up allows the clinician to effectively communicate the final esthetic outcome to the patient to facilitate treatment acceptance, assess the design of final restorations, and predict the restorations’ impact on lip position, smile line, and masticatory function.
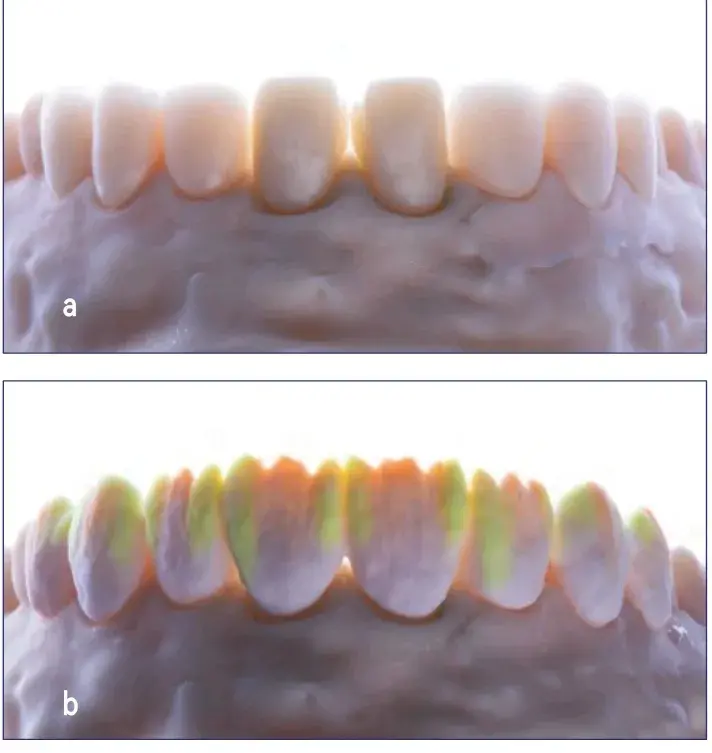
Digital workflows offer several advantages in terms of previsualizing the final result by means of smile design software, material thickness control, mandibular movement recording, and fabrication of CAD/CAM temporaries (3D printing). Digital workflows also enable more accurate recording of clinical corrections to the proposed wax-up design by intraorally scanning the adapted mock-up (Figs 4a & 4b).

 Figures 4a & 4b: Intraoral retracted views of mock-up.
Figures 4a & 4b: Intraoral retracted views of mock-up.
Step 4. Clinician-Technician Communication
To help ensure the desired outcome, all technical aspects of the interdisciplinary treatment must be discussed with the technician prior to initiating any clinical procedures.
The main aspects to be considered are as follows:
- Workflow to be adopted (i.e., analog, hybrid, digital).
- Information and documentation required by the laboratory technician, such as:
- baseline casts (either analog or digital impressions)
- intermaxillary position
- approved wax-up
- extraoral and intraoral photography protocols (e.g., camera settings, white balance, lighting set-up)
- color matching of initial situation and for preparation day (e.g., gray card, polarized filter, shade selection protocol, standard shade guide, customized ceramic specimens).
- Material selection based on the functional and esthetic requirements, which will determine the workflow for the final impression-making and technical fabrication procedures.
- Timeline for preparations, technical sequence, and cementation based on the patient’s requirements.
Control of each of these aspects reduces the risk of planning errors and helps in the fulfillment of technical requirements (e.g., sufficient prosthetic space availability, shade matching, and marginal fitting).
Step 5. Interim Prosthesis
The main goal of this phase is to assess function and esthetics. Resin materials allow for biological integration to test functionality and to evaluate the restorations’ esthetics. Based on the chosen workflow, temporaries will be manufactured using either an analog or a digital process. It is essential to have a thorough understanding of the durability and flexural strength of the materials selected for the interim prosthesis in order to manage the requirements of long-term provisional restorations or wide-span ridge rehabilitation.
Before proceeding to the preparations and final restorations, certain elements must be assessed; they are as follows:
- periodontal health of the soft tissues surrounding the interim prosthesis
- proper contact points with adjacent teeth
- occlusal integration
- final teeth shapes and contours.
Step 6. Preparation Design
Adequate assessment of healthy tooth structure preservation and affected substrate reduction is key for the success of adhesive restorations. Several preparation designs have been described in the literature to ensure minimal restoration thickness based on the residual healthy tooth structure, the available thickness, the esthetic criteria, the material to be used, and the occlusal pattern. To increase predictability in tooth reduction, it is advisable to use the mock-up as a reference and to adopt preparation guides for thickness control while preparing. The guides can be fabricated either with an analog process, using silicone or ethylene vinyl acetate material, or with a CAD workflow using 3D printable resin. Finally, prior to impression-making, mandatory adhesive procedures must be performed immediately after tooth preparation to guarantee dentin sealing; this will reduce tooth sensitivity and enhance the subsequent adhesive cementation of the final restoration (Figs 5a & 5b).

 Figures 5a & 5b: Views of (a) prosthetic space assessment with silicone guides and (b) tooth preparation.
Figures 5a & 5b: Views of (a) prosthetic space assessment with silicone guides and (b) tooth preparation.
Step 7. Impressions
The impression-making sequence must be set with the laboratory technician prior to dental preparation. Regardless of the selected operational workflow (i.e., analog, hybrid, or digital), it is advisable to take careful note of key pre-impression procedure checklist items: clearly visible and sharp margins, absence of undercuts, absence of contact between cavity and adjacent teeth, accessibility of subgingival margins, and adequate interocclusal space. Pre-preparation impressions are a useful tool to assess the modifications from the designed wax-up to the adapted mock-up/interim prosthesis, which serves as a functional guide for the definitive restoration (Fig 6).
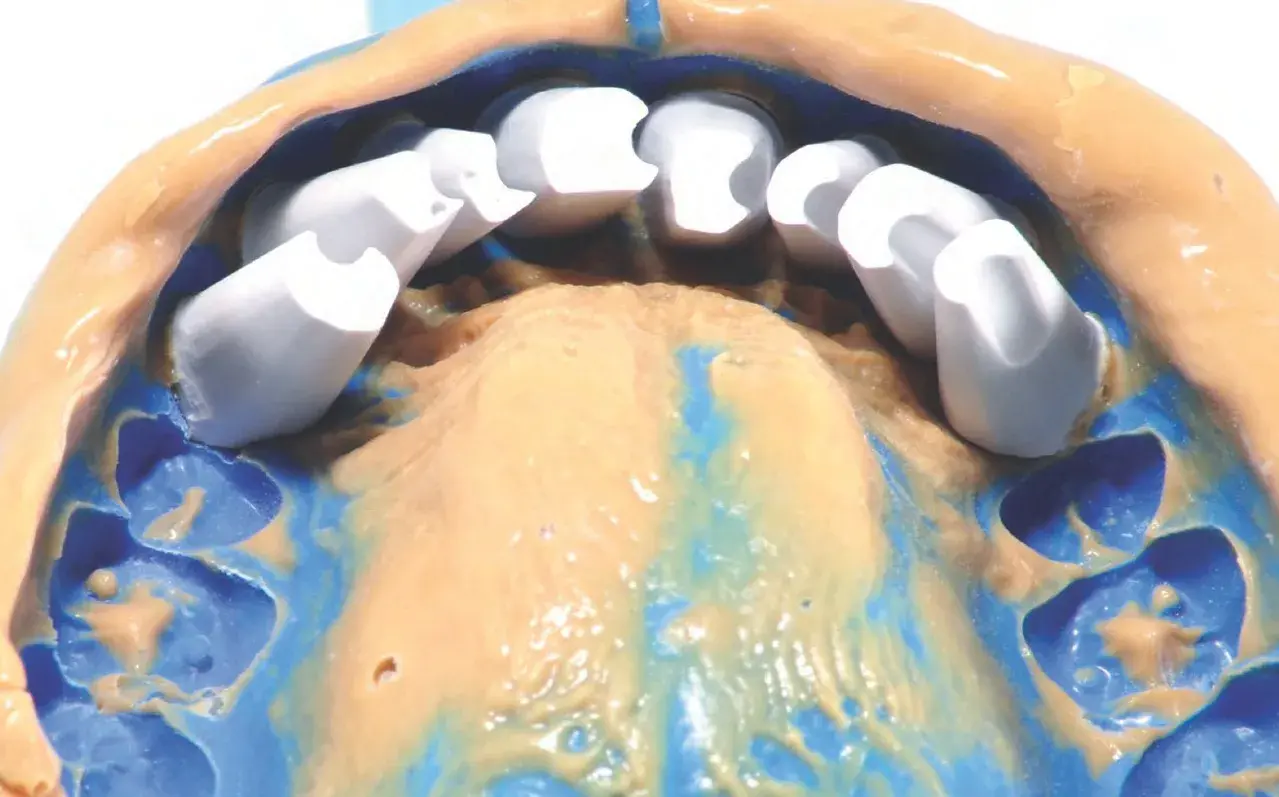 Figure 6: Polyvinyl siloxane impression for alveolar model fabrication.
Figure 6: Polyvinyl siloxane impression for alveolar model fabrication.
Step 8. Laboratory Procedure and Try-In
The main characteristics to be observed in a definitive restoration try-in are marginal fit by visual/tactile assessment and/or with fit checker pastes, intaglio fitting, interproximal and interocclusal contact, and esthetic integration (e.g., core color, secondary and tertiary anatomy, and characterizations). If there are diverse substrate colors, it is recommended to achieve chromatic uniformity with the restorations only. However, if slight compensations are needed, a wet try-in with appropriate pigmented resins could be useful (Figs 7a-7d)



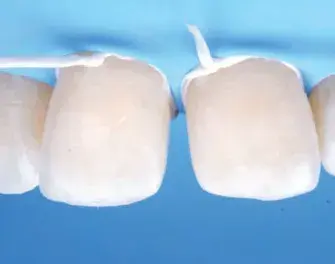
 Figures 7a-7d: Views of (a) layered feldspathic ceramic; (b) final restorations fabricated; (c) detail of feldspathic porcelain restoration; and (d) intraoral try-in.
Figures 7a-7d: Views of (a) layered feldspathic ceramic; (b) final restorations fabricated; (c) detail of feldspathic porcelain restoration; and (d) intraoral try-in.
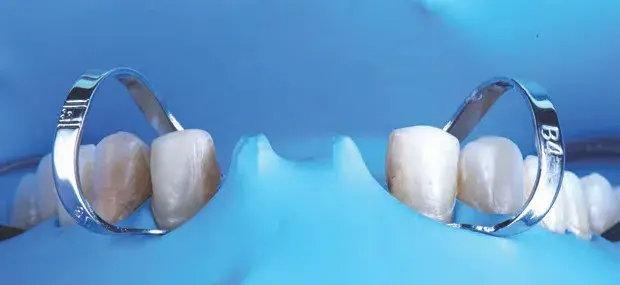
Step 9. Cementation
Tooth–restoration sealing is the goal of adhesive cementation procedures. A dental dam is mandatory for this process; absolute isolation techniques have been developed to guarantee humidity reduction, saliva and blood physical barrier, and a stress-free working environment. Selection of cementation material depends mainly on the restoration’s optical properties and thickness to allow light-induced curing luting agents to act or drive the decision toward dual- or auto-curing resin cements. Protocols for substrate and restoration adhesive conditioning differ depending on the combination of material and cement. However, occlusal adjustments and finishing and polishing of the interface between the tooth and the restoration are essential for long-term stability (Figs 8a-8c).


 Figures 8a-8c: Frontal views of (a) split dam isolation; (b) cemented restorations (Variolink LC, Ivoclar Vivadent; Amherst, NY), maxillary arch; and (c) final result.
Figures 8a-8c: Frontal views of (a) split dam isolation; (b) cemented restorations (Variolink LC, Ivoclar Vivadent; Amherst, NY), maxillary arch; and (c) final result.
Step 10. Maintenance
Patient recall, including professional maintenance as well as at-home maintenance regimens, is mandatory for patients with tooth- and implant-supported restorations, regardless of the case’s level of complexity. It is advisable to follow clinical practice guidelines as established by the American College of Prosthodontists (Figs 9a-16c).


 Figures 9a-9c: Views of (a, b) final result; and (c) bite splint.
Figures 9a-9c: Views of (a, b) final result; and (c) bite splint.


 Figures 10a-10c: Views of (a) initial situation; (b) intraoral scan; and (c) digital wax-up.
Figures 10a-10c: Views of (a) initial situation; (b) intraoral scan; and (c) digital wax-up.

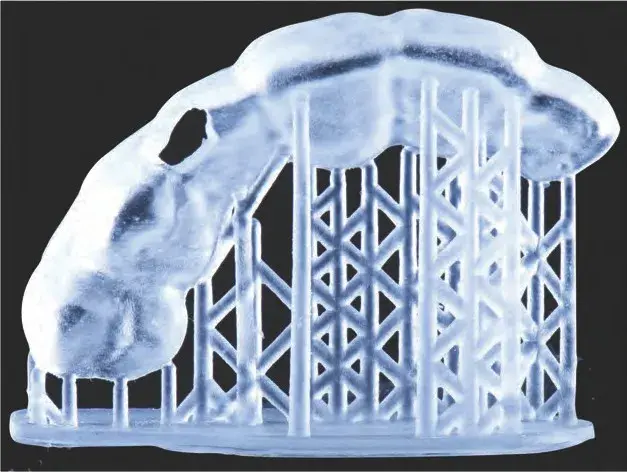
 Figures 11a & 11b: Mock-up: (a) 3D printed wax-up models; and (b) full-face view.
Figures 11a & 11b: Mock-up: (a) 3D printed wax-up models; and (b) full-face view.
 Figures 12a-12c: Views of selective tooth preparation guide: (a) CAD; (b) 3D printed splint; and (c) intraoral fit check.
Figures 12a-12c: Views of selective tooth preparation guide: (a) CAD; (b) 3D printed splint; and (c) intraoral fit check.
 Figure 13a: Images of 3D printed preparation guides for prosthetic space assessment.
Figure 13a: Images of 3D printed preparation guides for prosthetic space assessment.


 Figures 13b-13d: Views of tooth preparation guided by the mock-up: (b) mock-up in place; (c) preparation thickness control; and (d) intraoral scan of final preparation.
Figures 13b-13d: Views of tooth preparation guided by the mock-up: (b) mock-up in place; (c) preparation thickness control; and (d) intraoral scan of final preparation.
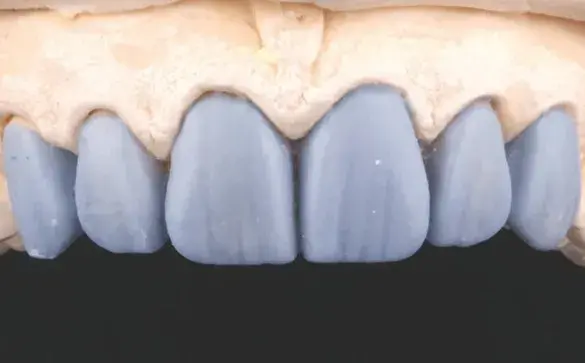
 Figures 14a-14c: Views of lab procedure: (a) milled lithium disilicate core for veneers and zirconia core for central incisor crowns; (b) ceramic layering; and (c) final restorations fabrication, detail.
Figures 14a-14c: Views of lab procedure: (a) milled lithium disilicate core for veneers and zirconia core for central incisor crowns; (b) ceramic layering; and (c) final restorations fabrication, detail.


 Figures 15a-15d: Views of cementation procedure: (a) absolute isolation; (b) cemented restorations under absolute isolation (Variolink LC); (c) central incisors try-in and subsequent cementation (Panavia V5, Kuraray; New York, NY); and (d) final result.
Figures 15a-15d: Views of cementation procedure: (a) absolute isolation; (b) cemented restorations under absolute isolation (Variolink LC); (c) central incisors try-in and subsequent cementation (Panavia V5, Kuraray; New York, NY); and (d) final result.


 Figures 16a-16c: Views of final result: (a) retracted intraoral; and (b & c) extraoral.
Figures 16a-16c: Views of final result: (a) retracted intraoral; and (b & c) extraoral.
Summary
The authors believe that the meaning of “minimally invasive” treatment needs to be redefined, with the focus shifting from solely striving to conserve healthy tooth structure even at the cost of failing to take into account the possible mechanical and physical consequences for both the tooth and the restoration. Instead, the primary goal should be to ensure predictability in every treatment. The MIRA concept offers clinicians a protocol that can be utilized for all cases regardless of the level of complexity. The authors recognize that the steps described in this article involve a high degree of technique sensitivity in terms of the treatment plan, preparation design, adhesive procedures, and final static and dynamic occlusal adjustments. However, the planning, coordination, preparation, and skill invested in obtaining predictable outcomes is well worth it.
Effective collaboration and communication among clinicians, interdisciplinary teams, and dental technicians will likely lead to better adherence to proper treatment protocols, thereby increasing the probability of achieving successful functional and esthetic outcomes for all restorative treatments.
Further information about indirect restoration you can get in our course "Ceramic veneers: the most demanded protocols in one place".
Author information
Dr. Torres is an assistant professor in the Department of Prosthodontics and Implantology at La Salle Bajío University School of Dentistry in León, Mexico. He has a private practice in León, Mexico.
Dr. Caponi is an associate professor in the Department of Restorative Dentistry at the International University of Catalonia School of Dentistry in Barcelona, Spain. He has a private practice in San Benedetto del Tronto, Italy.
Dr. Strimling has a private practice in Mexico City, Mexico.
References
- Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955 Dec;34(6):849-53.
- Browet S, Gerdolle D. Precision and security in restorative dentistry: the synergy of isolation and magnification. Int J Esthet Dent. 2017;12(2):172-85.
- Blatz MB, Conejo J. The current state of chairside digital dentistry and materials. Dent Clin North Am. 2019 Apr;63(2):175-97.
- Rekow ED. Digital dentistry: the new state of the art—is it disruptive or destructive? Dent Mater. 2020 Jan;36(1):9-24.
- Gamer S, Tuch R, Garcia LT. M.M. House mental classification revisited: intersection of particular patient types and particular dentist’s needs. J Prosthet Dent. 2003 Mar;89(3):297-302.
- Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001 Mar; 22(3):199-206.
- Kois DE, Kois JC. Comprehensive risk-based diagnostically driven treatment planning: developing sequentially generated treatment. Dent Clin North Am. 2015 Jul;59(3):593-608.
- Calamita M, Coachman C, Sesma N, Kois J. Occlusal vertical dimension: treatment planning decisions and management considerations. Int J Esthet Dent. 2019;14(2)166-81.
- Zitzmann NU, Krastl G, Hecker H, Walter C, Waltimo T, Weiger R. Strategic considerations in treatment planning: deciding when to treat, extract, or replace a questionable tooth. J Prosthet Dent. 2010 Aug;104(2):80-91.
- Marzola R, Derbabian K, Donovan TE, Arcidiacono A. The science of communicating the art of esthetic dentistry. Part I: patient-dentist-patient communication. J Esthet Dent. 2000;12(3):131-8.
- Heinsohn JPS, Arteaga EM, Rivera GJ, Stange VB. Mock-up. an old tool renewed. J Clin Res Dent. 2018;1(1):1-5.
- Scotti Nicola. New adhesives and bonding techniques. Why and when? Intl J Esthet Dent. 2017;12(4):524-35.
- Magne P, Spreafico RC. Deep margin elevation: a paradigm shift. Am J Esthet Dent. 2012;2(2):86-96.
- Magne P. Immediate dentin sealing: a fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005 May;17(3):144-54.
- Magne P, So WS, Cascione DS. Immediate dentin sealing supports delayed restoration placement. J Prosthet Dent. 2007 Sep;98(3):166-74.
- Veneziani M. Posterior indirect adhesive restorations: updated indications and the morphology driven preparation technique. Int J Esthet Dent. 2017 Jan;12(2):204-30.
- Gürel G. Porcelain laminate veneers: minimal tooth preparation by design. Dent Clin North Am. 2007 Apr;51(2):419-31.
- Hedelhoff D, Prandtner O, Saeidi Pour R, Liebermann A, Stimmelmayr M, Güth JF. Anterior restorations: the performance of ceramic veneers. Quintessence Int. 2018;49(2):89-101.
- Shillingburg HT, Sather DA, Wilson EL, Cain JR, Mitchell DL, Blanco LJ, Kessler JC. Fundamentals of fixed prosthodontics. Hanover Park (IL): Quintessence Pub.; 2012.
- Goodacre CJ, Campagni WV, Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 2001 Apr;85(4):363-76.
- Magne P, Belser UC. Novel porcelain laminate preparation approach driven by a diagnostic mock-up. J Esthet Restor Dent. 2004 Jan;16(1):7-16.
- Vailati F, Belser UC. Full-mouth adhesive rehabilitation of a severely eroded dentition: the three-step technique. Part 1. Eur J Esthet Dent. 2008 Spring;3(1):30-44.
- Ammannato R, Ferraris F, Marchesi G. The “index technique” in worn dentition: a new and conservative approach. Int J Esthet Dent. 2015 Spring;10(1):68-99.
- Schlichting LH, Resende TH, Reis KR, Magne P. Simplified treatment of severe dental erosion with ultrathin CAD-CAM composite occlusal veneers and anterior bilaminar veneers. J Prosthet Dent. 2016 Oct;116(4):474-82.
- Caponi LQ, Taha Y, Gutierrez N, Roig C M. Silicone key device for maxilla orientation and occlusal plane recording in a digital workflow. J Prosthet Dent. 2021 May 25;S0022-3913(21)00220-1. doi: 10.1016/j.prosdent.2021.04.010. Epub ahead of print.
- Caponi L, Raslan F, Roig M. Fabrication of a facially generated tooth reduction guide for minimally invasive preparations: a dental technique. J Prosthet Dent. 2021 Jan;:S0022-3913(20)30755-1. doi: 10.1016/j.prosdent.2020.11.030. Epub ahead of print.
- Ting-Shu S, Jian S. Intraoral digital impression technique: a review. J Prosthodont. 2015 Jun;24(4):313-21.
- Mocelin RC, Penteado MM, Pierre FZ, Saraiva ACV, Uemura ES, da Silva JMF. Assessment of patient and dentist preference between conventional and digital diagnostic waxing. Int J Esthet Dent. 2021 Aug;16(3):300-9.
- Joda T, Ferrari M, Gallucci GO, Wittneben JG, Brägger U. Digital technology in fixed implant prosthodontics. Periodontol 2000. 2017 Feb;73(1):178-92.
- Revilla-León M, Sánchez-Rubio JL, Besné-Torre A, Özcan M. A report on a diagnostic digital workflow for esthetic dental rehabilitation using additive manufacturing technologies. Int J Esthet Dent. 2018;13(2):184-96.
- Stanley M, Paz AG, Miguel I, Coachman C. Fully digital workflow, integrating dental scan, smile design and CAD-CAM: case report. BMC Oral Health. 2018 Aug 7;18(1):134.
- Davidowitz G, Kotick PG. The use of CAD/CAM in dentistry. Dent Clin North Am. 2011 Jul;55(3):559-70.
- Mangano F, Shibli JA, Fortin T. Digital dentistry: new materials and techniques. Int J Dent. 2016;5261247. doi: 10.1155/2016/5261247. Epub 2016 Oct 20.
- Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016 Oct;37(9):611-7; quiz 618.
- Bidra AS, Daubert DM, Garcia LT, Gauthier MF, Kosinski TF, Nenn CA, Olsen JA, Platt JA, Wingrove SS, Chandler ND, Curtis DA. A systematic review of recall regimen and maintenance regimen of patients with dental restorations. Part 1: tooth-borne restorations. J Prosthodont. 2016 Jan;25 Suppl 1:S2-15.
