Eliminating crowded teeth
Machine translation
Original article is written in RU language (link to read it) .
We carry out an initial risk assessment and determine the criteria by which we can achieve its reduction. Very often we see excellent work and carefully developed treatment methods that did not reduce the risk, but simply replaced it with another. Careful analysis of the risks and benefits of treatment methods allows the clinician to avoid this.
Learn more about the method of treating crowded teeth in the webinar Distalization of mandibular molars: treatment of complex cases of crowding and mesial occlusion without tooth extraction .
In our case, the patient chooses not an expensive, complex and time-consuming treatment, but a well-developed restorative and orthodontic treatment plan, which leads to a satisfactory and stable result. Restoring the correct position of the incisors to achieve good esthetics is quite a difficult job. The structural features of the dental system, etiology, risk factors and wishes of the patient - all this should be carefully studied, as it affects the prognosis of further treatment, which often requires the use of two or more dental methods.
Crowded teeth
A healthy, 63-year-old man requested to improve his smile, correct crowding of the lower teeth in the anterior region, uneven edges of the upper anterior teeth, and their color (photos 1, 2).

Rice. 1

Rice. 2
The medical history was unremarkable other than a successful right hip total replacement surgery performed 9 months previously. After which he was prescribed antibiotics to prevent dental diseases. A review of the dental history revealed that the patient had a moderate number of treated teeth, and he also reported some problems that concerned him. Chips on the teeth were noted (photos 3, 4). The upper right premolars were removed many years ago, he could not remember the reason. He did not notice any problems with chewing or any other dental diseases.

Fig.3

Fig.4
Diagnosis, risk assessment and prognosis
Periodontium: the study showed a probing depth of 2-4 mm, the presence of bleeding. The radiograph showed a horizontal loss of bone tissue with a depth of 2-3 mm. Teeth 3, 6, 11 have recession. In addition, in teeth 3, 11 there is abrasion in the cervical area.
Diagnosis: early periodontitis.
Risk: low.
Prognosis: good.
Biomechanical characteristics: teeth 2, 3, 11, 13 and 31 have questionable restorations. In teeth 2, 3, 10, 12, 13 and 15 there are intracanal restorations. No active caries was detected, but the posterior teeth had questionable restorations.
Risk: high.
Prognosis: satisfactory.
Functional characteristics: the patient did not complain of difficulty chewing or symptoms of temporomandibular joint dysfunction. There is moderate enamel wear on the occlusal surfaces, chipping on the upper anterior teeth and moderate wear on the lower anterior teeth. Because there was no evidence of occlusal trauma or temporomandibular joint disease, we concluded that the current dental problems were caused by preexisting occlusal dysfunction or crowding (Figure 5).

Rice. 5
Risk: low.
Prognosis: good.
Maxillofacial Characteristics: Moderate protrusion of the anterior teeth was noted when the patient smiled (Figure 6).

Photo 6
Wear on the upper incisors has negatively impacted the smile line. The maxillary midline was displaced 2–3 mm to the right due to early tooth loss 4, 5; however, its incorrect position did not bother the patient. The condition of the gums on the upper jaw was satisfactory, with the exception of teeth 6, 11 (recession of 1 mm and 2 mm, respectively). But when smiling, all this was not noticeable, so it was not a problem for either the patient or the clinician.
Risk: moderate.
Prognosis: good.
Treatment Goals
Treatment goals were determined by the patient's needs and an objective risk assessment of all existing dental diseases.
They are as follows:
1) cure, stabilize and maintain periodontal tissues through conservative treatment, systemic antibiotic therapy;
2) improve the appearance of the smile by increasing the size of the upper teeth and increasing the vertical dimension of occlusion (VRO), using ceramic restorations after orthodontic treatment;
3) minimize biomechanical risks by replacing bad restorations and improving the bite, doing this simultaneously on both sides.
Treatment plan
Thanks to modern technology, the patient was given several options for possible correction, including orthognathic surgery. As a result, we chose a treatment that included 4 stages and took from 10 to 12 months. The patient agreed to the proposed treatment.
Scaling and root planning, systemic use of antibiotics (amoxicillin 500 mg for 8 days; metronidazole 500 mg for 8 days). Then tooth 24 will be removed. Due to the vestibular location of tooth 24 and the lingual location of teeth 23-25, it is only possible to achieve the result we need by removing tooth 24.
Limited orthodontic treatment will be required to straighten all lower anterior teeth. Severe crowding in this area precluded consideration of porcelain veneers for two reasons. First, teeth 23 and 25 would be overloaded, so they would have to be reduced to the starting point of the root canals before using veneers. Secondly, tooth 24 had been displaced from the lower arch and would have required significant arch expansion and would have caused a major shift in biomechanical risk.
For the lateral teeth of the upper jaw, we chose restorations that completely covered the tooth, and improved the proportions of the anterior teeth by increasing the VRO and adding ceramic inserts to the incisal edge.
Stages of treatment
Stage 1 - periodontal therapy
Periodontal therapy. Scaling and root planning using systemic antibiotics, which were mentioned above.
Stage 2 - tooth extraction
Tooth extraction and orthodontic treatment.
Tooth 24 was removed and orthodontic treatment began (photo 7).
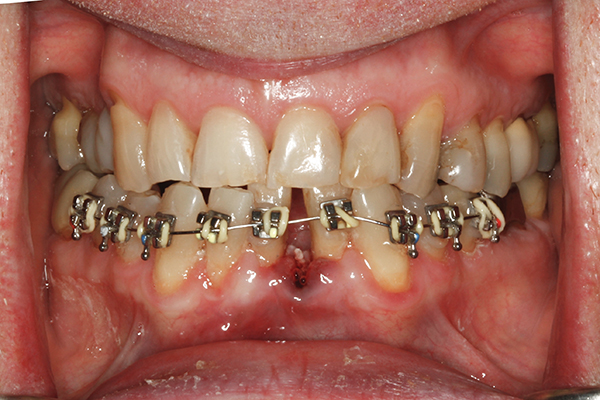
Photo 7
To correct crowding of the lower anterior teeth, there were several options: extraction of teeth 23 to 26 and a bridge, extraction of teeth 23 to 26 and placement of implants, or extraction of tooth 24. The patient was offered all of these options, but he was not willing to continue orthodontic treatment or resort to orthognathic surgery, which is why we chose this treatment method (photo 8).

Photo 8
Stage 3 - wax reproduction
Design of diagnostic wax-up for the upper jaw. A diagnostic wax-up was prepared using a Kois Dentofacial Analyzer and mounted in a Panadent articulator (panadent.com). The required smile line was achieved (photo 10).

Photo 9
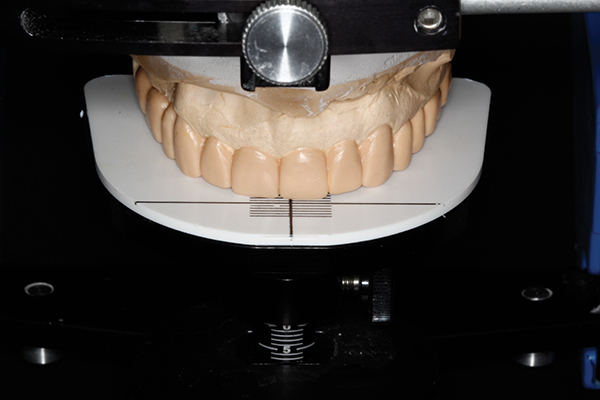
Photo 10
Stage 4
After orthodontic treatment, which lasted 6 months, we were able to achieve the required VRO in the upper jaw, with the exception of tooth 1. The incorrect crossbite was corrected through restorations (photo 11). The anterior teeth were prepared for subsequent cementation of porcelain restorations (e.max®). The incisal edge was reduced by 2 mm, resulting in improved esthetics.

Photo 11
The risk associated with the presence of questionable restorations on the posterior teeth was reduced through the use of crowns (photos 12, 13). They were prepared for subsequent cementation of e.max® crowns (Ivoclar Vivadent, ivoclarvivadent.com).

Photo 12
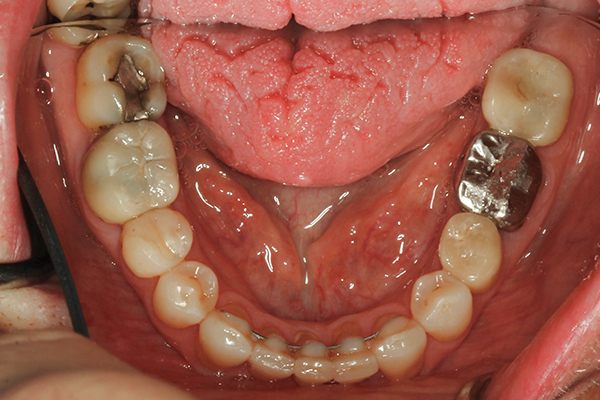
Photo 13
The treatment was completed in a timely manner, taking into account all the patient's wishes (photo 14). Active orthodontic treatment continued for 5 months, one month was required to maintain the result before restoration work.

Photo 14
Discussion
Taking into account the initial risk assessment, the doctor established criteria through which risk reduction can be achieved. Very often we see well-done work and carefully designed treatments that did not reduce the risk, but simply replaced it with another. This can be avoided, but only through careful analysis of the risks and benefits of treatment. Understanding and anticipating most, if not all, difficulties and having a consistent and well-thought-out treatment plan allows the dentist to avoid problems that could lead to undesirable consequences.
conclusions
Correction of the location of incisors standing “joint to joint” occurs quite often. If patients strongly disagree with the optimal comprehensive orthodontic treatment and surgical intervention, then it is necessary to plan the use of restorations in both the upper and lower jaws. This article attempts to present an alternative to comprehensive orthodontics by applying limited orthodontic treatment to the mandible, thereby reducing the duration and cost of treatment. The patient was monitored for more than 2 years. The restorations, functions, and periodontal condition are in a stable condition, the patient is satisfied with the result (photo 15).
If you are interested in the topic of this article, pay attention to the webinar Protocols for treating crowded teeth with aligners .
http://www.aegisdentalwork.com/
