Salivary stone disease. Clinic, diagnosis, treatment
Machine translation
Original article is written in RU language (link to read it) , IT language (link to read it) .
Salivary stone disease is a disease that affects both men and women equally. Moreover, the age range for salivary stone disease is very wide: cases occur in childhood, middle age and old age.
Find more useful information on surgical dentistry in the section of our website. Maxillofacial surgery training .
The incidence of this pathology is about 20.5%-60% of cases with a predominant lesion of the submandibular salivary gland. In this article we will look at the clinical picture, diagnosis and treatment of salivary stone disease.

The submandibular salivary gland often suffers from salivary stone disease due to:
- saliva flow against gravity;
- long and winding channel;
- contains two types of terminal sections: protein (predominant) and mucous.
In general, salivary stone disease is manifested by the appearance of stones of various sizes and shapes in the gland itself, but more often in its duct. The process of stone formation is long and may be asymptomatic.
Etiology of salivary stone disease
The etiology of salivary stone disease is not fully known. The fact is that in some patients, factors that play an important role in the occurrence of salivary stone disease do not lead to the development of pathology at all. And the opposite: patients who have no suspected etiological factors come with a huge stone in the salivary gland duct. Among the factors that may play a role in the etiology of salivary stone disease are the following:
- increased saliva viscosity;
- change in acid-base balance, alkalization;
- narrowing of the duct;
- inflammation of the duct;
- entry of foreign bodies into the duct;
- metabolic disorders in the body when calcium levels are higher than normal;
- genetic predisposition;
- improperly developed gland and its duct during anthogenesis;
- hypovitaminosis/vitaminosis group A;
- chronic diseases of the salivary gland.
Pathogenesis of salivary stone disease
The pathogenesis of salivary stone disease is a rather difficult process to understand and study. The difficulty in studying salivary stone disease lies in determining the triggering moment and the cause of the occurrence of salivary stone, because patients arrive at later clinical stages.
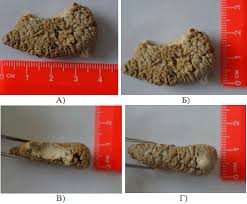
But if we talk about the chemical composition of the salivary gland stone, then these stones are complex in their structure, consisting of both organic and mineral substances. Moreover, the mineral component is predominant, accounting for 60-70%. Representatives of the mineral component in salivary gland stones are phosphates, calcium, and calcium-based salts. The organic component is bacteria, elements lining the ducts and the organic composition of saliva. Salivary gland concretions grow gradually, which reveals their layered structure. There are differences in the composition of salivary gland stones. Thus, the parotid salivary gland is characterized by a predominance of the organic component over the mineral one, and in the submandibular salivary gland, the opposite is true.
There are several theories about the pathogenesis of salivary stone disease. Some authors believe that the pathogenesis is based on a violation or instability of the state of the components that participate in the formation of the stone, which leads to their coagulation and crystallization. The point is that a core is formed from an organic component. Then the process of mineralization begins around this core, that is, the mantle is formed. These processes occur due to adsorption; the stone initially has the consistency of jelly. Subsequently, due to calcium, phosphate ions and their salts, the stone becomes dense.
There is another opinion. The basis of stone formation is the core, which is always an organic component. And most often, the trigger point in the occurrence of minerals and their adsorption is inflammatory diseases in the salivary gland, a change in the rate of salivation, saliva viscosity or pH.
An interesting fact: in the saliva of mammals (animals) and humans, microconcretions were found in a healthy salivary gland that did not in any way affect the functioning of the salivary gland. Consequently, the occurrence of a stone in the salivary gland will not always be a pathological process.
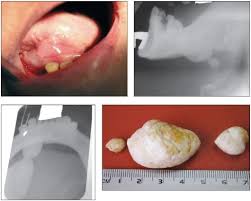
The process of stone formation is long. And there is no direct relationship between the size of the stone and the duration of its formation. However, stones can be either smooth or rough. There are grooves or channels on the surface of the stones. They are very variable in form. Thus, there are stones of oval, round, ovoid, elongated, and oblong shapes. There is a difference in the density of stones depending on their location. So the stones that are located in the gland itself will have a denser consistency. Most often, such stones are round in shape.
Clinical picture of salivary stone disease
The clinical picture of salivary stone disease consists of three main stages:
- The initial stage of salivary stone disease.
- Clinically pronounced stage of salivary stone disease.
- Late stage of salivary stone disease.
The initial stage of salivary stone disease is characterized by the complete absence of any acute clinical signs. Here changes occur at the histological level:
- dilation and congestion of blood vessels;
- swelling and loosening of connective tissue;
- formation of lymphocytic infiltrates;
- preservation of acini;
- expansion of intralobular, interlobular ducts;
- increase and compaction of collagen fibers.

One of the very first and main clinical signs of the initial stage of salivary stone disease is a change in the rate of salivation, especially when eating food and at the sight of food. Patients experience so-called “salivary colic.” Salivary colic with salivary stone disease is a common occurrence. Characterized by enlargement of the salivary gland; patients say: “It’s as if something is bursting,” pain occurs. The pain interval can be short: from a few seconds, but with the progression of the disease it increases to several hours.
If you palpate the salivary gland, the doctor notes its softness and painlessness, the secretion is released normally. When palpating the duct of the submandibular salivary gland, a dense calculus can be detected. When examining the oral cavity, no changes in the mucous membrane are noted.


The clinically expressed stage of salivary stone disease is a progression of the initial stage. The name of the stage speaks for itself: at this stage of development there is pronounced inflammation of the salivary gland. Symptoms are similar to acute sialadenitis:
- Acute onset: increased body temperature to 38.5 degrees, general malaise, weakness, headache.
- Facial asymmetry due to swelling of soft tissues in the area of the salivary gland.
- Edema.
- Difficulty eating.
- Painful palpation of the salivary gland.
- When examined from the oral cavity, hyperemia of the mucous membrane on the corresponding side is noted.
- Upon palpation, a stone is identified.
Without treatment, with each exacerbation the disease reaches a late clinical stage. This may be preceded by a purulent-necrotic form of salivary stone disease.
The late stage of salivary stone disease is characterized by complete atrophy of the salivary gland acini with replacement of the parenchyma by connective tissue.
The clinical picture of salivary stone disease at a late stage is characterized by the following symptoms:
- constant aching pain in the gland area;
- rare “salivary colic”;
- swelling of soft tissues;
- eating is difficult or impossible;
- general condition is disturbed;
- asymmetry of the face due to edema, but only within the gland;
- on palpation – painlessness;
- when massaging the gland - mucopurulent discharge from the duct.
- the mouth of the duct is widened.
Diagnosis of salivary stone disease
Diagnosis of salivary stone disease consists primarily of a careful collection of complaints, life history and illness. This is followed by an examination, both external and intraoral. For qualitative diagnosis of stones in the ducts of the salivary glands, the technique of bimanual palpation is used. To do this, the fingers of one hand are placed on the mucous membrane in the projection of the gland and its duct, the fingers of the other hand are placed on the side of the skin.

After bimanual palpation, it is recommended to massage the gland, which will determine the consistency of the secretion and the rate of its release. Probing the duct in case of salivary stone disease is not recommended at the time of exacerbation, as this can lead to perforation of the duct wall. And so probing with the help of special probes is allowed. Using probes, you can determine the fistula tracts if there was a perforation of the stone.
For a high-quality diagnosis of salivary stone disease, you need to understand two points: when the stone is localized in the salivary gland, there are no clinical symptoms. Such stones are discovered purely by chance. But when a stone moves from a gland into a duct or along a duct, the clinical picture is very variable.
The main methods for diagnosing salivary stone disease are radiation methods. Due to the mineral component in salivary stones, these stones are X-ray positive.
Radiation methods that can be used:
- Survey radiography. Survey radiography can be of the floor of the mouth, which is recommended for examining the anterior and middle sections of the excretory duct of the submandibular salivary gland, or it can be in a lateral projection to determine a calculus either in the submandibular salivary gland itself or in its initial section.
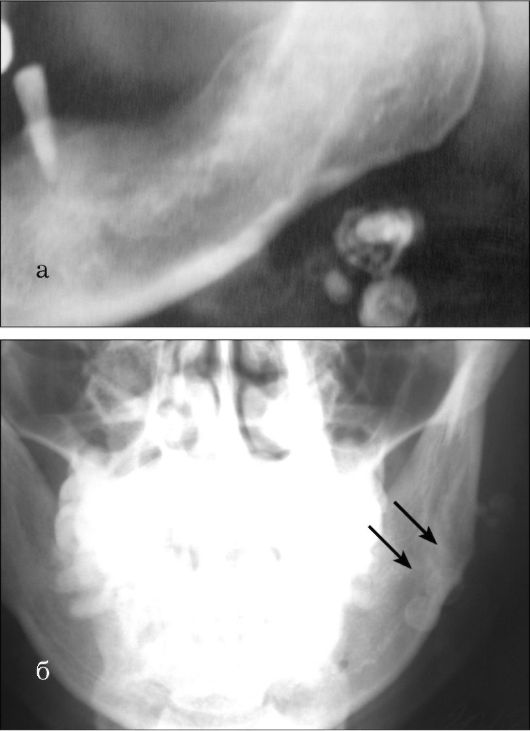
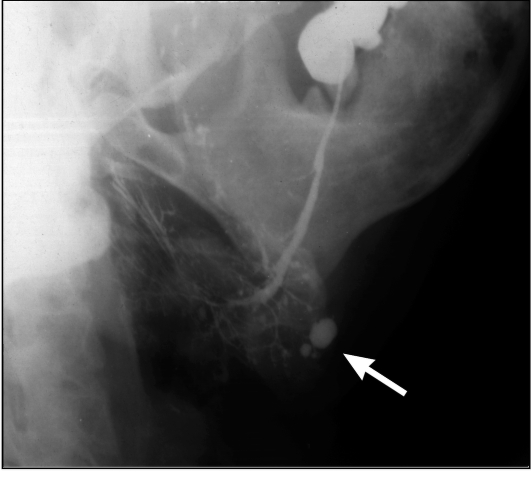
- Contrast sialography, which has not lost its importance both for the diagnosis of salivary stone disease and for other diseases of the salivary glands. Verografin, urografin, and cardiotrast are used as contrast agents. All substances are water-based and do not have a pathological effect on glandular tissue.
- Digital subtraction sialography. This diagnostic method is good because there is no overlap of images of the salivary glands and the skull. This occurs due to the fact that before the contrast agent is introduced, the study area is recorded in the computer memory, which is then subtracted from the image with the contrast agent injected.
- Cone beam computed tomography;
- Ultrasound examination of the salivary gland can be carried out both from the skin and from the oral mucosa. Due to the different ability of tissues to display sound, it is possible to determine X-ray negative stones, their location and size.
- In order to determine structural and functional changes in the salivary glands, radionuclide studies and magnetic resonance computed tomography can be performed.
- Fiberendoscopy of the salivary glands is based on the use of ultra-thin fiber optics, which are inserted into the main duct of the salivary gland. It is the newest method in the study of the salivary glands.
Treatment of salivary stones
The basis of any treatment is the elimination of etiological factors in the occurrence of the disease. However, the etiology and pathogenesis of salivary stone disease are not fully understood. Therefore, the treatment of salivary stone disease consists of removing the stones. The goal of treatment is not only to remove stones, but also to restore the functioning of the gland.
The submandibular salivary glands have an excellent adaptive response. Therefore, after removal, there is often either partial or complete restoration of both structural and functional integrity.
Treatment methods for salivary stone disease include:
- conservative (non-invasive);
- low impact;
- invasive/surgical.
Conservative treatment methods are only auxiliary. With the help of medications, salivation is increased. In addition to drugs for a salivary effect, massage of the salivary gland and a salivary diet are prescribed.
Minimally invasive methods are based on the use of some physical factor to crush the stone, which facilitates exit from the mouth of the excretory duct. That is, salivary stone is removed in a closed way. Minimally invasive methods that can be used:
- Extracorporeal shock wave lithotripsy is based on the use of ultrasonic lithotrips. Recommended for stones no more than 1 cm in diameter.

- Intracorporeal shock wave lithotripsy: special laser or electro-hydraulic lithotrips are used. It is carried out when the stone is localized in the proximal part of the salivary gland.
- Endoscopic stone removal.
Surgical treatment of salivary stone disease is the main method of treatment when the stone is localized in the duct or in the submandibular salivary gland itself. The choice of a specific surgical technique depends on the location of the calculus, its shape and size, and the condition of the submandibular salivary gland. The condition of the submandibular salivary gland plays an important role, since there are operations aimed at preserving the submandibular salivary gland, and there are, on the contrary, organ-non-preserving operations.
Organ-conserving surgery is performed through intraoral access.

The purpose of the operation is to free the duct from the stone and restore the normal flow of saliva. The operation is indicated only if the stone is localized either in the middle or in the distal part of the excretory duct of the submandibular salivary gland.
Organ-non-sparing surgery involves extirpation (complete removal) of the submandibular salivary gland. After removal of the gland, some authors recommend additional dissection throughout the entire part of the extraglandular section of the excretory duct, followed by suturing the edges of the wound with the mucous membrane of the sublingual region. These actions are aimed at preventing the development of sialodochitis in the remaining part of the excretory duct.
Removal of the submandibular salivary gland can be complicated by processes such as:
- traumatic neuritis of the lingual nerve;
- traumatic neuritis of the hypoglossal nerve;
- traumatic neuritis of the facial nerve;
- progression of chronic inflammation.
Removal of the submandibular salivary gland is a radical operation. After all, it is believed that the remaining salivary glands can fully compensate for the work of the removed submandibular gland. However, if we evaluate the relationship and influence of the large salivary glands on both internal and external secretion, on the relationship with the body, then radicalism will not always be justified. After all, it was noticed that with the complete removal of one of the submandibular salivary glands, no signs of hypertrophy were noticed on the other side. This means that the normal compensatory response is disrupted during such operations.
Therefore, it is necessary to strictly determine the indications for extirpation of the submandibular salivary gland, and pay more attention to minimally invasive treatment methods.
Find a lot of useful and relevant information on various areas of dentistry on our website .
