General characteristics of tooth sensitivity
Machine translation
Original article is written in RU language (link to read it) .
Dental sensitivity, or hyperesthesia of hard dental tissues, is a very common disease among the population around the globe.
About the prevention and treatment tactics of tooth sensitivity at the webinar Whitening under the supervision of a dentist: home whitening and remedies .
In the Republic of Belarus, dentin sensitivity occurs in up to 23.9% in different age groups; here only tooth sensitivity with non-carious lesions was taken into account. Another proof of the increased sensitivity of teeth among the population is the fact that in the search engine there are 1000 queries like “Treatment of tooth sensitivity with home remedies”, “Teeth pain when inhaling cold air”, “Which toothpaste to choose to make teeth less sensitive to cold water”. This once again proves that people want to solve their problems themselves, via the Internet, while not paying attention to the fact that it is necessary to eliminate the very reason causing the problem.

An interesting fact is that tooth sensitivity appears closer to 35-40 years. This is primarily due to changes in the periodontium – gum recession. Tooth sensitivity is also more common in women than in men.
Tooth sensitivity is a painful and rapid acute reaction of teeth to irritants. That is, this pain can be both cold and hot - thermal irritants, pain can be from mechanical influence - brushing teeth, from eating food (sour, spicy, sweet) - chemical irritants.
Etiology of tooth sensitivity
The etiology of tooth sensitivity is not fully understood. A single triggering factor or mechanism in the development of dental hypersensitivity has not been identified.
Tooth sensitivity is caused by a number of factors. Among them:
- cracks, chips of enamel;

- incorrect teeth brushing technique, horizontal movements, the appearance of wedge-shaped defects;

- high abrasiveness of the paste;
- hard brush, excessive force when brushing teeth;
- pathological abrasion of teeth;
- excessive consumption of acidic foods;

- treatment of teeth for inlays and crowns;
- teeth whitening;

- carious process;
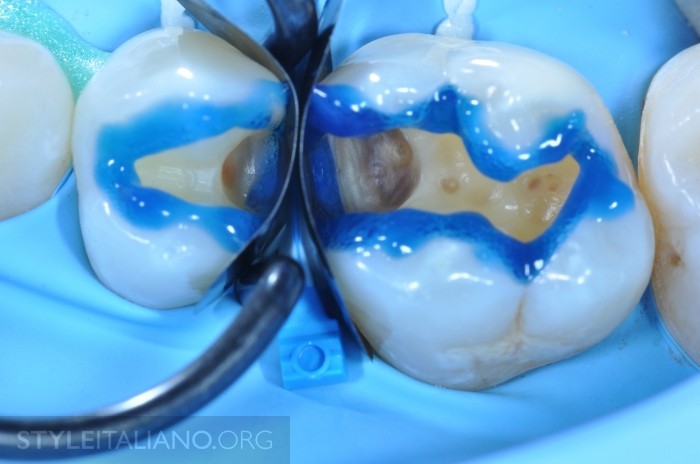
- incorrect technique for caries treatment - prolonged etching;
- improper rough technique for professional oral hygiene;

- gum recession (physiological);

- psychological disorders;
- metabolic disorders in the body (calcium-phosphorus metabolism disorders);
- psychosomatics, psychoneuroses;
- genetic disorders in the development of hard dental tissues;
- genetic predisposition;
- the presence of diseases of the body systems: endocrine disorders, diseases of the gastrointestinal tract.
There are many reasons for the occurrence of dental hyperesthesia. For example, home or improper professional whitening leads to disruption of ion exchange in dentin, calcium, phosphorus and other important elements are released from the enamel, all this leads to a violation of its structure and integrity. And bleaching itself is already a trigger for the development of calcium-phosphorus metabolism disorders. In addition, hormonal disorders also lead to metabolic disturbances. You don’t need to look far, the dentist himself, or rather his incorrect actions, can lead to disruption of calcium-phosphorus metabolism. Violation of the enamel etching technique when the etching time exceeds the permissible values.
An important point to clarify is gum recession. It is physiological, when the migration of the gums towards the apex of the root is associated only with age and age-related changes in the periodontium. After all, everything that was listed in the etiology of dental hyperesthesia will also be the cause of symptomatic gum recession. Therefore, you need to understand that very often gum recession occurs in parallel with increased tooth sensitivity.
Often tooth enamel is damaged when tissue is prepared for crowns and inlays. Also, excessive polishing of the enamel in the neck area of the teeth during professional hygiene will subsequently lead to dental hyperesthesia.
Theories of the occurrence of hypersensitivity of teeth
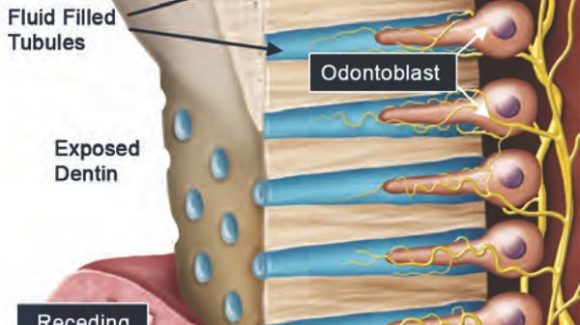
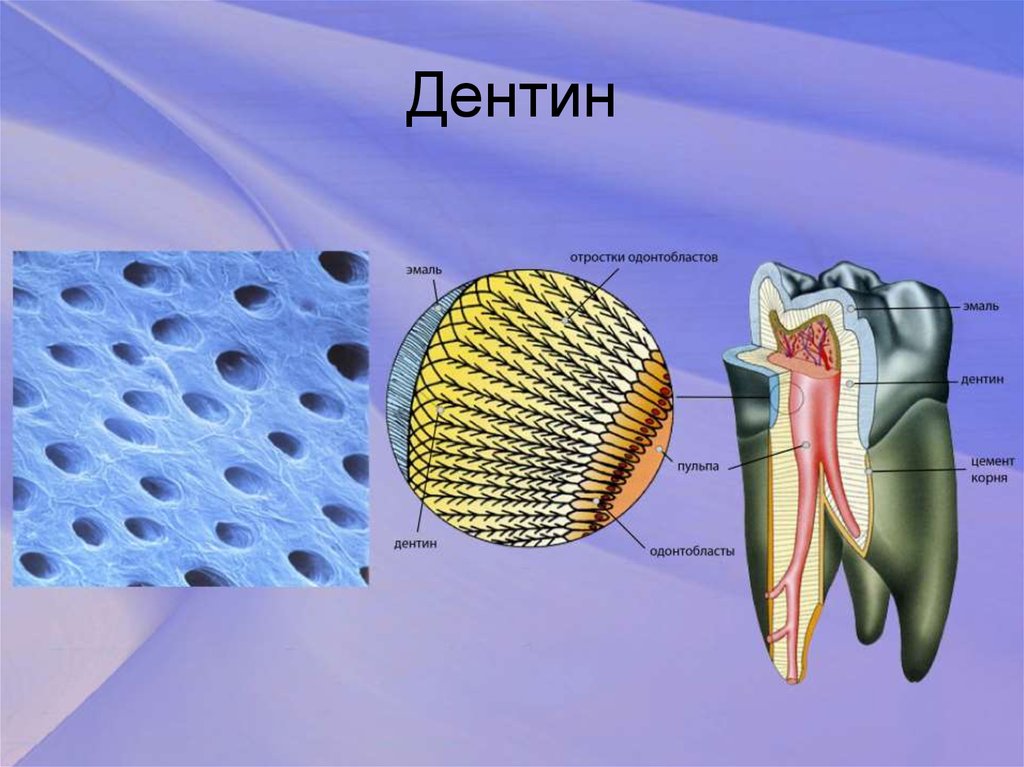
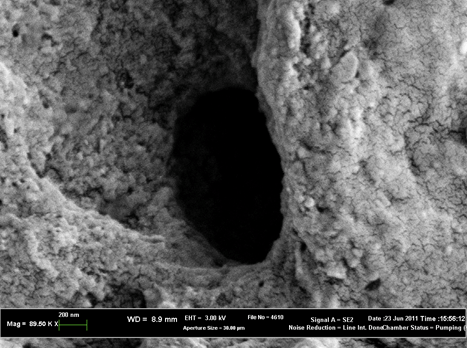
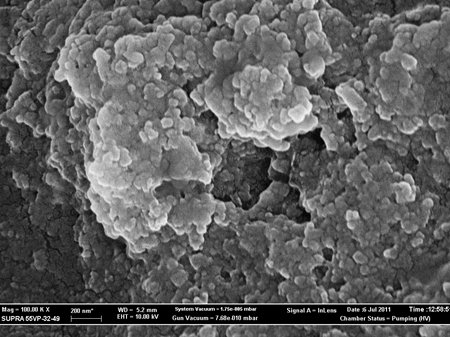
There are many reasons, many theories that have tried to explain the mechanism of development of increased sensitivity of teeth. But many theories were rejected because they were not clinically confirmed. At this stage of research into the mechanism of development of increased sensitivity of teeth, the hydrodynamic theory is very widespread. The hydrodynamic theory was proposed by A. Gyisi, but at the same time was sharply rejected. And only in 1980, the scientist M. Brannsuom, in the course of his research, proved that dentin consists of tubes that are S-shaped. The tubes contain dentinal fluid, which, when exposed to VARIOUS irritants, can move in any direction.
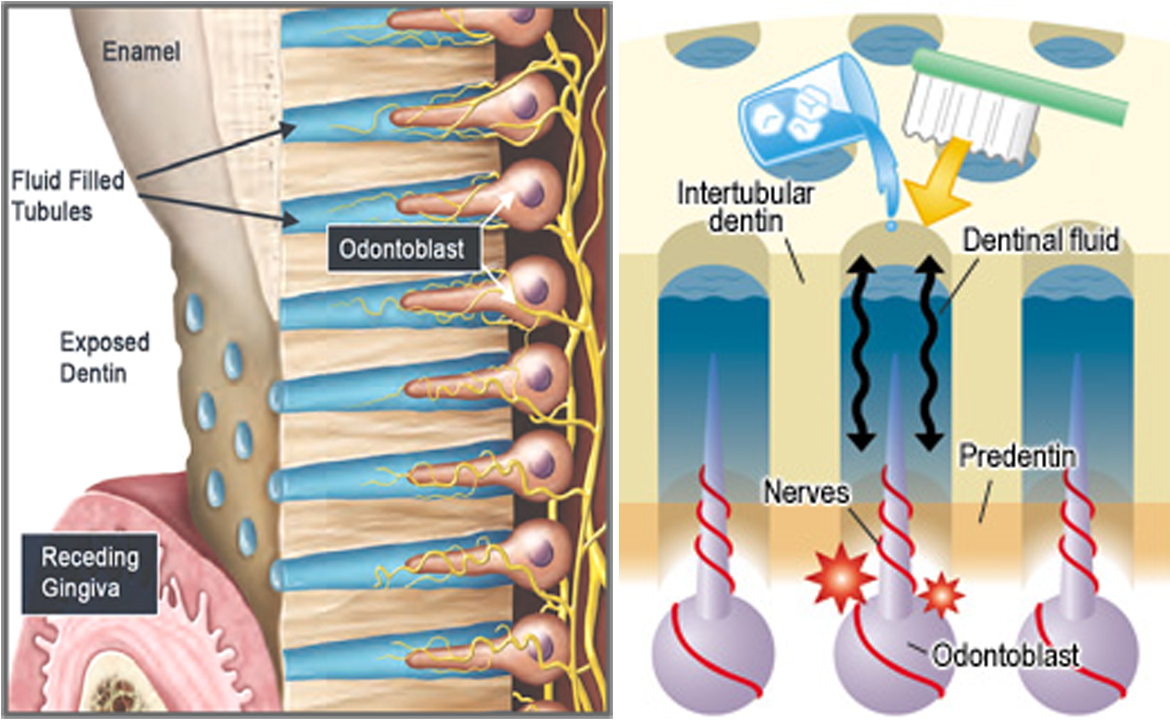
And it is this movement that leads to acute, fleeting pain in the tooth, since a change in pressure in the dentinal tubule on the receptor nerve ending occurs, and a nerve impulse occurs. Subsequently, this theory was confirmed by many scientists. And now it is considered as the most convincing evidence of the path of hypersensitivity of teeth.
Morphological picture of increased sensitivity of dentin
The morphological picture with increased sensitivity of dentin is characterized by the fact that many open dentinal tubules are observed in the dentin area. Some sources indicate that the number of open dentinal tubules is 8 times greater than closed ones, and that the opening width (diameter of the dentinal tubule) is 2 times greater compared to a regular dentinal tubule. In insensitive dentin, the dentinal tubules are filled with a mineralized substance, which has a clear structure, in contrast to dentin with increased sensitivity.
To summarize, we come to the conclusion that sensitivity (hyperesthesia) of teeth is a polyetiological disease. It is based on open dentinal tubules, the movement of fluid through which leads to a change in pressure on the nerve endings. Soreness occurs.
Classification of hyperesthesia (increased sensitivity) of teeth
The classification of hypersensitivity of teeth was proposed in 1988 by Yu.A. Fedorov. and Shtorin G.B.
A) According to the prevalence, dentin sensitivity is divided into:
- limited dentin sensitivity, which occurs in one maximum of 2 teeth;
- generalized dentin sensitivity, occurring in 2 or more teeth.
B) according to origin they are distinguished:
- dentin sensitivity associated with loss of hard tissue;
- dentin sensitivity not associated with loss of hard tissue.
B) according to the clinical course:
- 1st degree: teeth react only to a temperature stimulus - cold, EDI indicator is within 5 -8 mA;
- 2nd degree: teeth react to temperature and chemical stimuli, indicatively the EDI is below the norm of 3 -5 mA;
- 3rd degree: teeth react to any type of stimulus, EDI 1.5 - 3 mA.
Clinical manifestations of dental hyperesthesia
Clinical manifestations of dental hyperesthesia begin with minor mild pain when inhaling cold air or eating cold foods, both liquid and solid. Moreover, the more significant the process of increased sensitivity, the more intense and prolonged the pain. Often patients come in and can pinpoint exactly what the pain is, when and where. In patients with a generalized form and a subcompensated or decompensated course, plaque and caries in the stain stage are noted, since tooth brushing is difficult due to pain. In such patients, the face may change, it becomes puffy, speech is difficult - they try to minimally touch their cheeks to their teeth. In this case, increased salivation is noted.
The doctor needs to pay attention to:
- level of gum recession;
- the presence of non-carious lesions of hard dental tissues: erosion, wedge-shaped defects;
- abrasion of teeth;
- state of occlusion;
- presence of supercontacts;
- presence of cracks, chips of enamel;
During the survey, the dentist should clarify and even ask to demonstrate the technique of brushing teeth, ask about the oral hygiene products used, habits, profession and field of activity. Find out when the patient last visited the dentist and for what reason.
Treatment of tooth sensitivity
Treatment of hypersensitivity of teeth is a rather long process. Depending on the treatment method, the duration and effectiveness may be long-term, which aggravates the patient’s well-being, since the pain is not relieved. Therefore, it is important to choose the right treatment method for a patient with increased dental sensitivity, depending on the degree of dental hyperesthesia.

Treatment of teeth with hypersensitivity can be done at home or professionally. Home treatments include:
- chamomile solutions;
- oak bark solutions;
- pastes for sensitive teeth;
- mouth rinses;
- ointments based on sesame oil.
In general, this list can be continued with many points. And often patients, coming back from unbearable pain, can talk about some of them. But all this does not affect the dentinal fluid, will not change the composition of the micro- and macroelements of enamel and dentin, but only veils the pain.
Professional treatment for dental hypersensitivity is varied. It all depends on the material base and the degree of sensitivity of the teeth.
The first method of treating dental hyperesthesia is fluoridation. The bottom line is that drugs are used whose action is aimed at clogging the dentinal tubules. They cover and seal the dentinal tubules. Active substances - calcium, phosphorus, fluorine, strontium - bind to the proteins of hard tissues, precipitate and close the dentinal tubules. The movement of dentinal fluid stops, which means pain is eliminated. The technique involves the use of professional dental gels and varnishes, as well as the daily home use of fluoride-containing toothpastes. This way achieves deep fluoridation of hard dental tissues. Fluoride ions interact with calcium ions to form an insoluble compound that precipitates in the dentinal tubules, blocking the flow of dentinal fluid. Strontium-based preparations not only block dentinal tubules by depositing in them. But by contacting the protein matrix of hard tissues, they trigger the formation of tertiary (replacement) dentin. Strontium-based preparations replace enamel crystals with strontium-hydroxyapatite crystals, which increases the enamel's resistance to irritants.


The 2nd method of treating dental hyperesthesia is aimed at reducing the sensitivity of nerve endings and desensitizing them. This process is long. The results of treatment are very long-term.

The essence of the method is that potassium enters the dentinal tubules and penetrates through them into the nerve endings. With a sufficient accumulation of potassium ions, they create a supposedly protective shell, preventing the penetration of pain impulses. In dentistry, special professional pastes with potassium are used to fill mouthguards for patients. And the patient sits for a certain time with such a mouthguard in a chair, ensuring a massive supply of potassium to the nerve endings.

For treatment at home, special pastes called desensitizers are used to consolidate the effect. These are pastes with a high content of essential microelements, such as calcium, phosphorus, fluorine. These are alkali-based pastes, which, when they enter the dentinal tubules, lead to dehydration of the dentinal tubules. Desensitizers are used no more than three times a year.
Good treatment results were obtained using electrophoresis with a 10% calcium gluconate solution. This type of treatment is used in courses of 10-12 procedures for 10-15 minutes.
The listed methods for treating dental hypersensitivity will be effective only if the causes are eliminated: caries is cured, psychosomatics are normalized, the correct technique for brushing teeth is achieved, remedies are selected, and the general condition of the body is normalized.
Learn more about the diagnosis and treatment tactics of dental hypersensitivity at the webinar Dental erosion as one of the factors in the development of pathological abrasion .
