Pigmentation of the gums. Treatment, errors and complications
Machine translation
Original article is written in RU language (link to read it) .
In recent years, there has been a shift in dentistry in which aesthetics has become a higher priority than in the past. Patients' cosmetic expectations are constantly increasing, so gingival pigmentation, especially in areas that are visible when smiling and speaking, has become an important component of aesthetics and an attractive smile.
Detailed protocols for the surgical treatment of periodontal diseases from world experts in the online course Surgical Periodontology .
Although gum pigmentation occurs in all races, it is more commonly seen in dark-skinned populations. The gums are the most pigmented of all oral tissues. Physiological melanin pigmentation is relatively common in dark-skinned individuals, and generally the degree of gingival melanin pigmentation correlates well with the degree of skin melanin pigmentation. The most common etiology of pigments that alter the normal color of the gums is the deposition of melanin by melanocytes, which in turn depends on the activity of the enzyme tyrosinase.
Gingival depigmentation is a periodontal plastic surgery procedure to remove pigmented gums. The gum depigmentation procedure can be performed using a laser; however, as described in this case report, laser burns may be associated with this procedure and, if this occurs, they must be subsequently treated.
Clinical case
In this clinical case, the patient had an extensive elliptical ulceration on the right side of the upper jaw in the premolar area. The underlying alveolar bone was exposed and the surrounding gingival margins were inflamed. After debridement of the area and removal of sequestered bone tissue, bone graft and subepithelial connective tissue graft were placed using microsurgical techniques to correct the defect. This case report aims to raise awareness of the potential complications of gingival depigmentation surgery and to present a possible approach for treating such complications.
Due to the oral melanin pigmentation pandemic and today's high cosmetic demands, the topic of gum pigmentation has gained great importance. Gum depigmentation is a periodontal plastic surgery procedure in which pigmented gums are removed. To date, several different techniques have been used for gingival depigmentation, including mechanical, surgical, electrosurgical, and cryosurgery techniques; cauterization using chemical agents; gum grafts and lasers. Scalpel surgery for depigmentation is time-tested and remains the gold standard.
Laser to remove gum pigmentation
Lasers that are commonly used for gum depigmentation are carbon dioxide (CO2) (10,600 nm) and neodymium-doped yttrium aluminum garnet (Nd:YAG) (1,064 nm), although erbium-doped yttrium aluminum garnet (Er:YAG) (2,940 nm) has recently attracted more and more attention. Laser therapy removes melanin pigment by ablation (from the word ablation) epithelial tissue. This requires melanocytes to be within the laser's penetration range and contain melanin to absorb and convert light energy into heat through photothermolysis. The intensity and time interval of repetitions depend on the treatment methods used. There are numerous treatment options for depigmentation, but laser is emerging as the most effective, acceptable and reliable method. Laser use is associated with less pain compared to other treatment methods.
In the present clinical case, a laser burn occurred as a result of improper use during the depigmentation procedure. A review of reported laser-related incidents in the literature showed that most of them involved ocular injuries or skin injuries. Few papers in the literature have reported laser burns to mucous membranes, and none have reported laser burns associated with gingival depigmentation procedures. According to the author, this is the first report of a clinical case of laser gum burn as a result of laser depigmentation and its elimination.
Clinical case
A 28-year-old female patient was offered cosmetic correction of ulcerated gums with exposed bone on the right upper jaw in the premolar area as a result of laser depigmentation of the gums, which was performed 2 months ago in a private clinic. The patient reported that the procedure left a bare area that would not heal and that there was no improvement in the following weeks. As a result, she decided to seek an opinion on the matter from the Department of Periodontology Clinic, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia.
Plastic surgery to repair gum burns
On examination, a large elliptical ulceration was observed extending from the mesial edge of tooth No. 3 to the mesial edge of tooth No. 5 (Figure 1). The underlying alveolar bone was exposed and the surrounding gingival margins were inflamed. Corrective periodontal plastic surgery was performed, including removal of bone sequestration, augmentation of the underlying bone layer and reconstruction of the overlying soft tissue. In addition, due to the thin wound and the difficulty of subsequent repair, periodontal microsurgery techniques were used.

Figure 1: Preliminary intraoral photograph of the maxillary premolar region on the right, which shows exposed alveolar bone with inflamed gingival margins at the wound.
After local anesthesia, an incision was made medial to the gingival sulcus, which was limited to the buccal surface of tooth No. 4 using a microsurgical blade (SM Blade, Hartzell, denmat.com) (Figure 2). The edges of the wound were carefully debrided using the same blade to create a fresh wound. A microsurgical periosteal elevator (Micro Elevator, Hartzell) was used to gently elevate the coronal gingival margins and to create a pocket using blunt dissection (Figure 3 and Figure 4). The bony sequestration was removed and the underlying alveolar bone was recontoured using a piezoelectric knife (Piezotome, Satelec Acteon, dental-bone-surgery.com) (Figure 5).

Photo 2. The incision is made using a microsurgical blade.

Photo 3. Displacement of the marginal edge is performed using a microsurgical periosteal elevator.
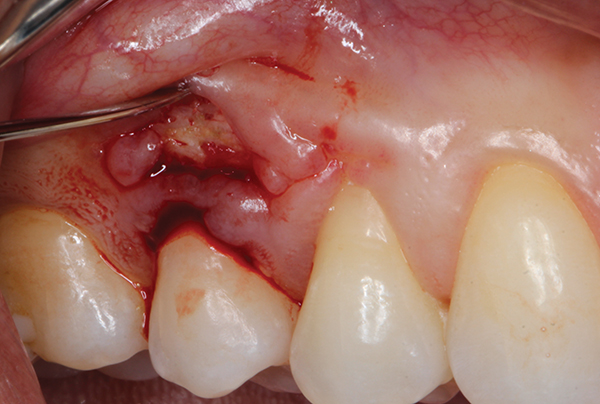
Photo 4
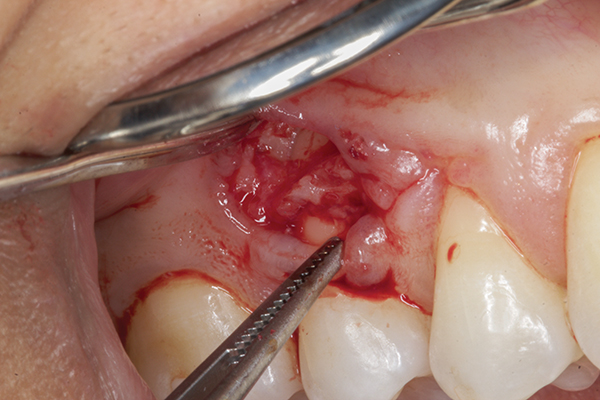
Photo 5. Bone recontouring and stimulation of bone bleeding
After inducing bleeding, 0.5 cm3 demineralized freeze-dried bone (Ace Surgical Supply, acesurgical.com) was grafted to cover the exposed bone and roots (Figure 6). A subepithelial connective tissue graft was taken from the ipsilateral palate (Figure 7) and placed under the gingival pocket and over the bone graft. The gingival graft was secured and the incision was sutured with chrome catgut using single interrupted sutures (Figure 8). After suturing the donor site (palate), the recipient site was protected with a periodontal dressing (COE-Pak™, GC America, gcamerica.com).

Photo 6: Demineralized freeze-dried bone added over exposed bone and roots.
 Photo 7. The mucous membrane of the palate after removal of the connective tissue graft.
Photo 7. The mucous membrane of the palate after removal of the connective tissue graft.

Photo 8. The final seams are placed without tension. The subepithelial connective tissue graft was sutured to the papillae, and the buccal flap was sutured over the graft using chrome catgut.
The patient was sent home with prescriptions for an antibiotic (500 mg amoxicillin, three times daily for 7 days) to minimize the risk of infection and a nonsteroidal anti-inflammatory drug (400 mg ibuprofen). She was instructed to rinse with chlorhexidine twice daily for 2 weeks. The patient was prescribed once a week for the first 2 weeks (photo 9 and photo 10), and then once a month for 3 months. After a 3-month postoperative follow-up, recovery was adequate at both the recipient and donor sites (Figure 11 and Figure 12), and the patient was satisfied with the outcome.
 Photo 9. Postoperative recipient site after 2 weeks.
Photo 9. Postoperative recipient site after 2 weeks.  Photo 10. Post-operative donor site after 2 weeks.
Photo 10. Post-operative donor site after 2 weeks.

Photo 11. Postoperative recipient site after 3 months.
 Photo 12. Postoperative donor site after 3 months.
Photo 12. Postoperative donor site after 3 months.
Laser
The laser is a simple device that has revolutionized clinical practice. However, the diversity of laser technologies in terms of different wavelengths, energy modes and settings has led to the emergence of a variety of clinical protocols in general dentistry and periodontics in particular. Given this variety, clinicians should only implement laser treatments after gaining a thorough understanding of the technology and how to use it correctly to maximize benefits and minimize the risk of injury.
Laser depigmentation
The prognosis for laser depigmentation is usually favorable. As the use of lasers becomes more common and their applications become more diverse, regulation of laser use and safety monitoring are important considerations. Follow-up after such treatment is important as all laser procedures have inherent risks, including burns, and the treatment provider must provide the necessary care.
Because not all lasers work the same, clinicians must be trained on each one they work with. The practitioner must consider the type of laser used and its indications, as well as understand the biophysics of the laser, the appropriate settings for a particular procedure, and what to do if complications occur. In this case report, the patient was referred to the author's clinic and he was unsure of the type of laser used in the patient's previous treatment.
Giannelli et al studied the clinical effectiveness of two different lasers for gingival depigmentation, the diode laser and the Er:YAG laser. They reported that the diode laser gave better results. They also concluded that the Er:YAG laser should be used with caution as it often results in incomplete ablation of the gingival epithelium with deeper epithelial ridges, requiring repeat procedures and therefore increasing the risk of damage to the lamina propria. It causes blood vessels to dilate, which results in delayed wound healing. These and other data confirm that the diode laser has the benefit of safe and successful use in cases of gingival hyperpigmentation with minimal intra- and post-operative trauma.
The patient in this case suffered complications caused by improper use of the laser during gum depigmentation. Presumably, her injuries were unintentional and her dentist did not do anything wrong on purpose.
Fortunately, oral mucosa is highly treatable compared to skin fibroblasts. Histologically, fibroblasts of the oral mucosa are phenotypically different from skin fibroblasts and are more closely related to embryonic fibroblasts. Such differences contribute to the rapid healing of the oral mucosa. Another reason for rapid healing is that the oral mucosa is constantly covered with saliva, which contains many growth factors and biologically active peptides and proteins. These substances promote tissue growth and differentiation, thereby promoting wound healing. It is noteworthy that if the injury is deep (reaches the bone, as in this case), treatment of the necrotic edges of the wound will be indicated, and then tissue transplantation into this area.
Another important element associated with impaired wound healing is hypoxia. Wounds should have a minimum oxygen pressure of 30 mmHg. Art. for normal cell division and a minimum of 15 mm Hg. Art. for fibroblast proliferation. Adequate oxygenation is critical for cell proliferation, angiogenesis, collagen synthesis, and re-epithelialization. Therefore, in this case, careful debridement of necrotic bone to expose new healthy bone with neovascularization was mandatory to obtain minimal oxygen pressure and subsequent normal wound healing.
In addition to the presence of dead bone, another possible contribution to the chronicity and delay of healing in this case was that the wound was stretching the basement membrane through the connective tissue and creating bone necrosis. Since the main elements of the basement membrane include type IV collagen and adhesion molecules (laminins and fibronectin), which are important for fibroblast growth factor and vascular endothelial growth factor binding, they influence angiogenesis and accelerate the healing process.
To avoid complications, if the clinician is in doubt, it may be advisable to use a longer wavelength with low fluence and high pulse duration. This is based on the principle of conservativeness, according to which more intensive treatment can be applied later. Because treatment that has already begun and has become excessively intensive cannot be cancelled. Additionally, while all laser technicians should take every precaution to prevent burns from occurring, they should also be aware of the fundamental techniques by which burns can be treated should they occur.
The main obstacle in performing the operation in this clinical case was the correct treatment of necrotic bone, since within a small wound the author had to reach (get to) living bone in order to ensure a good blood supply to the subsequently introduced overlying graft. Clinically, necrotic bone appears as a white or yellowish, painless, exposed area. However, in cases with a large area, it may have symptoms of secondary infection, leading to inflammation, the formation of pus, an unpleasant odor and pain. Attempts to cover necrotic bone with local flaps or soft tissue grafts often fail, resulting in subsequent bone exposure and loss of overlying soft tissue. In this case, the operation was performed with magnifying instruments, and the surgeon attempted to remove necrotic bone until vital bone was exposed before suturing. However, it was extremely difficult.
Gum depigmentation using laser
Potential complications may arise from laser depigmentation of the gums. Practitioners using lasers should exercise extreme caution and understand how to prevent the type of injury described here. However, the risk of laser burn can never be completely eliminated. All laser practitioners should be familiar with the appropriate techniques to treat burns should they occur.
Even more relevant information in the online course Surgical periodontology: preparation for prosthetics .
