Miller classification of gum recession
Machine translation
Original article is written in RU language (link to read it) .
The original classification of gum recession, more than three decades ago, described four classes of recession. For example, Miller class III recession included several variations without complete root coverage. However, today, new surgical techniques have allowed clinicians to potentially achieve complete root coverage for interdental bone loss. Currently, in dentistry, an important role is assigned to the interdental papilla. This article presents a new classification of interdental papilla shape that emphasizes the importance of papilla width and height. In addition, an updated classification of periodontal terms will be presented.
More useful up-to-date information about gum recession in the webinar Localized recession: definition, classification, etiology and risk factors .
The original article, published more than 30 years ago, described four classes of recession in the classification. A common feature of Miller class I and class II recession was the absence of interalvelar bone or soft tissue loss. The difference between Class I and Class II recession was whether the recession extended beyond the periodontal attachment.
However, the original article did not emphasize the distinction between attached and nonattached gingiva. Class III recession indicated two variants in which there was no complete root closure. The first case described an extracted tooth without loss of interalveolar bone or soft tissue, while the second, on the contrary, was associated with loss of bone and soft tissue. New surgical techniques allow the clinician to achieve complete root coverage in cases of interalveolar bone loss. Miller class lV describes interdental recession with absence of the papilla, which means the root cannot be covered.
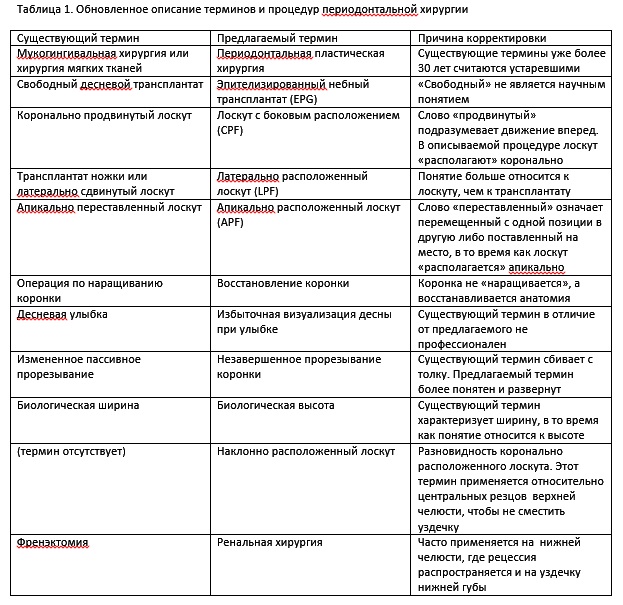
Since there is some confusion in periodontal terminology that requires revision, a new classification of these terms will be presented (Table 1).
Periodontal plastic surgery
When the original classification of marginal gingival recession was published, periodontists emphasized the treatment of periodontal disease rather than esthetics. The operation not related to the disease was called mucogingival surgery. Since the introduction of the concept of periodontal plastic surgery, periodontics has entered a new stage of development.
Unlike mucoginval surgery, periodontal plastic surgery sought not only to achieve the maximum functional result, but also to achieve an aesthetic component. At the same time, treatment options for marginal recession were limited to lateral (LPF) and lateral placement of flaps (CPF), and on the palatal side, placement of epithelialized graft (EPG).
Despite the positive esthetic results from the use of LPF and CPF, EPG had serious disadvantages that not only led to repeated surgery, but also to discoloration of the gingiva with subsequent proliferation of connective tissue leading to scar formation.
A breakthrough in the treatment of recession occurred with the presentation of subepithelial connective tissue (SCTG). In this method, the graft was covered with SCTG, which provided bilaminar circulation, additional blood supply and improved graft survival. The graft was removed from the palatal side, which reduced discomfort. Allograft and xenograft materials were replaced with native tissue, which avoided damage to the palate.
Thus, taking into account the development of surgical methods for treating recession, Miller's original classification has been expanded and a new classification of the gingival papilla has been added.
Class I and II recession
Class I and II recessions are characterized by preservation of bone or soft tissue, suggesting complete root coverage. The difference between the two classes is the presence or absence of attached gingiva (Figure 1).

Fig.1 Class I recession. Note that the free gingival groove separates the unattached gingiva from the attached gingiva.
Class I recession was initially described as recession that did not extend to the periodontal junction (MGJ). If the gums remained on the vestibular surface, then this option was classified as class I recession. In fact, if the gum is not attached, there is a “hidden recession”, it should be classified as a class II recession (Fig. 2).

Fig.2 Class II recession. Although the labial surface may have retained gingiva, if it is not attached, it is a Class II recession. The only way to accurately determine this is to check whether the probe extends beyond the periodontal attachment.
Thus, in places where the gum is present on the vestibular surface, it is necessary to carefully examine it and determine whether it is attached or not attached.
Although complete root coverage is achieved in both Class I and Class II recessions, the treatment modalities may vary. For example, if normal keratinizing epithelial tissue is present in Class I recession, the simplest root coverage procedure, CPF, may be suggested. whereas in class II recession, a soft tissue flap will be required. Treatment of class II recession requires more complex tissue grafting procedures. Combining classes I and II into one classification point may lead to confusion when choosing treatment. In the author's opinion, the new classification of recession presented at the 2017 World Workshop on the Classification of Periodontal Diseases did not take this into account.
Class III Recession
Class III recession was initially described as loss of interalveolar bone and/or soft tissue or tooth extraction. In this clinical case, only partial root coverage can be achieved. This is achieved by using tunnel technology; further root closure in class III recession can be achieved, but not in all cases (Fig. 3 and Fig. 4). At the time of the original classification, the emphasis of periodontal treatment was on maintaining gingival health and function rather than on gingival aesthetics. More often than not, the underlying problem was aesthetic rather than functional, and attempting to partially cover the root was not even considered. 
Fig. 3 Class III recession (Fig. 3) was originally described as bone and/or soft tissue loss or tooth extraction. Only partial root coverage can be achieved. Using a tunnel technique, peeling and lifting the papilla can provide additional root coverage in some class III recessions (Figure 4).

Rice. 4
Class IV Recession
In class IV recession, regardless of its severity, root coverage cannot be achieved because there is no interdental papilla (Fig. 5).

Fig. 5 In class IV recession, regardless of the severity of the recession, complete root coverage cannot be achieved because there is no papilla.
The importance of interdental papillae in flap root coverage
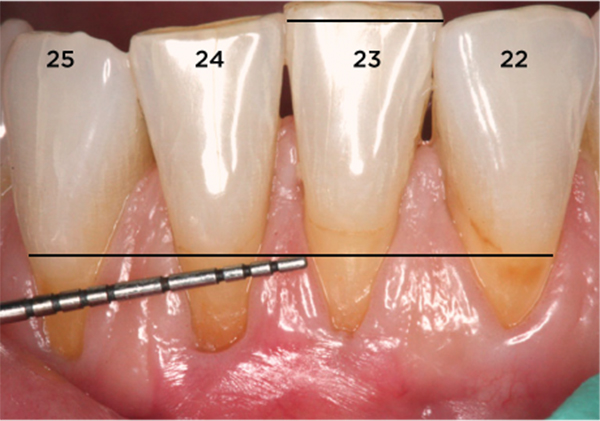
In 1992, Tarnow et al demonstrated that the height of the normal interdental papilla is 5 mm. In 1998, Nordland and Tarnow published a classification of interdental papillary recession. However, it did not take into account the width or vestibulo-lingual size of the papilla. With the advent of the tunnel technique, the interdental papillae acquire normal volume, especially in the mesio-distal direction. A papilla of sufficient size on the vestibular surface provides good blood supply to the graft. This helps to improve root closure in approximal areas according to Miller class III.
Classification of interdental papillae
Based on the author's observations, papillae can be divided into three types: A, B and C (Table 2).
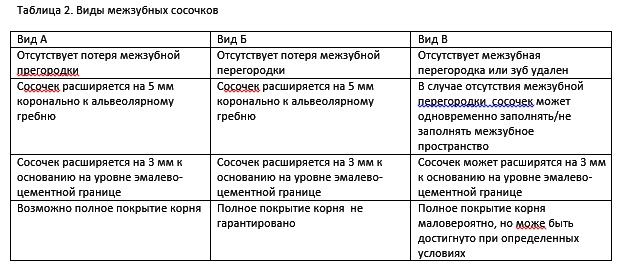
Type A and type B are similar in that the interalveolar bone is preserved. The papilla extends 5 mm coronally to the alveolar ridge.
They differ in width. A type A papilla is ≥3 mm wide at the base (Fig. 6), and a type B papilla is <3 mm wide (Fig. 7). A type C papilla is characterized by the absence of interalveolar bone tissue or tooth loss (Fig. 8). That is, in all cases in the absence of interalveolar bone, the papilla is classified as type C.

Rice. 6 Class II recession with type A papillae. Papillae ≥3 mm.

Fig. 7 Class II recession with type B papilla between the central incisors. Papilla <3 mm.
Rice. 8 The papilla between teeth 2.4 and 2.5 is type A. The papilla between teeth 2.2 and 2.3 is type C. Note the interdental recession distally on tooth 2.3 and mesially on 2.2
Where bone loss is present, the papilla may enlarge ≥5 mm towards the crown. It is sometimes difficult to identify and accurately classify a papilla as type C because the shape of the papilla does not always correspond to the shape of the bone. Since there is bone loss in the interdental space, but the papilla remains unchanged, hidden recession is observed. A distinctive feature is the loss of the interdental septum. The width of the type C papilla may be ≤3 mm.
Class I and class II recessions have papillae of type A or type B. Class III recession has a type C papilla, and class IV recession does not have a papilla. Type A papillae provide a favorable environment for graft survival, whereas type B papillae provide a more limited source of blood supply and stability as their width tapers, reducing the predictability of complete root coverage.
In the anterior maxilla, the width of the type A papilla is ≥3 mm. On the contrary, in the lower jaw, the interdental papillae are rarely wide, especially when the teeth are crowded. Width, height, and distance from the ridge affect the amount of root coverage that can be achieved with Class III recession. Clinical experience shows that adequate papillary width is necessary for adequate blood supply and placement of the suture on soft tissue.
Conclusion
With the advent of tunneling technology and subsequent modifications, complete root coverage in Class III recessions has become possible. The shape of the papillae becomes an important factor in such areas. In addition to the features of the Type C papilla described above, the papilla must have sufficient volume in the labiolingual direction to survive movement toward the crown. Under ideal conditions, an increase in papillary height of up to 2 mm can be achieved. Advantages of the tunnel technique include complete graft coverage, delamination and elevation of interdental papillae, and avoidance of external vertical or horizontal incisions.
Learn more about this topic in the online course Advanced Treatment of Periodontal Diseases .
https://www.aegisdentalnetwork.com/
