Lateral Sinus Lift with Oseodensification of Sticky Bone Graft with Si-PRF Technique and Placement of Implants in a Single Surgical Act
Abstract
The placement of implants in posterior sectors of the maxilla may entail the need for additional regeneration procedures, considerably increasing time for the patient and for clinicians. The need to optimize procedures in implantology has allowed us to execute new techniques that are capable of achieving excellent results in a single intervention. The technique presented below deals with the osseodensification of the sticky bone and the simultaneous placement of the implant.
Introduction
Replacement by means of implants in the posterior area of the maxilla is usually dependent on the previous performance of regenerative procedures prior to the placement of implants. This is due to the fact that after dental extraction, a high rate of bone resorption occurs physiologically, this is due to several reasons, on the one hand, to the low bone density of trabecular bone in the area, and to the alveolar deficit caused due to crest resorption and pneumatization of the maxillary sinus. The placement of implants in this anatomical area with bone resorption has always been a challenge for clinicians. Several surgical approaches have been published, mainly two, a lateral and a transcrestal approach [1]. Lateral sinus lift was introduced in 1980 by Boyne and James [2]. Although it is a procedure in which predictable clinical results are obtained, it is not exempt from risks and possible failures. In 2012, Wallace and Testori published a study in which they concluded that it presents a certain degree of morbidity, risk of perforation of the the membrane, delayed healing and postoperative infection [3]. For decision-making regarding the technique to choose, the MISCH4 classification has traditionally been used. All the cases presented in this study were grade IV where the residual bone height (AOR) is less than 4 mm and the treatment of choice to date has been sinus elevation through lateral access and deferred placement of the implants in a second surgical time. , after maturation of the antral graft.
In the retrospective clinical study published by Huwais et al [5]. They reported on various clinical strategies and bone instrumentation techniques, with the aim of increasing the bone density of the posterior maxilla, thus achieving improved implant stability. Pre-preparation of the osteotomy to place a wider tapered implant, and a mallet osteotome to facilitate bone condensation, have been used with variable success. In the retrospective study Rosen et al, published a 95% survival rate in 174 implants that used osteotomes to achieve osteocompression in combination with membrane elevation in a 20-month multicenter follow-up study, they also concluded that the rate was reduced to 85% in sites with inferior subcrestal alveolar height of 4mm or less [7]. The osseodensification drilling technique was proposed to improve local bone quality and implant stability in low-density alveolar ridges, being developed by Dr. Huwais in 2013, this system of specially developed drills (Densah burs, Versah) by Dr. Huwais in 2013, allowing an increase in bone density, bone quality and bone expansion [8]. The objective of the present investigation was to show the effectiveness of the osseodensification technique for the preparation of the implant bed through a treatment plan consisting of sinus elevation through a lateral approach with osseodensification of the sticky bone graft, using the technique described by Hernández 2021 (Si-PRF) [9], a novel technique, which advocates the use of specific counterclockwise drills, which favors bone expansion and condensation of the patient’s bone and the bone graft in areas where there is less than 4mm of remaining bone.
The bone graft material (CORTI-OSS® - CORTICO/MEDULAR) was densified in the sinus with the drills at low speed (100 rpm) in a counterclockwise direction without irrigation. After sinus lift, a switched platform implant (MIS Implants) with internal connection was placed. In this article, the author proposes a novel technique, osteodensification of sticky bone graft.
Due to this technique, it is possible for the bone to condense towards the osteotomy walls at the same time as the implant site preparation surgery and implant placement in a single surgical act. Currently, the evolution of the techniques and materials used by doctors make it possible to place implants in very complicated situations where, just a few years ago, surgeons would not have been able to make a minimally invasive therapeutic choice.
Materials and Method
This retrospective analysis followed the Declaration of Helsinki of the Medical Association World and the directives given by the Egas Moniz Ethics Commission (CEEM) at Egas Moniz Cooperativa de Ensino Superior, Monte de Caparica, Portugal, which does not require ethical approval for retrospective clinical studies. All the patients included in the study signed an informed consent, both for the clinical procedure and for the follow-up appointments. All treatment steps and data collection were part of the routine procedures at the centers and no additional steps were taken for the study. The study was structured following the STROBE statement [10].
Selection criteria and surgical technique
Patients who presented dental lack in the upper maxillary posterior area were evaluated. The inclusion criteria were patients who presented a pneumatized maxillary sinus and a height of less than 4 mm of remaining bone in the area to be operated on. The exclusion criteria are patients with a preexisting uncontrolled systemic condition, smokers, who have received radiotherapy or are taking antiresorptive medication. All patients underwent cone beam computed tomography (CBTC) before and after the surgical procedure. All interventions were performed by experienced surgeons, who followed a standardized surgical technique. Before performing the surgical procedure, venipuncture was performed to draw blood and make a bone block (Sticky Bone), under the Si-PRF protocol, which is reserved for later use (Figure 1 & 2). After anesthesia with lidocaine/epinephrine 20mg/ml + 0.0125mg/ml, a lateral window is performed to approach the area for lateral sinus elevation (Figure 3), after elevating the sinus membrane, bone densification is performed at 800 RPM in the opposite direction. clockwise with copious irrigation and in small increments (standard protocol, Densah®(Versah, LLC, Jackson, MI, USA) in the area where the implants will be placed (Figure 4), then placed within the sinus cavity the sticky Bone and proceed to osseodensify it at 100 RPM counterclockwise and without irrigation through the same orifice planned for the placement of the implants (Figure 5 & 6), placement of dental implants in the planned area (Figure 7), coverage of the sinus window with Si-PRF membranes and closure of the operated area with monofilament suture (4/0) (Figure 8 & 9).
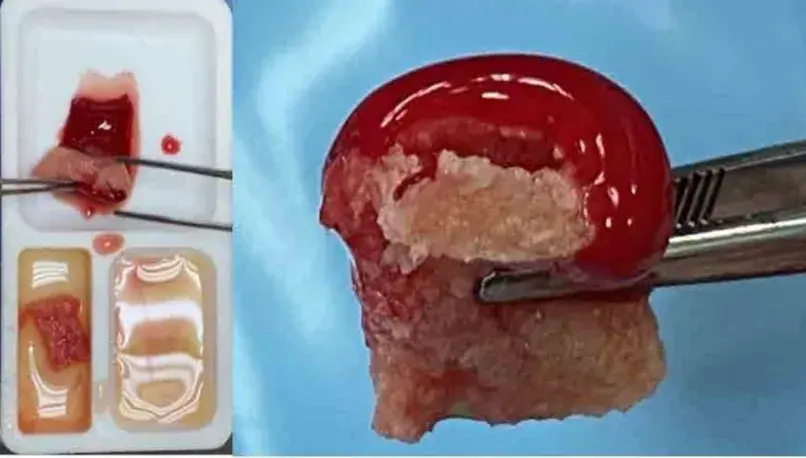 Figure 1 & 2: Preparation and Sticky Bone, according to the Si-PRF technique.
Figure 1 & 2: Preparation and Sticky Bone, according to the Si-PRF technique.
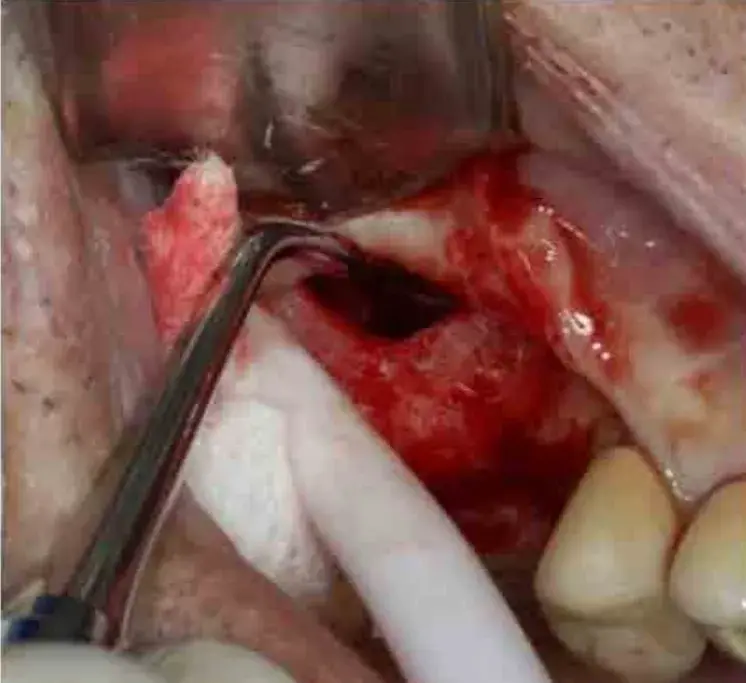 Figure 3: Sinus Elevation.
Figure 3: Sinus Elevation.
 Figure 4: Osseodensification of the area where the future implants will be placed.
Figure 4: Osseodensification of the area where the future implants will be placed.
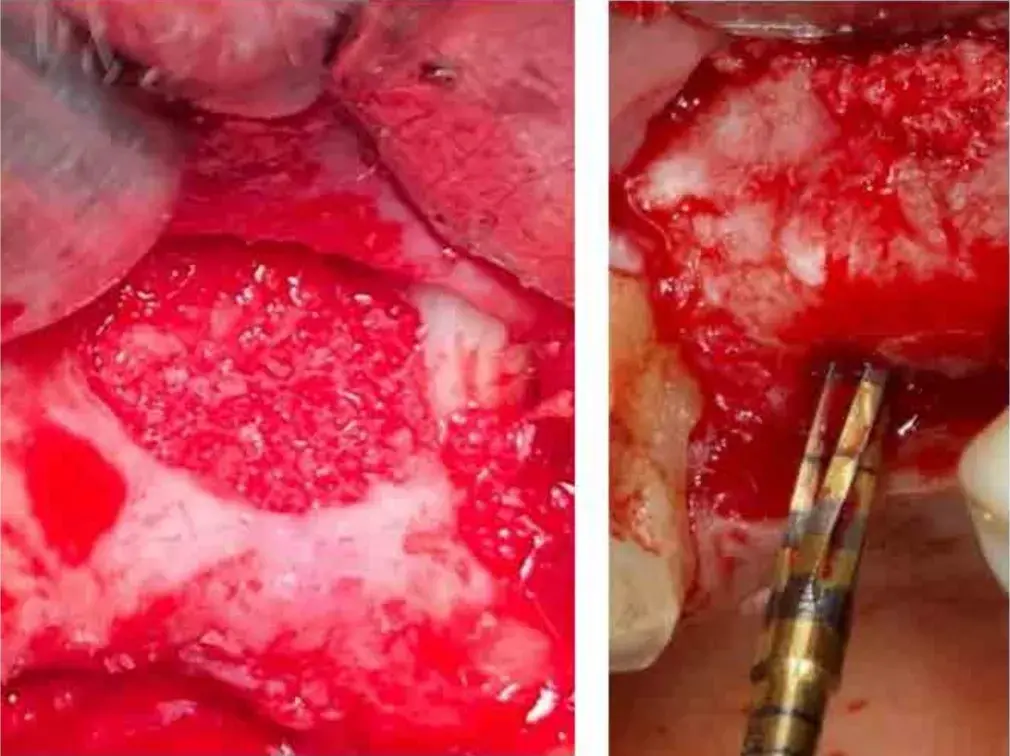 Figure 5 & 6: Sticky Bone inside the Sinus cavity and its Osseodensification at 100 RPM.
Figure 5 & 6: Sticky Bone inside the Sinus cavity and its Osseodensification at 100 RPM.
 Figure 7: Placement of implants at 30 N/cm in the area.
Figure 7: Placement of implants at 30 N/cm in the area.
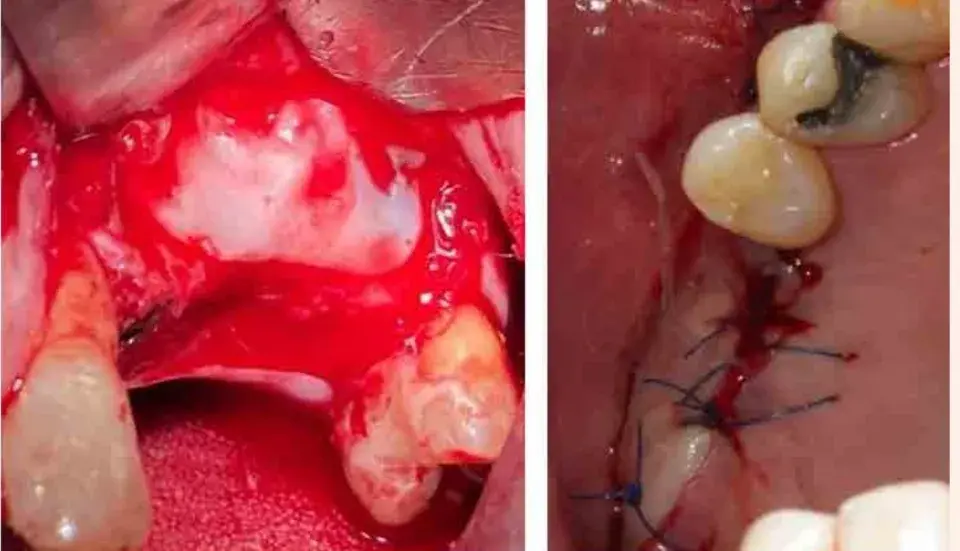 Figure 8 & 9: Coverage of the sinus window with PRF membrane and closure of the area.
Figure 8 & 9: Coverage of the sinus window with PRF membrane and closure of the area.
Result
All the data were recorded before and after the surgical intervention in the area where the implants were placed, for later analysis, Misch classification, bone height, Housfield Units (HU) were measured, and the initial anchorage of the implants was measured in Newton at the time of placement (Table 1).
A total of three patients were included, 2 men and one woman, with an average age of 68 years (range 6572), where 4 surgical procedures of the described technique were performed, all of them had an edentulous area with more than 5 years of evolution and were performed in the upper maxillary area of the molars. The mean follow-up of the patients was 6 months. In the CBCT, an initial residual bone height of 2.66 mm on average (range 2.19-3.34 mm) was observed up to the maxillary sinus, Misch grade IV classification, and after the procedure 14.97 mm (range 11, 3418.32 mm), Misch grade I classification (Figure 9-11). Hounsfield Units (HU) were also measured before and after each intervened area, initially having an average of 221.5 HU (range 103-381 HU) and final results of 1040 HU (range 821-1205 HU) (Figure 9-11). All implants placed had an insertion torque above 30 Ncm (range 30-40 Ncm)
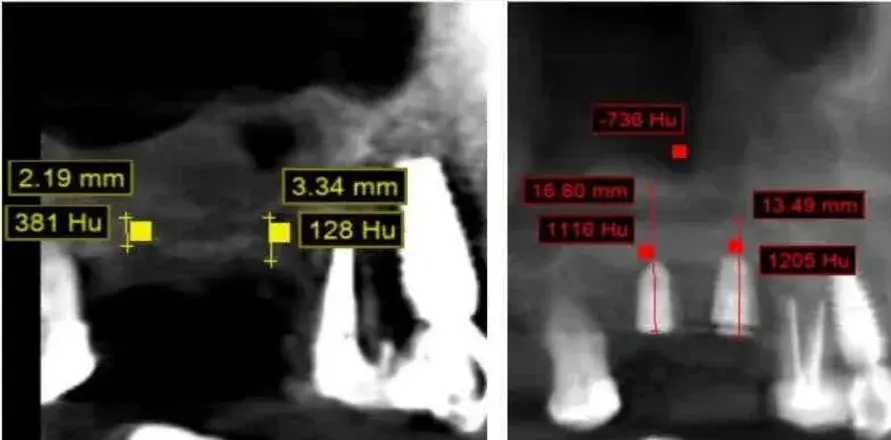 Figure 9: CBTC of patient 1, before and after surgery in area 16 and 17.
Figure 9: CBTC of patient 1, before and after surgery in area 16 and 17.
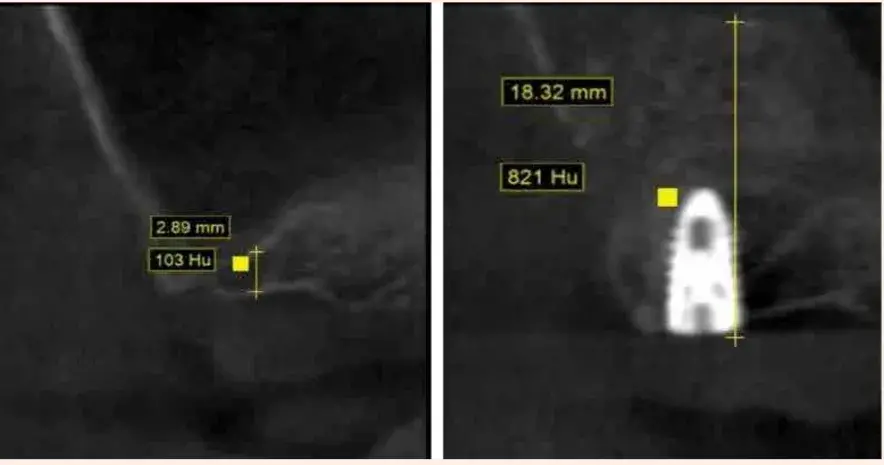 Figure 10: CBTC patient 2, before and after surgery in area 27.
Figure 10: CBTC patient 2, before and after surgery in area 27.
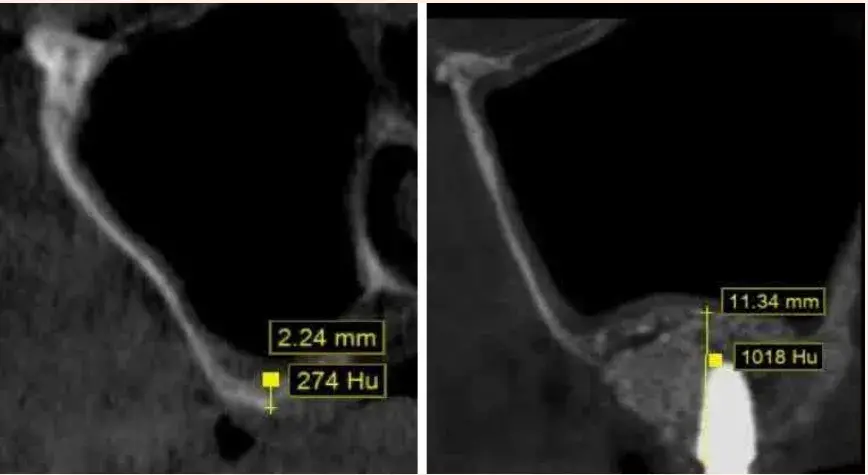 Figure 11: CBTC patient 3, before and after surgery in area 26.
Figure 11: CBTC patient 3, before and after surgery in area 26.
Table 1: (1a and 1b similar patient). Clinical cases performed. MISCH Cla. (Misch’s Maxillary Sinus classification), HU (Hounsfield Units). NW (Newton). MM (Millimeters of residual bone height on maxillary sinus).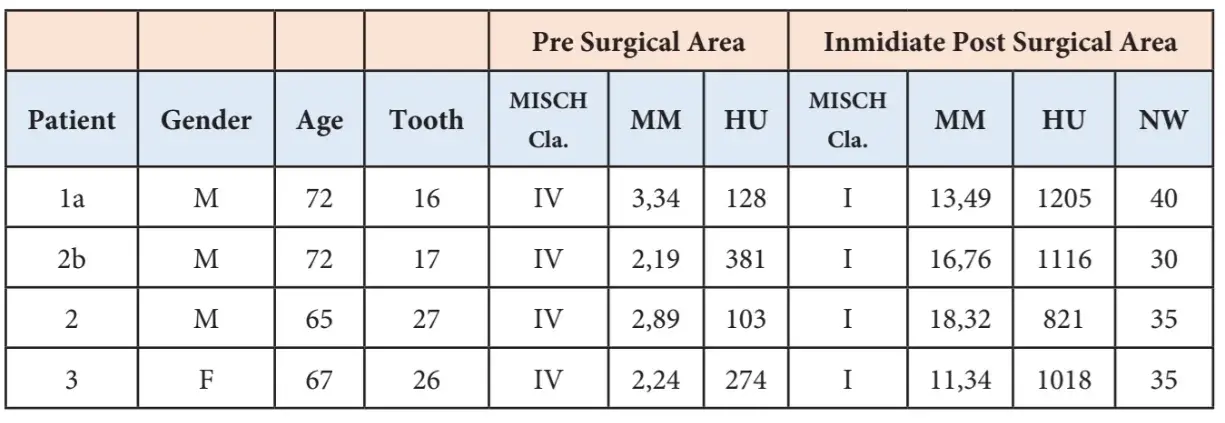
Discussion
In this radiological and clinical study, it was observed that it is possible to place implants in atrophic maxillar that present a residual bone height (RBA) in the maxillary sinus area of less than 4 mm in a single surgical act. Traditionally, the lateral window approach with delayed implant placement has been recognized as the surgical technique of choice in cases where the AOR is less than 5 mm due to the lack of primary implant stability in such situations [11-12]. The initial stability of the implant is the key factor for osseointegration and should be the main criterion for indicating simultaneous or delayed implants in the maxillary sinus [13] and is mainly determined by the quality (proportion between cortical and trabecular bone) and quantity of the alveolar bone. According to Rao PL et al. [14] and Elias C et al. Bone density is the main parameter for the mechanical stability of dental implants. Primary stability is directly related to bone quality [15,16].
In our study, we managed to increase the bone density (OD) of the graft, which allowed us to place the dental implant, where it was previously not possible to do so, in a single surgical act, we achieved an increase in bone density which could be quantified based on at the UH and described by Misch in his work on the relationship between UH and DO [17]. Hounsfield in 1980, shows that it is possible to quantitatively measure bone density (DO) and these are expressed in Hounsfield units (HU), taking as reference the value of 0 HU for the air and the bone goes in a range of 50 HU to 2500 HU, which objectively allows us to relate them to the OD scale described by Misch in which he establishes D1 (dense compact bone) >1250Hu, D2 (dense thick and compact trabecular bone) 850 - 1250Hu, D3 (fine and compact trabecular bone) 350 - 850 Hu and D4 (fine trabecular bone) <350Hu; Relating these results to those obtained in our study, we can show that we went from D4 bone to a D2 bone, after osseodensification.
A follow-up study by Tatli et al. [18] mentions that various available techniques, such as preoperative bone density assessment, subjective bone quality ratings, and insertion torque degree, were set to determine the conditions of the bone-implant interface. In our study, the insertion torque of the implants placed after bone graft osseodensification was above 30 NW. Conventional osteotomy is considered a subtractive surgery 19-20 because it extracts autologous bone from the implant insertion site, while the osteodensification technique compacts it and models it in favor of the implanted graft [21,22].
It can be noted that most of the studies analyzed confirm osteodensification in terms of maintaining the quality and quantity of autologous bone, which will have a significant influence on the outcome of implant surgery [23] because it ensures the primary stability of the implant. Placed [24]. A wide variety of studies consider PRF as a biologically active scaffold that induces the proliferation and differentiation of osteoblasts [25]. The osteoinductive properties of platelet concentrates favor bone regeneration and its clinical use is suggested as a valid protocol for the recovery of bone tissues in surgery oral and periodontics. In our study we used a scaffold made with the technique described by Hernández in 2021 called Si-PRF 9, which will allow an improvement in osseointegration and bone regeneration of the graft placed in the sinus cavity. Various alveolar preparation techniques have been described to increase the interface of the implant with the surrounding bone [26] to improve primary stability and osseointegration results. The implant-bone interface is important in terms of primary stability, reducing the possibilities of micromovements of the implant, which is one of the main causes of implant loss [27-28]. A multicenter retrospective clinical study with a follow-up of up to 5 years using a method that improves bone density and allows transcrestal sinus augmentation using a compaction graft [29]. In our study we managed to improve the implant-bone interface, primary stability and osseointegration results by using the combination of techniques (ossedensification-Si-PRF scaffolds).
Conclusion
Despite the limitations of this study: the small number of cases (4), performed on three patients and the short follow-up (6 months), based on the results obtained, it can be suggested that the techniques described may represent a viable alternative in the placement procedure. of implants in a single surgical act when there is residual bone height (AOR) less than 4 mm. However, these clinical case studies demonstrate the potential capacity of this new procedure where we osseodensify the scaffold made with Si-PRF within the sinus cavity and place implants in a single surgical act. More studies will be required to determine its statistical effectiveness in relation to the success rate and survival of implants over time.
Authors:
Hernández Suarez Argimiro, Álvarez Rogelio, Sastre Naranjo Javier, Freites Daniel, Cordero Francisco
References
Tatum H Jr (1986) Maxillary and sinus implant reconstructions. Dent Clin North Am 30(2): 207-229.
Boyne PJ, James RA (1980) Injerto del suelo del seno maxilar con médula autógena y hueso. J Oral Surg 38: 613-616.
Testori T, Weinstein RL, Taschieri S, Fabbro D (2012) Análisis de factores de riesgo después del aumento del seno maxilar: un estudio multicéntrico retrospectivo. Int J Oral Maxilofac Implants 27: 1170-1176.
Misch CE (1989) Bone classification, training keys to implant success. Dent Today 8(4): 39-44.
Huwais S, Mazor Z, Ioannou A, Gluckman H, Neiva R () A multi-center retrospective clinical analysis of 261 implants with up to 5 years follow-up placed via osseodensification transcrestal sinus augmentation. Int J Oral Maxillofac Implants 33(6): 1305-1311.
Summers R, Rosen RB, Summers PS, Mellado R (1994) The bone-added osteotome sinus floor elevation technique: Multicenter retrospective report of consecutively treated patients. Int J Oral Maxillofac Implants 15: 853-858.
Rosen PS, Summers R, Mellado JR, Salkin LM, Shanaman RH, Marks MH, et al. (1999) The bone-added osteotome sinus floor elevation technique: multicenter retrospective report of consecutively treated patients. Int J Oral Maxillofac Implants 14(6): 853-858.
Huwais S (2013) Fluted osteotome and surgical method for use. US Patent Application.
Hernández SA, Rizo GM, Suárez VD, Velazco G, Rodriguez GI, et al. (2021) Effectiveness of silicon platelet-rich fibrin and autologous bone on bone regeneration in rabbit calvarian defects: A radiological and histological study. Appl Sci (Basel) 11(9): 4074.
Elm V, Altman E, Egger M (2007) La declaracion de Fortalecimiento de los Informes de Estudios Observacionales en Epidemiologia (STROBE): Directrices para informar estudios observacionales. Lanceta 370: 1453-1457.
Zitzmann NU, Scharer P (1998) Comparacion de los abordajes crestal y lateral. Oral Surg Oral Med Oral Pathol Oral Radiol Endo 85: 8-17.
1эGui CL, Naval GL, De La Plata M, Sastre PM, Moreno C, et al. (2009) Análisis clínico de nuestra experiencia en más de 100 casos. Rev Esp Cir Oral Maxilofac 31: 223-230.
Herrero M, Picón M, Almeida F, Trujillo L, Núñez J, et al. (2011) 382 elevaciones de seno con técnica de ventana lateral y uso de biomaterial de relleno. Rev esp cir oral maxilofac 33(3):109-113.
Gill A, Rao P (2012) Primary stability: The password of implant integration. J Dent Implant 2(2): 103.
Misch CE (2007) Bone density: a key determinant for clinical success. Contemporary Implant Dentistry 3.
Elias C, Rocha F, Nascimento A, Coelho P (2012) Influence of implant shape, surfasse morphology, surgical technique and bone quality on the primary stability of dental implants. J Mec Behav Biomed Mat 16: 169-180.
Misch CE (2009) Implantología contemporánea. Elsevier Health Sciences.
Tatli U, Salimov F, Kurkcu M, Akoglan M, Kurtoglu C (2014) Does Cone beam computed tomography-derived bone density give predictable data about stability changes of immediate loaded implants?- a 1-year resonance frequency follow-up study. J Craniofac Surg 25(3): e293-e298.
Tumedei M, Piattelli A, Degidi M, Mangano C, Iezzi G (2020) Una evaluacion microscopica retrospectiva de 30 anos (1988-2018) de implantes dentales recuperados por diferentes causas: una revision narrativa. Int J Restaurador. 2020: e211-227.
Doi K, Kubo T, Makihara Y, Oue H, Morita K, et al. (2016) Aspectos de osteointegracion del implante colocado en la reconstruccion osea con hidroxiapatita de calcio porosa interconectada de tipo bloque recientemente desarrollada. J Appl Ciencia oral 24: 325-331.
Padhye AM (2020) NB Osseodensification - Una revision sistematica y analisis cualitativo de la literatura publicada. J Oral Biol Res Craniofacial 10: 375-1380.
Lahens B, Neiva R, Tovar N, Jimbo R, Cuppini M, et al. (2016) Bases biomecanicas e histologicas de la perforacion de osteodensificacion para la colocacion de implantes endoseos en hueso de baja densidad. Un estudio experimental en ovejas. J Mech Behav Biomed Mater 63: 56-65.
Elsayyad AA, Osman RB (2019) Osseodensification in implant dentistry: A critical review of the literature. Implant Dent 28(3):306-312.
Slete Fb, Olin P, Prasad H (2018) Comparacion histomorfometrica de 3 tecnicas de osteotomia. Implante Dent 27: 424-428.
Qi L, Pan S, Dangaria S, Gopinathan G, Kolokythas A, et al. (2013) Platalet-rich fibrin promotes periodontal regeneration and enhances alveolar bone augmentation. BioMed Res Int.
Sakka S, Baroudi K (2012) Factores asociados con el fracaso temprano y tardio de los implantes dentales. J Investig Clin Mella 3: 258-261.
Trisi P, Berardini M, Falco A, Podaliri Vulpiani M (2016) Validacion del valor del micromovimiento real como medida directa de la micromovilidad del implante despues de la cicatrizacion (estabilidad secundaria del implante). Un estudio histologico y biomecanico in vivo. Clin Implante oral Res 27: 1423-1430.
Trisi P, Perfecto G, Baldoni E, Berardi D, Colagiovanni M, et al. (2009) El micromovimiento del implante esta relacionado con el par de insercion maximo y la densidad osea. Clin Implante oral Res 20: 467-471.
Huwais S, Mazor Z, Gluckman H (2018) A Multicenter Retrospective Clinical Study with Up-to-5Year Follow-up Utilizing a Method that Enhances Bone Density and Allows for Transcrestal Sinus Augmentation Through Compaction Grafting. Int J Oral Maxillofac Implante 33(6): 1305-1311.

