Implantation for the rehabilitation of patients with neoplasms
Machine translation
Original article is written in RU language (link to read it) .
Chris Butterworth, BDS (Hons), MPhil, FDSRCS, FDS, RCS, Lead Orthopedic Prosthodontist at the Merseyside Head and Neck Cancer Centre, Liverpool, UK, shared his experience and clinical research findings on patient rehabilitation over the past 12 years years.
More detailed information in the online course Guided Regeneration and Navigated Implantation .
The patients were treated for malignant neoplasms in the upper jaw and midface. He outlined the challenges of managing this rare but noteworthy group of patients, the importance of using specialized instruments for malar cancer (with a unique intermediate cut, surface treated) and Co-Axis® implants (Southern Implants) for early prosthetic and orthopedic treatment. Over the past 12 years, he has collected the largest number of cases of patients with oncology who received zygomatic implants, and carefully analyzed the available literature on this important topic. He presented the results of his latest 10-year study.
Implants and oncology
Butterworth's study, "Immediate versus delayed local implant placement in patients with head and neck cancer—a 10-year study," is now in press. This work previously received an award for best clinical presentation at the 2017 Academy of Osseointegration meeting. He studied the survival and effectiveness of zygomatic and modified zygomatic implants placed in patients with head and neck cancer over a 10-year period. He also compared patients who received zygomatic implants during cancer treatment with those who received treatment at a later time.
Although 50% of all patients treated were smokers before surgery and 49% received radiation therapy before or immediately after implantation, the study results demonstrated a 12-month survival rate of 94% and a 5-year implant survival rate of 92%. %. His study also found that although there was a slight trend toward higher survival rates for implants placed directly compared with delayed placement, the difference was not statistically significant. There was also no statistically significant difference in survival between traditional zygomatic implants and oncology-modified implants placed in the maxillary defect.
Butterworth also described a modified and more aggressive approach to the rehabilitation of patients with maxillary excision and midfacial malignancies in his department. Moreover, the tendency has been to always strive to introduce (place) implants during cancer cell resection surgery and to reconstruct the implants as quickly as the patient’s recovery allows.
Zygomatic implants
Since 2016, Butterworth and his surgical colleagues have been combining zygomatic implant placement with microvascular soft tissue reconstruction for small maxillary excision defects to provide greater benefits to patients. He outlined and presented his new technique, the zygomatic implant-perforated (ZIP) flap, with several clinical examples.
The SIP flap technique, published in 2017 in the International Journal of Implant Dentistry 1, combines the benefits of surgical soft tissue reconstruction using zygomatic bone implants and oncologic implants placed during surgery to provide the patient with ongoing dental rehabilitation that is completed in for several weeks after surgery.
Figures 1 through 8 demonstrate the SIP flap technique for a patient with a large left maxillary tumor, followed by tumor resection and placement of oncologic-modified implants in the remaining left zygomatic bone, as well as removal of the remaining teeth and placement of conventional zygomatic implants on the contralateral side.
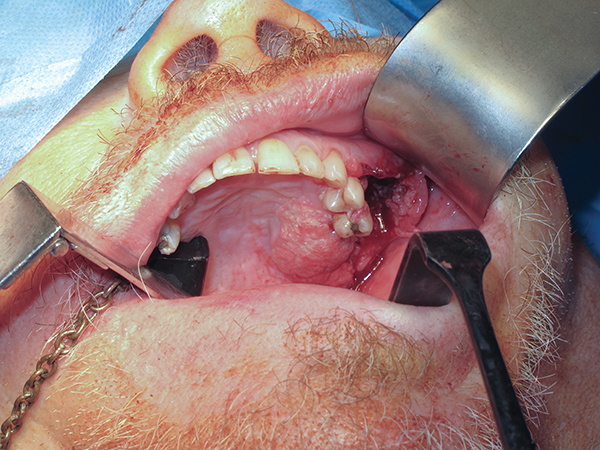
Rice. 1
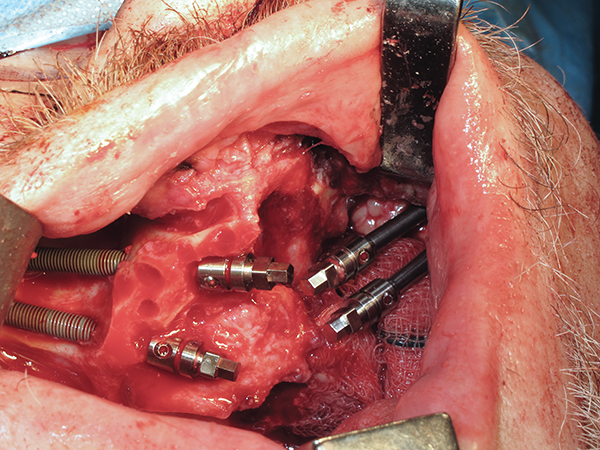
Fig.2
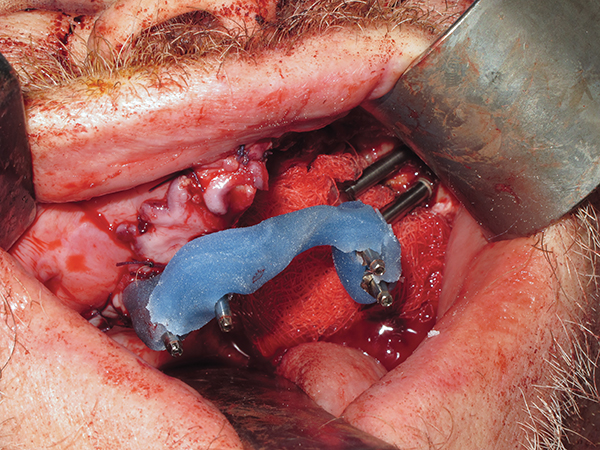
Fig.3
Multi-component abutments were placed, and impression-taking and occlusion recording techniques were used to help fabricate the temporary restoration. A large surgical defect between the oral and nasal cavities was covered with a radial free flap obtained from the forearm, which was placed and then perforated to allow access to the abutments on the oncology implants after surgery.
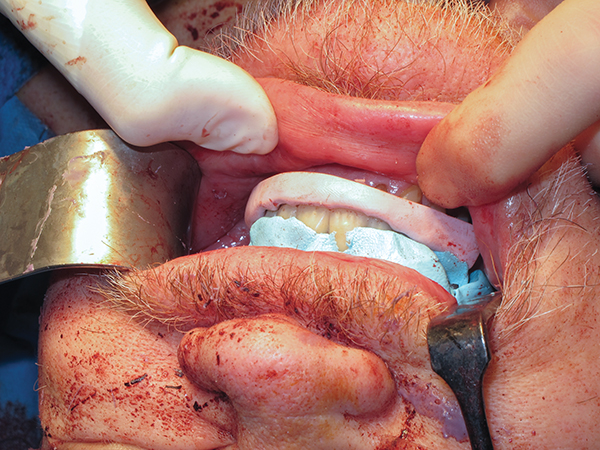
Fig.4
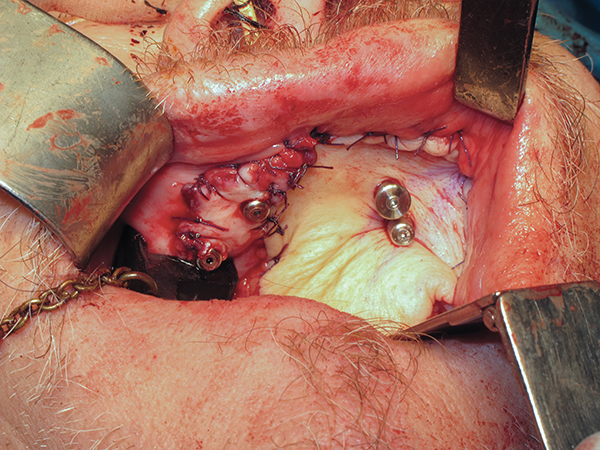
Fig.5

Fig.6

Fig.7
A temporary fixed denture was then placed 3-4 weeks after surgery. This can be done even when the patient requires postoperative adjuvant radiation therapy. With the defect surgically corrected and the teeth restored, ongoing orthopedic care was minimal and the patient's quality of life improved significantly.

Fig.8
Research into this new and exciting technique is ongoing, but the initial results presented by Butterworth on the first 12 patients treated in this way are extremely encouraging.
Learn more about this topic in our course Simultaneous implantation and immediate loading: surgical protocols .
http://www.aegisdentalnetwork.com/
