Natural course of temporomandibular disorders with low pain-related impairment: a 2-to-3-year follow-up study
SUMMARY
To describe the natural course of temporomandibular disorders (TMD) in patients with low levels of pain-related impairment, independently by the physical diagnoses they received. Amongst all patients who attended the TMD Clinic, University of Padova, Italy, during the year 2009, those who: (i) had Research Diagnostic Criteria for TMD (RDC/TMD) axis II Graded Chronic Pain Scale (GCPS) grade 0 or 1 scores, (ii) received counselling on their signs and symptoms at the time of their first visit and suggestions on how to self-manage their symptoms, (iii) did not attend the Clinic since the time of their last visit and (iv) were visited by the same resident, were recalled for a follow-up assessment during the period from September to December 2011. Sixty-nine patients (79% females; mean age 47.4 +- 11.3 years; range 26–77) of 86 who were potentially eligible accepted to enter the study.
The time span since the first visit ranged from 23 to 36 months. At the follow-up assessment, the percentage of patients with muscle disorders decreased from 68.1% to 23.1%; disc displacement with reduction remained unchanged (52.1%), whilst the 5.7% of patients who had disc displacement without reduction with limited opening then showed absence of limitation; diagnoses related to other joint disorders decreased from 30.4% to 14.4% for arthralgia and from 27.5% to 24.6% for osteoarthritis/osteoarthrosis. In a sample of patients TMD with low pain-related impairment followed up with a single recall assessment at 2-to-3 years, the natural course of disease was generally favourable.
There are additional details about temporomandibular disorders you can learn in our Online congress on evidence-based temporomandibular disorders and bruxism treatment.
INTRODUCTION
Temporomandibular disorders (TMD) are heterogeneous conditions affecting the temporomandibular joints (TMJ), the jaw muscles, or both (1). Such disorders have a complex pathophysiology with a multitude of risk factors interacting at the individual level.
Importantly, whilst some patients develop chronic pain and are very demanding from a therapeutic viewpoint, the prognosis is favourable in the majority of subjects presenting TMD signs and symptoms, thus supporting the need for adopting reversible and conservative treatments (2, 3). Fluctuation and self-remission of symptoms are a major source of bias for studies on the effectiveness of TMD treatments as well as one of the reasons why high success rates have been described for several treatment approaches (4). The description of the natural course of disease is fundamental to get deeper into the epidemiology of such disorders and to appraise critically all the studies on treatment effectiveness. Several investigations have been performed so far in the attempt to improve knowledge on the natural course of disease or the positive effects of conservative treatments over long follow-up periods (5–8). A major shortcoming of the available investigation is that patients’ recruitment was based on the physical diagnosis, viz., a clinical assessment or even the so-called axis I of the Research Diagnostic Criteria for TMD (RDC/TMD) (9).
Such an approach did not take into proper account for the importance of a thorough psychosocial assessment, which is likely to have much importance in terms of disease’s course and treatment outcomes.
The Graded Chronic Pain Scale (GCPS) included amongst the evaluation instruments of the RDC/TMD axis II may be assumed as the standard of reference for assessing pain-related impairment in patients with TMD, because it allows identifying five categories of patients with TMD based on their pain-related impairment (10). Multicentre studies have shown that subjects with the most severe GCPS ratings (i.e. grade III or IV) are only 15–20% of the TMD patient populations (11) and that impairment levels are not associated with axis I diagnoses (12). Also, patients with severe impairment are the worst treatment responders (13), whilst those with low impairment benefit a lot from simple cognitive-behavioural therapy regimens (14).
With these premises, the present investigation described the natural course of TMD signs and symptoms in patients with low levels of pain-related impairment, independently by the physical diagnoses they received, with the aim to gain a better insight into the epidemiological features of TMD. To ease comparison with future studies, this manuscript was reported according to the STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) guidelines for reporting observational trials, which were elaborated as an useful strategy to improve reporting of observational studies (Table 1) (15).
Table 1. Key study features. Summary checklist according to the STROBE guidelines for REPORTING observational studies
MATERIAL AND METHODS
The study sample was composed of patients with no pain-related impairment or low pain-related impairment (low disability, low intensity) attending the TMD Clinic, Department of Maxillofacial Surgery, University of Padova, Italy to seek for TMD advice and/or treatment. As part of a project for a MSc thesis, all patients who attended the clinic during the year 2009 and were included in the clinic database were screened for inclusion in the study. To be included in the investigation, patients had to: (i) Present RDC/TMD axis II GCPS grade 0 or 1 scores, (ii)
Receive counselling/advice on their signs and symptoms at the time of their first visit and receive suggestions on how to self-manage their symptoms, (iii) Not to attend the clinic since the time of their last visit and (iv) Being visited by the same resident (G.G.) who was then taking part to the postgraduate MSc residency in TMD during the years 2010–2011. The two leading investigators of the project (D.M, L.G.N.) acted as clinical supervisors in both periods.
The routine procedure in use at the TMD Clinic provides that patients received an assessment performed in accordance with the RDC/TMD. Despite those diagnostic criteria are currently under revision and update (16, 17), the data presented in this investigation were recorded according to validated Italian translation of the original 1992 version (9), which allowed multiple axis I physical diagnoses and investigated for axis II psychosocial impairment. The study procedures were approved by the Ethical Committee of the University of Padova.
The axis II GCPS, which was here used to set the main criterion for inclusion in the investigation, was originally developed by Von Korff et al. (10). Its validity has been tested in a large population survey, and the prognostic value has been tested in a 3-year follow-up study in large samples of primary care pain patients, also including patients with TMD pain (18).
The GCPS is composed of six items assessed on a 10-point scale and one item on the number of disability days due to facial pain. These items are suitable for self-report use and, even though the characteristics of the scale enable measuring pain dysfunction as a continuous variable, the authors have provided hierarchical criteria to grade pain dysfunction into ordinal categories. The scoring criteria are simple to use and allow categorising pain patients into five levels of chronic pain grades (0, no disability; 1, low disability, low pain intensity; 2, low disability, high pain intensity; 3, high disability, moderately limiting; 4, high disability, severely limiting).
Axis I physical diagnoses were based on the following diagnostic groups: group I (a. myofascial pain; b. myofascial pain with limitation in mouth opening); group II (a. disc displacement with reduction; b. disc displacement without reduction with limited opening; c. disc displacement without reduction without limited opening); and group III (a. arthralgia; b. osteoarthritis; c. osteoarthrosis) (9).
All patients who satisfied the inclusion criteria were recalled and were asked to attend the clinic for a follow-up assessment of their TMD signs and symptoms during the period from September to December 2011. The follow-up evaluation was again performed according to the RDC/TMD guidelines, with the aim to gather data on the natural course of axis I diagnoses. Additional information on the use of any treatment regimens during the time span between the first visit and the follow-up assessment was also collected.
Descriptive data on the number of patients receiving each of the specific axis I diagnoses at both evaluation points were presented for discussion along with a quantitative measurement of significance of the changes in the number of subjects with each specific diagnoses from baseline to follow-up (chi-square test). The level of significance was set at P < 0.05, and the procedures were performed with the software SPSS 19.0.*
RESULTS
Of the 86 patients who satisfied the criteria for eligibility in the study, 8 could not be reached because of address and/or telephone number changes with respect to the data included in the database, and 9 were not willing to participate to the investigation because they lived too far from the clinic or they had work-related duties that prevented them to attend the appointment. One of those nine subjects admitted to use painkillers for a tension-type headache associated with her TMD symptoms, and another subject referred a worsening of her pain symptoms that forced her to seek for treatment in a private clinic. The other seven subjects referred an absence of advice-needing TMD signs or symptoms during the time from the first appointment. The remaining 69 patients (79% females; mean age 47.4 11.3 years; range 26–77) accepted to attend the TMD Clinic for a follow-up assessment. The time span since the first visit ranged from 23 to 36 months.
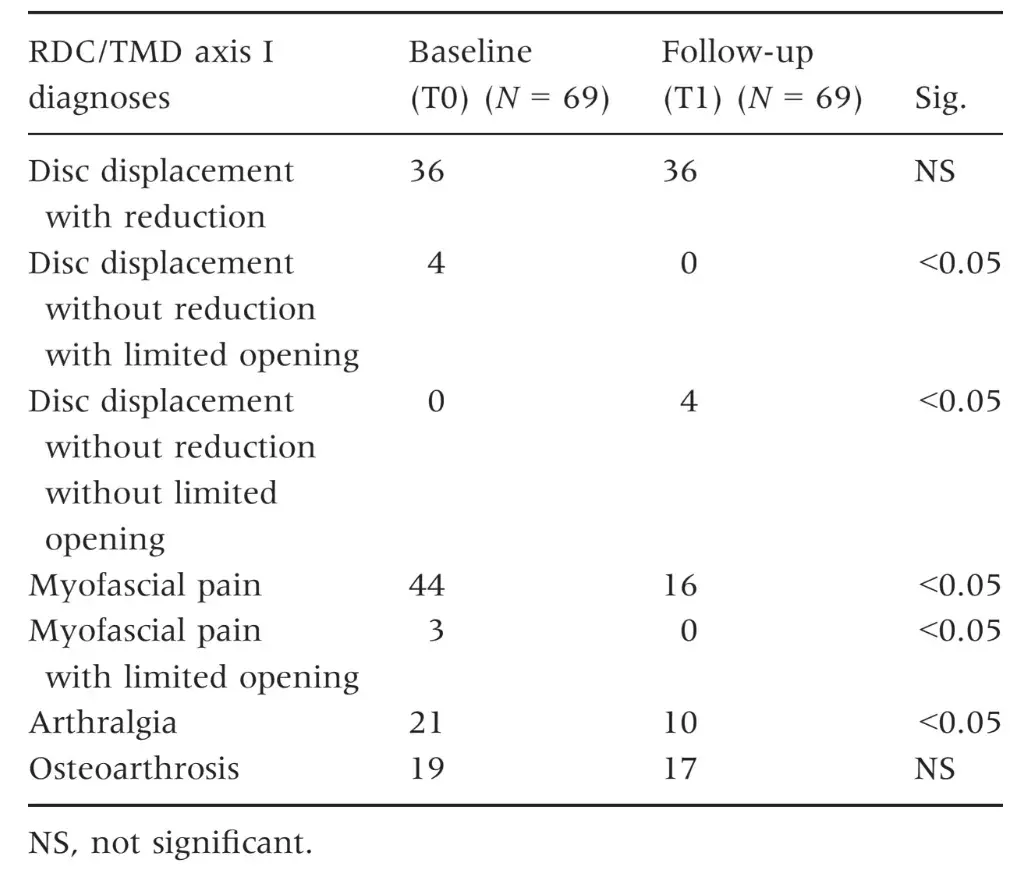
Baseline and follow-up diagnoses of the study participants were reported in Table 2. At the time of the first assessment, 68.1% of the patients received a muscle disorders (i.e. myofascial pain) diagnosis, 52.1% had disc displacement with reduction and 5.7% disc displacement without reduction with limited opening, 30.4% were diagnosed with arthralgia and 27.5% with osteoarthritis/osteoarthrosis of the temporomandibular joint. The follow-up assessment showed that the percentage of patients with muscle disorders decreased to 23.1% (P < 0.05), whilst disc displacement with reduction remained unchanged (52.1%) and 5.7% of patients had disc displacement without reduction without limited opening (P < 0.05). Diagnoses related to other joint disorders decreased to 14.4% for arthralgia (P < 0.05) and to 24.6% for osteoarthritis/osteoarthrosis.
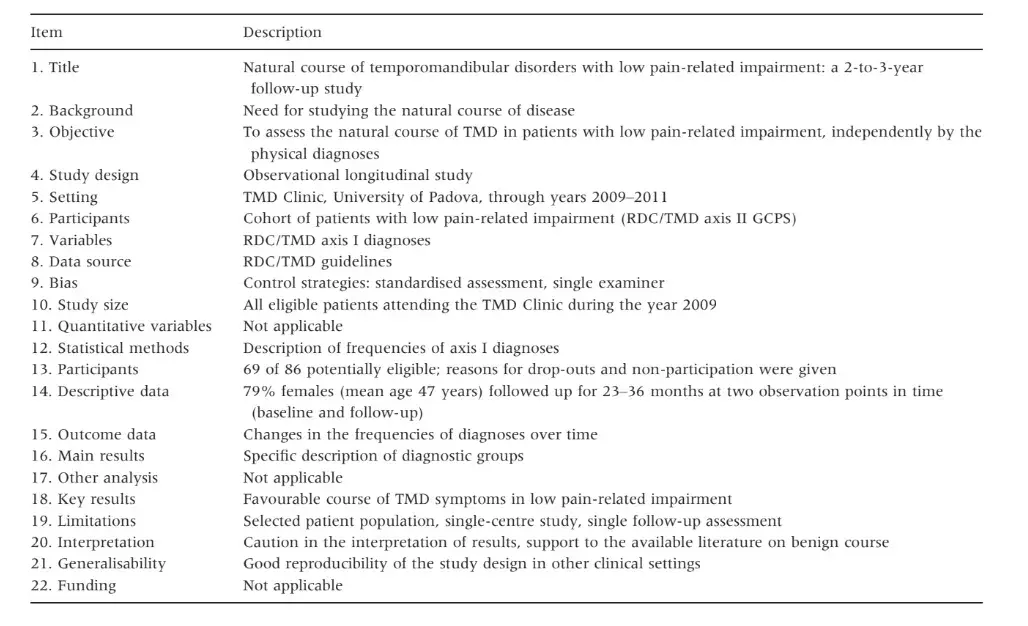
As for the course of the different RDC/TMD axis I diagnoses, more than half of the patients who had a diagnosis of muscle disorder did not receive any muscle disorder diagnoses at the follow-up appointment, with the percentage of subjects who were free from muscle pain increasing from 31.8% at baseline to 76.8% at the follow-up (Fig. 1). As for disc displacements, subjects with disc displacement with reduction at baseline showed the same diagnosis at follow-up, and all the four subjects who at baseline had limited opening due to disc displacement without reduction improved their mouth opening at follow-up and received a diagnosis of disc displacement without reduction without limited opening (Fig. 2). As for the other joint disorders, more than half of the patients who had arthralgia at baseline received no joint disorders diagnoses at follow-up (Fig. 3). None of the patients referred the use of painkiller drugs on a regular basis or received any treatments by other clinicians during any periods of the follow-up span.
In summary, the natural course of disease in the patients’ group included in this investigation was favourable, with no subjects showing worsening of symptoms, except than the individual who dropped out from the follow-up assessment and referred to have sought for treatment in the meanwhile.
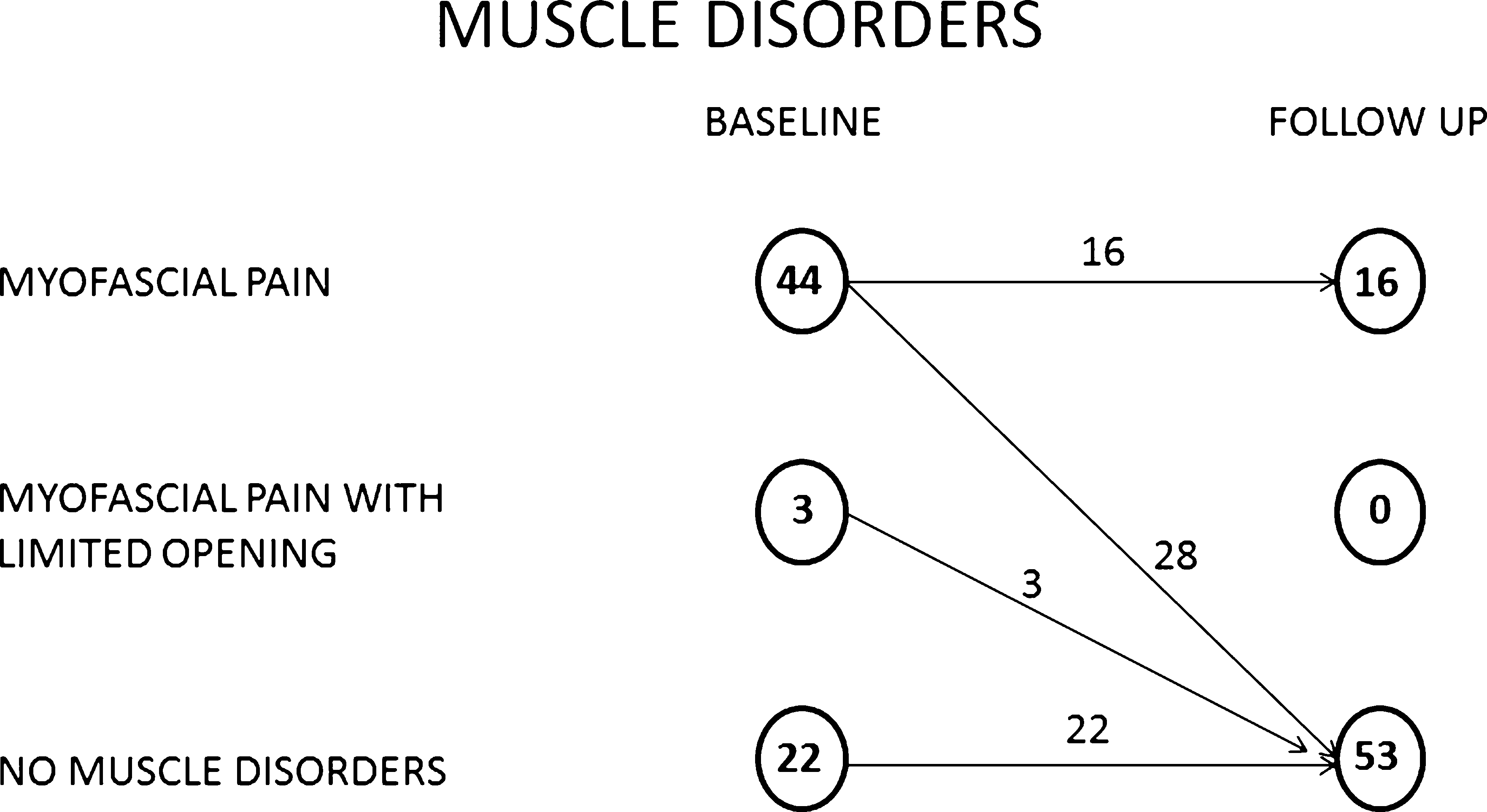 Fig. 1. Flow-chart of patients receiving the different muscle disorders diagnoses at baseline and follow-up.
Fig. 1. Flow-chart of patients receiving the different muscle disorders diagnoses at baseline and follow-up.
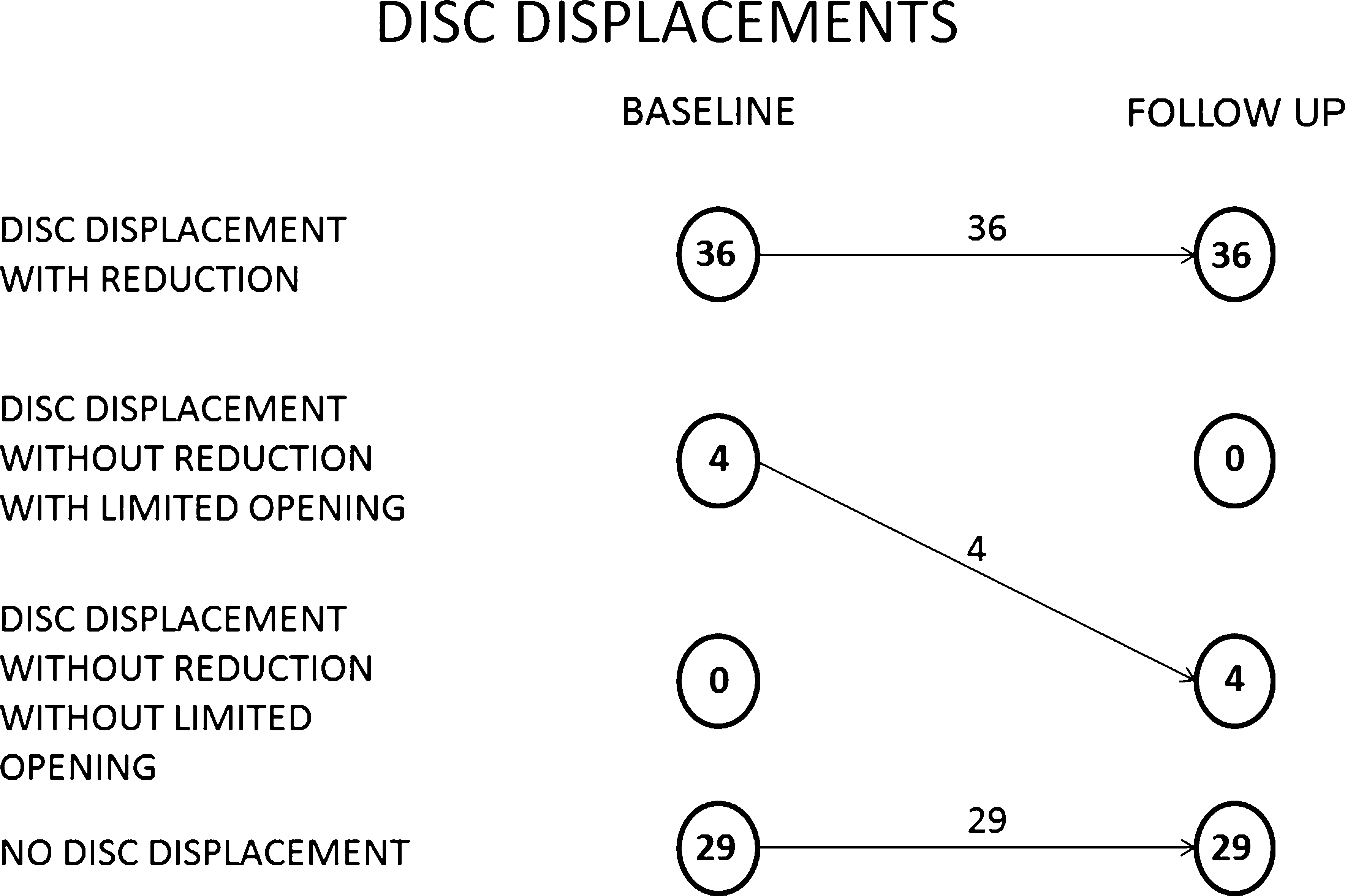 Fig. 2. Flow-chart of patients receiving the different disc displacement diagnoses at baseline and follow-up.
Fig. 2. Flow-chart of patients receiving the different disc displacement diagnoses at baseline and follow-up.
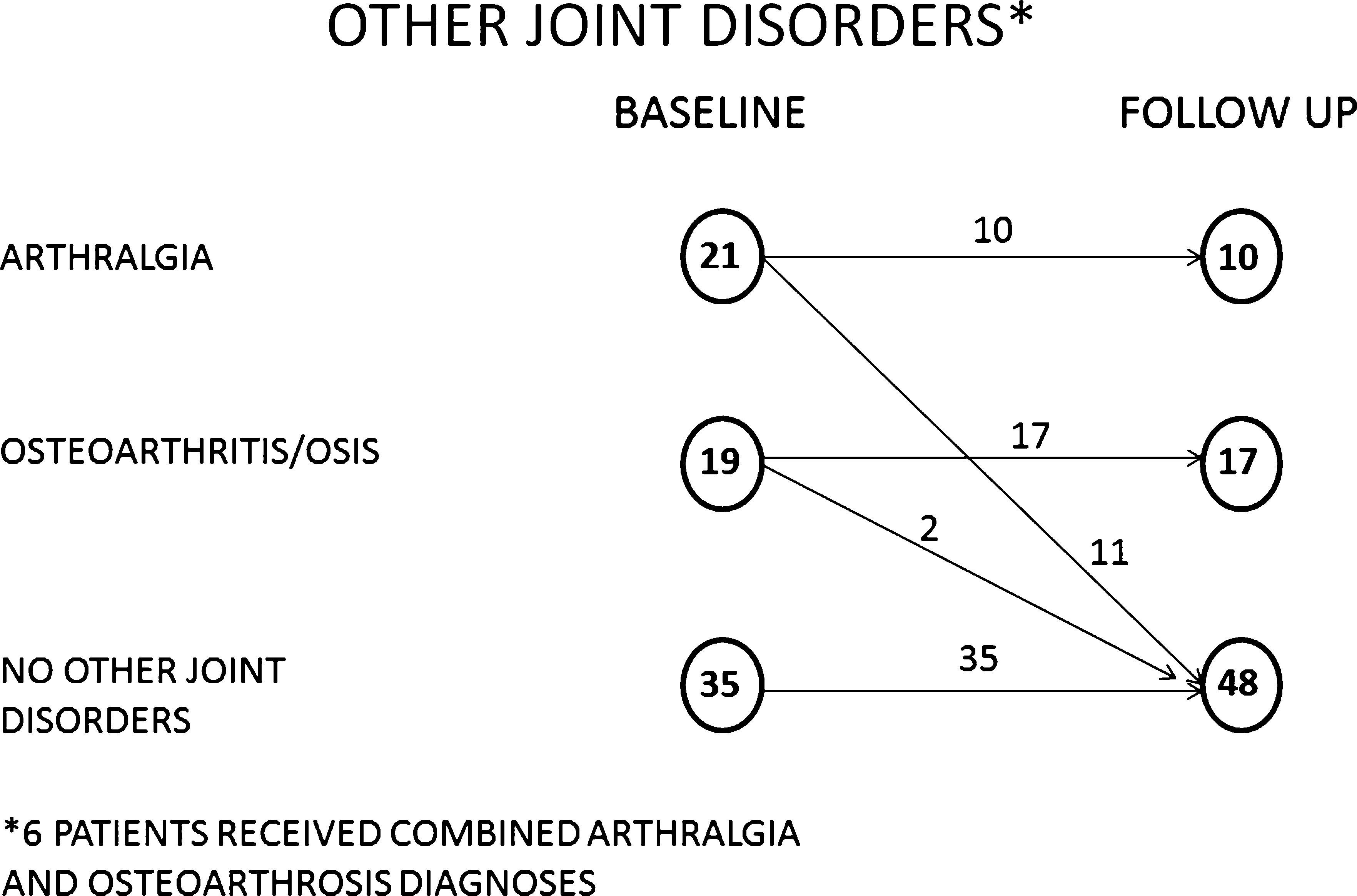 Fig. 3. Flow-chart of patients receiving the other joint disorders diagnoses at baseline and follow-up.
Fig. 3. Flow-chart of patients receiving the other joint disorders diagnoses at baseline and follow-up.
Table 2. Number of patients receiving the different RDC/TMD axis I diagnoses at baseline and follow-up
DISCUSSION
The literature on the epidemiology of TMD suggested that the majority of patients have a positive symptoms’ course (19, 20). Also, there is an increasing evidence in support of the importance of psychosocial factors in the field of TMD practice (21). The two statements above, viz., ‘TMD patients have a benign course’ and ‘TMD patients have some sort of psychosocial impairment’, are apparently in contrast and may be source of misinterpretation. Indeed, the overwhelming amount of papers on the relationship between TMD and psychological/psychosocial symptoms seems to suggest erroneously that most patients with TMD are impaired from a psychosocial view-point, almost crippling the so-called biopsychosocial model on which the TMD practice should be based (22). Based on this premise, knowledge on TMD epidemiology should be implemented by a more detailed description of both axis I, viz., physical and axis II, viz., psychosocial, assessment of patients with TMD.
Descriptive prevalence data have been gathered in large sample multicentre investigations (12), but information on the natural course of TMD symptoms in specific populations of patients with certain levels of psychosocial impairment was missing.
The present investigation attempted to describe the natural course of TMD signs and symptoms in patients with the lowest levels of pain-related impairment, viz., those subjects who were rated 0 or 1 in the GCPS. The main overall finding was that a positive course over a 2-to-3 year span was described, with self-remission of symptoms in most cases, independently by the physical diagnoses (i.e. muscle, disc, or other joint disorders) received by the patients at base-line. Importantly, no patient reported worsening of symptoms, neither in terms of frequent pain recurrence and/or worsening nor in terms of negative evolutions from disc displacement with reduction to disc displacement without reduction. More than half of the muscle or joint pain patients were symptom-free at the recall appointment, and all the four subjects who had a non-reducing displaced disc with limited opening at baseline improved to the same condition without limited opening. Also, no patients underwent any treatments or painkiller regimens during the follow-up period.
These data are in agreement with literature suggestions that the evolution of muscle and joint disorders is generally positive (5, 7, 8) and with longitudinal observations that only a minority of patients with disc displacement with reduction progress towards a diagnosis of disc displacement without reduction (23, 24).
Thus, past beliefs that disc displacements go through staged phases of anteriorisation that inevitably end in a non-reducing displacement have been shown to be wrong. Also, the findings supported the broader concepts that patients with low psychosocial impairment respond well to conservative treatments (14), that a diagnosis based on axis I findings is not enough to explain a treatment seeking behaviour by the patients’ side (12), that psychosocial factors are more important than physical ones to predict treatment effectiveness (13) and that intervention aiming to manage the psychosocial component of pain is useful to reduce risks of pain chronicisation (25). Unfortunately, a common shortcoming to many of the studies on the natural course of TMD symptoms is that they were performed on selected population of patients not taking into proper account for the axis II evaluation to explain the natural course of disease.
The present investigation was designed to maximise the external validity (26), because the inclusion criteria, the diagnostic approaches, the follow-up strategy and, more in general, the study design, can be easily replicated in other clinical settings.
Also, the STROBE guidelines for reporting observational studies were followed as well as a detailed checklist summarising the main study features in accordance with the STROBE statement was provided to ease readability of the manuscript. Notwithstanding that it must be borne in mind that this strategy, even if allowing a potential ‘generalization’ of the findings, is not free from internal validity problems (27). Indeed, despite efforts have been made to mine all the data that were available on the university hospital database, one cannot exclude that a super-selected population of patients who are more prone to a positive evolution of their symptoms was included in the study. Such a risk may be confirmed by the fact that the one subject who dropped out was the one with worsening symptoms.
On the other hand, this is a potential bias in common with many longitudinal studies relying on subjects’ reporting back, and it has to be taken into proper account when describing the reasons for dropping out. Moreover, the single follow-up observation point may not be enough to detect symptoms’ fluctuations over time, so that the adoption of multiple observation points, possibly in combination with the use of pain diaries are recommendable strategies to implement the internal validity of findings. The clinical implications of these findings should also be reappraised in the light of the ongoing reconceptualisation of the therapeutic role of placebo and patients’ counselling and reassurance (28), here assumed as strategies not influencing the ‘natural’ course of disease.
For the above reasons, findings from this investigation can be viewed as a pilot data pool for comparison of future researches. On the other hand, it must be borne in mind that other study designs are hard to perform to investigate the natural course of disease on more psychosocially compromised patients, due to obvious ethical reasons that prevent from putting patients with high levels of pain-related impairment on a waiting or observation list.
So, within the limitations of this study, support to the importance of an axis II evaluation has been provided, and a strong recommendation for integrating the physical and the psychosocial assessments seems to emerge as a suggestion for designing future investigations with an increased validity of clinical and research findings.
You have the opportunity to gather more in-depth information about temporomandibular disorders diagnosis and functional treatment in our course "Evidence-based treatment of TMJ dysfunction" .
CONCLUSIONS
In a sample of 69 patients with TMD with low pain-related impairment followed up with a single recall assessment at 2-to-3 years, the natural course of disease was generally favourable. The findings support the need for identifying TMD populations based on their psychosocial impairment as an important issue to consider when assessing TMD epidemiology.
References
McNeill C. History and evolution of TMD concepts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:51–60.
Greene C. The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain. 2001;15:93–105.
American Association for Dental Research. AADR TMD policy statement revision.
Manfredini D. Fundamentals of TMD management. In: Manfredini D, ed. Current concepts on temporomandibular disorders. Berlin: Quintessence Publishing; 2010:305–318.
De Leeuw R, Boering G, van der Kuijl B, Stegenga B. Hard and soft tissue imaging of the temporomandibular joint 30 years after diagnosis of osteoarthrosis and internal derangement. J Oral Maxillofac Surg. 1996; 54: 1270–1280.
Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res. 1998;77:361–365.
Rammelsberg P, LeResche L, Dworkin S, Mancl L. Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 2003;17:9–20.
Kalaykova S, Lobbezoo F, Naeije M. Two-year natural course of anterior disc displacement with reduction. J Orofac Pain. 2010;24:373–378.
Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355.
Von Korff M, Dworkin SF, Leresche L. Graded chronic pain status: an epidemiologic evaluation. Pain. 1990;40: 279–291.
Manfredini D, Winocur E, Ahlberg J, Guarda-Nardini L, Lobbezoo F. Psychosocial impairment in temporomandibular disorders patients. RDC/TMD axis II findings from a multicentre study. J Dent. 2010;38:765–772.
Manfredini D, Ahlberg J, Winocur E, Guarda-Nardini L, Lobbezoo F. Correlation of RDC/TMD axis I diagnoses and axis II pain-related disability. A multicenter study. Clin Oral Investig. 2011;15:749–756.
Manfredini D, Favero L, Del Giudice A, Cadorin C, Guarda-Nardini L. Axis II psychosocial findings predict effectiveness of TMJ hyaluronic acid injections. Int J Oral Maxillofac Surg. 2013; 42: 364–368.
Dworkin SF, Huggins KH, Wilson L, Mancl L, Turner J, Massoth D et al. A randomized clinical trial using research criteria for temporomandibular disorders-Axis II to target clinic cases for a tailored self-care treatment program. J Orofac Pain. 2002;16:48–63.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577.
List T, Greene CS. Moving forward with the RDC/TMD. J Oral Rehabil. 2010;37:731–733.
Schiffman EL, Truelove EL, Ohrbach R, Anderson GC, John MT, List T et al. The Research Diagnostic Criteria for Temporomandibular Disorders. I: overview and methodology for assessment of validity. J Orofac Pain. 2010;24:7–24.
Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–149.
De Bont LGM, Dijkgraaf LC, Stegenga B. Epidemiology and natural progression of articular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:72–76.
Stohler CS. Phenomenology, epidemiology, and natural progression of the muscular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:77–81.
Suvinen TI, Reade PC, Kemppainen P, Kon€ onen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9:613–633.
Palla S. Biopsychosocial pain model crippled? J Orofac Pain. 2011;25:289–290.
de Leeuw R, Boering G, Stegenga B, de Bont LG. Clinical signs of TMJ osteoarthrosis and internal derangement 30 years after nonsurgical treatment. J Orofac Pain. 1994;8:18–24.
Kononen M, Waltimo A, Nystrom A. Does clicking in adolescence lead to painful temporomandibular joint locking? Lancet. 1996;347:1080–1081.
Gatchel RJ, Stowell AW, Wildestein L, Riggs R, Ellis E III. Efficacy of an early intervention for patients with acute temporomandibular disorder-related pain: a one-year outcome study. J Am Dent Assoc. 2006;137:339–347.
Palla S, Farella M. External validity: a forgotten issue? J Orofac Pain. 2009;23:297–298.
Shamliyan TA, Kane RL, Ansari MT, Raman G, Berkman ND, Grant M et al. Development quality criteria to evaluate nontherapeutic studies of incidence, prevalence, or risk factors of chronic diseases: pilot study of new checklists. J Clin Epidemiol. 2011;64:637–657.
Greene CS, Goddard G, Macaluso GM, Mauro G. Topical review: placebo responses and therapeutic responses: how are they related? J Orofac Pain. 2009;23:93–107.
