The Correlation between Temporomandibular Disorders, Atypical Swallowing and Dyslalia
Abstract
Background: temporomandibular disorders are pathological conditions which involve temporomandibular joint. Their etiopathogenesis is multifactorial. Therefore it’s interesting to analyse their correlation with other structures of the oral cavity such as tongue. The context and purpose of the study: to investigate the eventual correlations between temporomandibular disorders and atypical swallowing and between temporomandibular disorders and dyslalia in adult subjects. It is also studied the association between atypical swallowing and dyslalia in temporomandibular disorders and in healthy patients. There are additional details about temporomandibular disorders diagnosis and treatment that you can obtain on our website in Trainings in TMJ Dysfunction.
Main findings: this study shows that the prevalence of atypical swallowing in the group with TMD is greater than in the group without TMD. These results suggest the presence of atypical swallowing could be used to detect an increased risk of temporomandibular disorders.
Results: the prevalence of temporomandibular disorders among subjects with or without atypical swallowing is respectively 67.7% and 46.7%, being statistically significant. The prevalence of temporomandibular disorders among subjects with or without dyslalia is respectively 62.5% and 48.9%, resulting not statistically significant. The prevalence of dyslalias in subjects with atypical swallowing is 28.6% in the group with temporomandibular disorders and 30.0% in the group without temporomandibular disorders. Therefore our study confirms the association between atypical swallowing and dyslalia, regardless of the fact that the treated patients were affected by temporomandibular disorders.
Conclusion: To our knowledge, this is the first study that investigates the existence of associations between temporomandibular disorders and tongue position in swallowing and phono-articulation in the adult population.
Brief summery: an observational case-control study was conducted. The total sample consisted of 100 adult subjects with temporomandibular disorders and 100 healthy adult subjects. All patients underwent a gnatology test, using Helkimo disfunction index, a phonemic test linked to evaluation of spontaneous speech for dyslalias and they eventually underwent a swallowing test. Comparison between groups with and without TMD was made using the chi-square test or Fisher’s exact test or test-parametric Mann-Whitney. Significance values p less than 0.05 were considered statistically significant.
Background
Temporomandibular disorders (TMD) include a variety of pathological conditions involving masticatory muscles, temporomandibular joint and associated structures [1]. Atypical swallowing is a “model” of swallowing characterized by contact between tongue tip and the upper or lower arch or interposed between them [2]. Dyslalia are disorders of articulation of the phonemes, caused by functional or organic alterations in the phonatory system [3].
As part of the multifactorial features of temporomandibular disorders [4-6], it could be clinically relevant to examine the relationship between TMD and tongue position in swallowing and phono-articulation. The existence of a possible correlation between temporomandibular disorders, atypical swallowing and dyslalias has been studied in pediatric patients and the results reported in literature are sometimes controversial [7-10]. Currently, there are no data concerning the adult population. The primary objective of this study is to examine whether in adult patients there is an association between temporomandibular disorders and atypical swallowing and between temporomandibular disorders and dyslalia. Studies have shown the existence of a relationship between atypical swallowing and dyslalia [2,3,11].
The secondary objective is to establish if in adult subjects this association is different between subjects with or without temporomandibular disorders.
Materials and Methods
The observational case-control study was conducted on 100 adult patients with temporo-mandibular disorders and 100 healthy subjects.
Patients with TMD were recruited sequentially, over a period of six months, in the Unit of Odontostomatology and Oral Prevention, San Paolo Hospital, University of Milan. They were matched by gender and age (+/- 2 years) with control subjects not affected by TMD, recruited from the staff of the Unit of Temporomandibular Disorders and Orofacial Pain, San Paolo Hospital, and patients of the Unit of Odontostomatology and Oral Prevention, San Paolo Hospital, being treated for simple conservative treatments or debridement. The informed consent of all patients has been obtained in accordance to the principles of Nuremberg Code, The Declaration of Helsinki and The Belmont Report. The project was executed so as not to cause any risk of harm and discomfort to patients. All the procedures are founded on scientific literature and are routinely used in clinical practice.
The subjects of both groups underwent an accurate gnathological examination to assess the effective presence of TMD. The evaluation was performed using a modifi ed version ñof Helkimo’s dysfunction index [12], which is based on the evaluation of the functional state of the masticatory system, taking into consideration:
A. Opening range: it was measured as the distance between upper and lower central incisor > 40 mm = score 0
30-39 mm = score 1
< 30 mm = score 5
B. Mandibula deviation during lowering:
< 2 mm = score 0
2-5 mm = score 1
> 5 mm= score 5
C. TMJ dysfunction: clicking, locking and luxation were evaluated:
no impairment = score 0
palpable clicking = score 1
evident clicking, locking and luxation = score 5
D. TMJ pain:
no pain = score 0
palpable pain = score 1
palpebral reflex = score 5
E. Muscle pain:
no pain = score 0
palpable pain = score 1
palpebral reflex = score 5
For each clinical sign, a score of 0, 1 or 5 points was assigned based on the presence and severity. The classification of clinical dysfunction, according to total score, includes:
No disfunction (D.0) = 0 points
Mild dysfunction (D.I) = from 1 to 4 points
Moderate dysfunction (D.II) = from 5 to 9 points
Severe dysfunction (D.III) = from10 to 25 points
All patients, in addition, underwent a swallowing examination to evaluate the presence of atypical swallowing. The swallowing examination consists of two phases of investigation: a phase of observation at rest and a phase of observation in the act of swallowing, breathing and articulation, in which the attention is placed on the position of the teeth, tongue, lips and oro-facial musculature.
The phase of extraoral observation at rest includes the evaluation of lines of symmetry of the face. Furthermore, it is necessary to detect characteristics typical of the so-called “facies adenoidea”: accentuated circles, small nose and narrow nostrils, incompetent and hypotonic lips [13]. In the phase of intraoral observation at rest we evaluated: dental formula, molar and canine relationships, overjet and overbite, upper and lower interincisive midlines, health of teeth and gums, shape of the palate and presence of hypertrophic tonsils. Particular attention should be paid to the posture of the tongue at rest: it can be on the palatal rugae (normal posture), against upper or lower incisors or interposed between the dental arches. In the extra and intra-oral observation, we evaluated the position of lips and tongue during swallowing. At first, we observed the patient in spontaneous swallowing of saliva, then in swallowing of water. A correct kinetics is characterized by tongue on the palatal rugae, lips in contact without effort and teeth in occlusion: this is the physiological swallowing [14].
In case of atypical swallowing we can observe: incompetence or hypertonic contact of lips with contraction of the orbicularis oris muscle, mentalis muscle and possible accentuation of the labiomental groove. In the intraoral functional examination, the position of the tongue is evaluated using a particular maneuver: while the patient swallows, the lower lip is lowered gently, but firmly to counteract the force exercised by the orbicularis oris muscle. The diffi culty in swallowing, with the attempt by the orbicular to close the dental gap and the incorrect posture of the tongue interposed between teeth are two important diagnostic elements. The tongue can make contact with upper or lower incisor or can be interposed between dental arches [15]. At the same time the focus is also on the position of dental arches and jaw. The jaw at rest presents physiologically dental arches not in contact with each other. During normal swallowing, it rises thanks to the contraction of jaw elevators bringing the teeth into contact, but without effort; palpating the temporal muscle and the masseter muscle, we can detect this contraction, while this doesn’t happen if the patient swallows without clenching his teeth. The patient can therefore swallow: physiologically (normal adult swallowing), lips and teeth in contact without effort and tongue on rugae; deviating with a simple tongue thrust: evident contraction of orofacial muscles, anterior tongue thrust, clenching dental arches; deviating with complex tongue thrust: evident contraction of the orbicular oris muscle and the mentalis muscle, no contraction of jaw elevators, anterior tongue thrust, open dental arches with tongue and/or lower lip interposed [16]. Finally, they underwent a phonemic examination to detect any phonoarticulatory disturbance, integrating this test with an evaluation of the spontaneous speech during the visit. The modified Schindler’s phonemic exam is used because it’s a valuable tool for the ease and speed of application. This exam consists in the repetition of simple words (mostly bisyllabic) containing different phonemes of the language, in initial and/or median position, and some consonant clusters. Using this test, it is possible to detect the presence of dislalia, the completeness of the phonetic inventory on repetition and the presence of some simplifications; on the basis of present phonemes it is possible to establish the performance range of patients [17]. The sample size was calculated to detect an odds ratio equal to or greater than 2.5 of atypical swallowing in patients with TMD compared to controls, assuming a fi rst-type error of 5% and 80% power. Comparison between subjects with or without temporomandibular disorders (TMD) was conducted using the Chi-square test or Fisher’s exact test, or the Mann-Whitney non-parametric test, when appropriate. Finally, the association between atypical swallowing and dyslalias in the total sample of subjects was tested separately in groups with or without TMD. Signifi cance values p less than 0.05 were considered statistically signifi cant (two-tailed test). The SPSS program (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Further information about TMJ pathologies treatment are accessible for you to learn on our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
Results and Discussion
The prevalence of atypical swallowing in the group with TMD is 21%, compared to 10% of the group without TMD. This difference is statistically significant (p=0.032; chi-square test), with odds ratio of 2.39 and relative 95% confi dence interval 1.01 - 5.83. However, the prevalence of dyslalia in the group with TMD is 10%, while in the group without TMD it is 6%. This difference is not statistically significant (p = 0.435, Fisher’s exact test). A stratifi ed analysis by gender did not show any significant difference in the prevalence of atypical swallowing between males and females in subjects with TMD (prevalence: females 21.5%, males 20%, p> 0.05) or in those without TMD (prevalence: females 10.8%, males 8.6%, p> 0.05). Similar results have been obtained for dyslalia.
Specifically, the analysis showed no significant difference in the prevalence of dyslalia between males and females in subjects with TMD (prevalence: females 12.3%, males 5.7%, p> 0.05) or in those without TMD (prevalence: females 6.2%, males 5.7%, p> 0.05), as illustrated in table 1. The prevalence of TMD among subjects with or without atypical swallowing is equal to 67.7% and 46.7%, respectively, being statistically significant (p<0.05), as shown in figure 1. The results in literature, related to research conducted in pediatric age, are controversial for atypical swallowing [7-10]. The prevalence of TMD among subjects with or without dyslalia is 62.5% and 48.9%, respectively, resulting not statistically significant (p=0.435), as shown in figure 2. Finally, the association between atypical swallowing and dyslalia, in the overall sample of subjects and separately in groups with or without TMD, was tested. The association between the presence of dyslalia and atypical swallowing was found statistically signifi cant in patients with TMD (p <0.001; odds ratio = 7.5; 95% CI = 1.9 - 29.9) and in controls (p = 0.013; odds ratio = 12.4; 95% CI = 2.1 - 73.4), as illustrated in table 2. This association is widely reported in literature [2,3-11].
The prevalence of dyslalia in subjects with atypical swallowing is comparable in the two groups with or without TMD: respectively, 28.6% and 30.0% (p=0.999), as shown in figure 3.
Table 1: Association of TMD with atypical swallowing and dyslalia.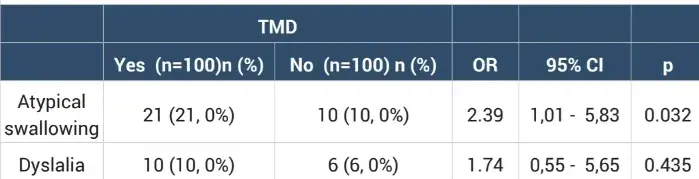
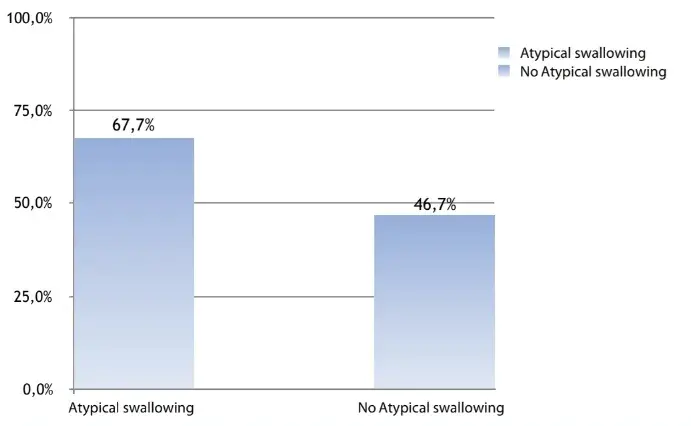 Figure 1: Prevalence of TMD in subjects with or without atypical swallowing.
Figure 1: Prevalence of TMD in subjects with or without atypical swallowing.
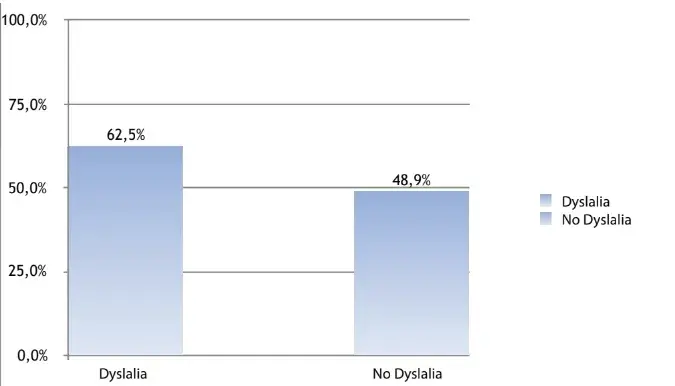 Figure 2: Prevalence of TMD in subjects with or without dyslalia.
Figure 2: Prevalence of TMD in subjects with or without dyslalia.
Table 2: Association between atypical swallowing and dyslalia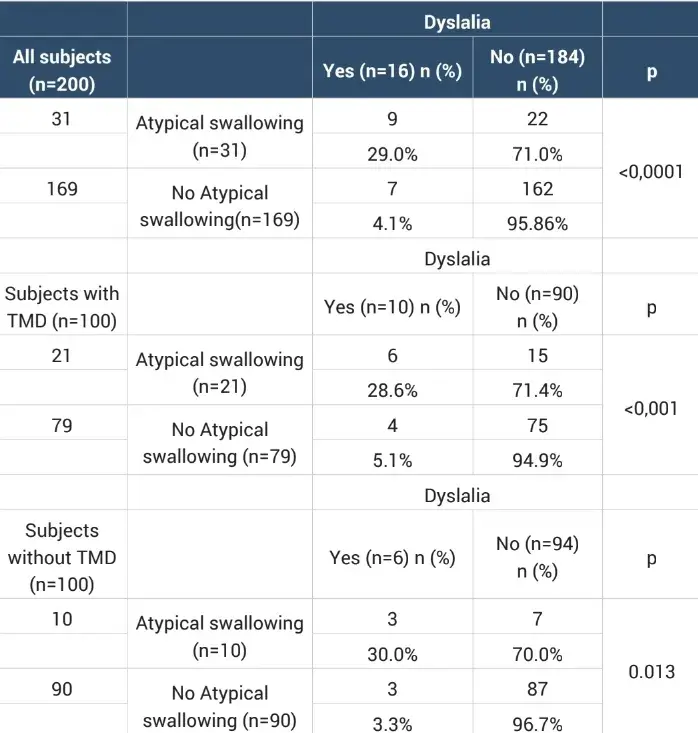
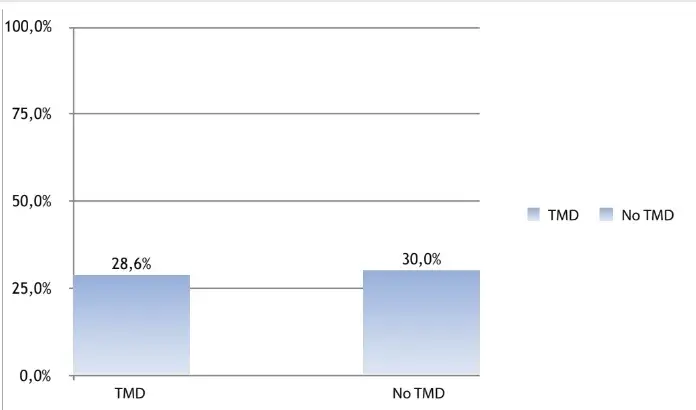 Figure 3: Prevalence of dyslalia in subjects with atypical swallowing, ingroups with or without TMD.
Figure 3: Prevalence of dyslalia in subjects with atypical swallowing, ingroups with or without TMD.
Conclusion
In conclusion, the results of this observational case-control study, the fi rst to our knowledge to be conducted on the adult population. It suggests the existence of a statistically significant association between TMD and atypical swallowing but not between TMD and dyslalia. No association was found between TMD and dyslalia. Our study has confirmed secondarily the association between atypical swallowing and dyslalia, regardless of temporomandibular disorders. Given the observational nature of the study, it is not possible to draw any conclusion on the possible etiologic relationship between TMD and atypical swallowing. Longitudinal studies with adequate statistical boots are needed to clarify the possible inter-relationships between TMD and atypical swallowing.
If you enjoyed reading this article and would like to explore temporomandibular joint pathologies further, we encourage you to enroll our course "Evidence-based treatment of temporomandibular disorders".
List of authors:
Alessandro Marchesi, Daniele D’Apote, Anna D’Apote, Riccardo Ciancaglini, Laura Strohmenger
References
Costen JB (1934) A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol 43: 1-15.
Schindler O, Ruoppolo G, Schindler A (2010) Fisiologia della deglutizione. In Deglutologia, 2nd edition. Edited by Omega Edizioni, Torino 87-99.
Perrotta E, Rustici P (2006) Introduzione. In Correggere i difetti di pronuncia, 1st edition. Edited by Erickson Edizioni, Trento 7-13.
Oral K, Bal Kucuk B, Ebeoglu B, Dinçer S (2009) Etiology of temporomandibular disorder pain 21: 89-94.
Greene CS, Mogini F (2005) Temporomandibular disorders (TMD). Prog Orthod 6: 224-231.
Scrivani SJ, Keith DA, Kaban LB (2008) Temporomandibular disorders. N Engl J Med 359: 2693-2705.
Castelo PM, Gavião MB, Pereira LJ, Bonjardim LR, Gavião MBD (2005) Relationship between oral parafunctional/nutritive sucking habits and temporomandibular joint dysfunction in primary dentition. Int J Paediatr Dent 15: 29-36.
Williamson EH, Hall JT, Zwemer JD (1990) Swallowing patterns in human subjects with and without temporomandibular dysfunction. American Journal of Orthodontics and Dentofacial Orthopedics 98: 507-511.
Vierucci F, Mongelli C, Doldo T (2010) Relationship between parafunctional habits, malocclusions and temporomandibular disorders in primary and mixed dentition (Correlazione tra parafunzioni orali, malocclusioni e disordini temporomandibolari in pazienti in dentizione primaria e mista). Mondo Ortodontico 35: 263-268.
Goldstein LB, Last FC, Salerno VM (1997) Prevalence of hyperactive digastric muscles during swallowing as measured by electromyography in patients with myofascial pain dysfunction syndrome. Functional Orthodontist 14: 18-22,24.
De Filippis Cippone A (1998) Deglutizione atipica e terapia miofunzionale. In Nuovo manuale di logopedia. Edited by Erickson Edizioni, Trento 71-100.
Sapna R, Salil P, Sunil G, Mansha B (2017) Analysis of Helkimo index for temporomandibular disorder diagnosis in the dental students of Faridabad city: a cross-sectional study. J Indian Prosthodont Soc 17: 48-52.
Farronato G, Maspero C, Chimenti C, Cordasco G, Festa F et al. (2013) Indagini strumentali. In Ortogonatodonzia, Volume 1, 1st edition. Edited by Edi.Ermes, Milano 300-305.
Lanteri C, Beretta M Deglutizione, dislalie e malocclusioni. Società Italiana di Ortodonzia (SIDO).
Maspero C, Prevedello C, Giannini L, Galbiati G, Farronato G (2014) Atypical swallowing: a review. Minerva Stomatol 63: 217-227.
Ierardo G, Manzon L, Ottolenghi L, Polimeri A (1999) Aspetti clinici e terapeutici della deglutizione atipica. Dental Cadmos 17: 55-83.
Gilardone M, Casetta M, Luciani A (2008) Il bambino con disturbo di linguaggio. Valutazione etrattamento logopedico. Edited by Cortina, Torino.
