Dental trauma. Diagnosis and treatment
Machine translation
Original article is written in RU language (link to read it) .
Dental trauma is one of the most common problems with which a person goes to the dentist. It's logical. After all, we all grew up, learned to crawl and walk, and explored the world. Having grown up, of course, we play sports and try to lead an active lifestyle.
Read more about dental injuries at the webinar Injuries to the teeth and the supporting apparatus of the tooth - various types of classifications, an overview of all possible injuries in the maxillofacial area .
The problem of diagnosing dental trauma, treating dental trauma and preventing dental trauma remains relevant both among dentists and among the population.
This article will discuss the following types of injuries:
- tooth root fracture;
- tooth dislocation and its types.
Before revealing the topic, I remembered some elements of the classification of dental trauma.
Classification of dental trauma
According to the International Classification of Dental Diseases based on ICD-10 (WHO, Geneva, 1997), the following dental injuries are distinguished:
- S02.5 Tooth fracture.
- S02.50 Fracture of tooth enamel only;
- S02.51 Crown fracture without pulp damage;
- S02.52 Fracture of the tooth crown with damage to the pulp;
- S03.53 Tooth root fracture;
- S02.54 Fracture of the crown and root of the tooth;
- S02.57 Multiple fractures of teeth;
- S02.59 Unspecified tooth fracture;
- S03.2 Tooth dislocation;
- S03.20 Tooth luxation;
- S03.21 Tooth intrusion or tooth extrusion;
- S03.22 Tooth dislocation (disarticulation).
Elements of classification of tooth trauma according to N. M. Chuprynina (Moscow, 1993)
Tooth luxation:
- Incomplete tooth dislocation;
- Complete tooth dislocation;
- Impacted tooth dislocation.
Tooth root fracture:
- Longitudinal fracture of the tooth root;
- Transverse fracture of the tooth root;
- Oblique fracture of the tooth root;
- Displaced tooth root fracture;
- Fracture of the tooth root without displacement.
Tooth root fracture
Symptoms of tooth root fracture
Symptoms of a tooth root fracture are as follows:
- pain, which is most often characterized as aching;
- pain when biting on the causative tooth;
- pain when touching the alveolar process;
- tooth mobility;
- change in tooth position;
- possible bleeding from a damaged tooth;
- appearance of fragment elements on the surface;
- when trying to open your mouth, when trying to talk, the pain may intensify;

Most often, this symptomatology of a tooth root fracture accompanies an acute injury. For people with a chronic tooth root fracture, aching pain is more typical, aggravated by chewing or percussion; most often these teeth have an existing dental problem.
Causes of tooth root fracture
The reasons for a tooth root fracture are quite varied and commonplace:
- Aggressive tooth extraction;
- Incorrect tooth extraction technique;
- Poor quality root canal treatment;
- Poor-quality orthopedic treatment (for example, installation of a cast stump insert);
- Deep caries extending to the cementum and dentin of the tooth root. In this case, any touch to the tooth can lead to its fracture;
- Dental injuries: sports, household, automobile;
- Disturbances in the development of hard dental tissues;
Diagnosis of tooth root fracture
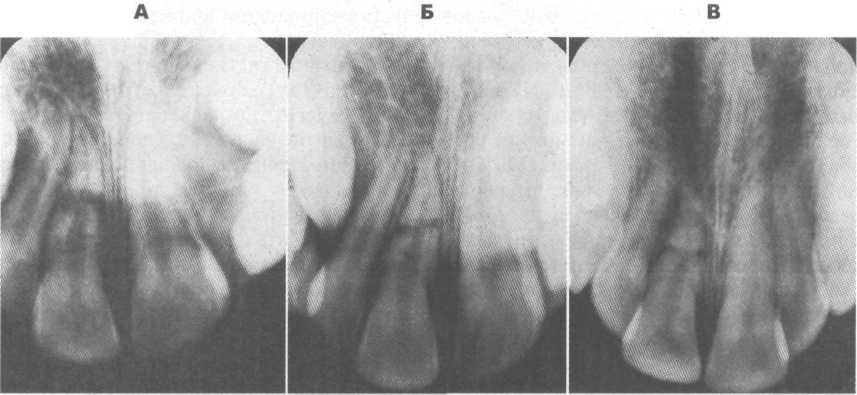
Diagnosis of a tooth root fracture is quite difficult, although it would seem that all the clinical signs are obvious. However, no. In the absence of an x-ray, a tooth root fracture can be confused with a tooth dislocation - aching pain, there may be slight mobility. During a visual examination, you may not notice any clinical signs; for example, if the root of a tooth is fractured, the crown of the tooth will not always turn pink. Staining will be observed when the apical third of the root is fractured - this is associated with intrapulpal hemorrhage. And even here the statistical figures are not unambiguous, and changes in the color of the tooth crown due to a fracture of the tooth root are recorded on average in 30% of patients.
Even such basic diagnostic methods as palpation along the transitional fold, palpation along the alveolar process, vertical and horizontal percussion will not fully reveal the entire clinical picture. In general, percussion during a tooth root fracture will be painful both at the time of injury and for three weeks after its diagnosis.
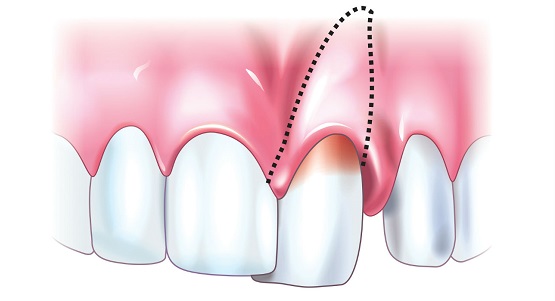
Palpation of the alveolar process should be carried out whenever there is a suspicion of a tooth root fracture, because these injuries are often combined. Also, with palpation, you can guess where the fracture line is and whether the fragment is displaced. To do this, place the finger of one hand on the gum on the vestibular side, and with the other hand rock the crown of the tooth with a root fracture. The closer the fracture line is to the edge of the crown, the greater the trajectory of the crown will be. And the more the fragment is displaced, the mobility and trajectory of the crown will also be greater.
For a high-quality diagnosis of a tooth crown fracture, or more precisely to check the viability of the pulp, dentists use electroodontometry, where the condition of the pulp is determined by indicators in microamperes. It must be remembered that a tooth root fracture is not always accompanied by pulp necrosis.
The main diagnostic method is x-ray. And it is best to do this in three planes at three different angles (45, 90, 110 degrees) or, if possible, do a CBCT scan. It must be remembered that radiographs taken in the first hours after a tooth root fracture are not always informative due to the tight fit of the fragments. Only after a while can the fragments disperse due to the formation of a blood clot. Therefore, it is recommended to take another x-ray. In the picture you can appreciate:
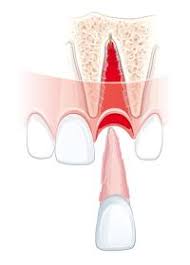
Divergence of fragments:
- complete fracture (with complete divergence of fragments);
- incomplete fracture (fragments are intact, not separated);
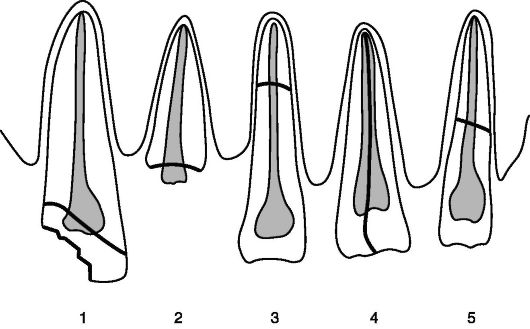
Fracture line direction:
- transverse;
- oblique;
- longitudinal;
Fracture line level:
- in the cervical part of the tooth;
- in the middle part of the tooth;
- in the apical part of the tooth;
- “Intraosseous” fractures - inside the alveolar bone with damage to the integrity of the periodontium;
- Fractures are “extraosseous” - outside the alveolar bone without damage to the periodontium.

From the image you can determine the direction of displacement of the fragment. So, if a fragment of a tooth root has shifted either vestibularly or orally, then this is accompanied by a decrease in the size of the crown of the causative tooth; When a fragment of a tooth root is displaced in the occlusal direction, it will be noticeable on the radiograph that the crown of the damaged tooth and the adjacent healthy tooth will be at different levels.
There is also such a thing as a comminuted fracture. This is a fracture in which there are more than three fragments, separated from each other by fracture lines of different directions (that is, a combination of several directions). And most often, such comminuted fractures are extremely difficult to diagnose and can only be done after a long period of time, when the gap is filled with connective tissue.
TREATMENT OF TOOTH ROOT FRACTURE
For correct and competent treatment of a tooth root fracture, it is necessary to find out whether or not there is a connection with the oral cavity, how and where the fracture line runs, and whether the tooth is of functional value. But before answering these questions, it is necessary to understand 4 possible mechanisms of healing of a tooth root fracture line.
Mechanisms of tooth root healing
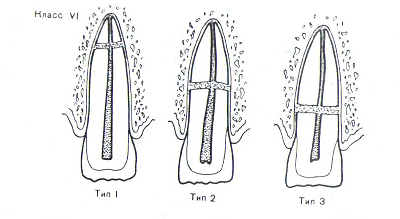
Among all the mechanisms of tooth root healing, mineralized healing is considered the most favorable, that is, dentin and cement grow into the fracture line (this healing mechanism is typical for well-immobilized teeth and without infection).
The so-called “connective tissue fusion” is possible - when the connective tissue bundle ruptures and the blood supply is restored, the connective tissue grows in the fracture line (that is, the periodontal ligament) with the formation of a new apical foramen. The periodontal ligament grows into the fracture gap, thereby forming a periodontal gap around each fragment.
The third option for healing the fracture line is combined healing, that is, mineralized healing together with connective tissue. Such fusion will occur only in the case of growth of the alveolar processes and with a large distance between the fracture fragments.
And the most unfavorable thing with the possible formation of fistula tracts is healing “without fusion” with the germination of granulation tissue. This type of fusion is typical for teeth without timely endodontic treatment.
The main goal in the treatment of a tooth root fracture is to create an anastomosis to form a mineralized connection between the fragments. Vital pulp will improve the prognosis of treatment. Therefore, when treating a tooth root fracture, it is necessary to reduce the distance between the fragments as early as possible and ensure reliable immobilization of the teeth.
Treatment of a tooth root fracture that does not communicate with the oral cavity
When treating a fracture of a tooth root that does not communicate with the oral cavity, when confirming the viability of the pulp, it is necessary to reposition the fragments and immobilize the teeth, followed by monitoring on an x-ray. The duration of splinting can be up to 3 months. In this case, the patient is recommended to eat only soft foods. Every month, the splint is checked and a photo is taken to ensure proper fusion of the fragments, and tests are done for pulp vitality.
Treatment of a fractured tooth root communicating with the oral cavity
Treatment of a fracture of a tooth root communicating with the oral cavity depends primarily on the passage of the fracture line, the volume of damaged tissue, and the length and anatomy of the tooth root. In case of a fracture involving more than 2/3 of the root length, the tooth is removed.
Often, when a tooth root is fractured, the pulp is already necrotic. And then the dentist must determine the indications for filling the canals with either gutta-percha or calcium hydroxide.
Indications for canal filling with gutta-percha in case of tooth root fracture
Indications for filling canals with gutta-percha in case of a tooth root fracture are as follows:
- on the radiograph there are no areas of destruction in the area of the lower third of the tooth root;
- when touching the tooth pulp with a paper point - bleeding (confirmation of the vitality of the tooth pulp);
- there is no distance between the fragments, or the distance is insignificant;
- The root canal at the fracture line is not wide.
Indications for canal filling with calcium hydroxide in case of tooth root fracture
Indications for canal filling with calcium hydroxide in case of a tooth root fracture may be:
- wide root canal (as a risk of gutta-percha removal);
- the presence of periapical changes on the radiograph;
- internal/external resorption of root fragments;
- Viable pulp (paper point bleeding test).
When observing changes on an x-ray, if the course is favorable, after six months a dentinal bridge may form, after which the canals can be filled with gutta-percha.
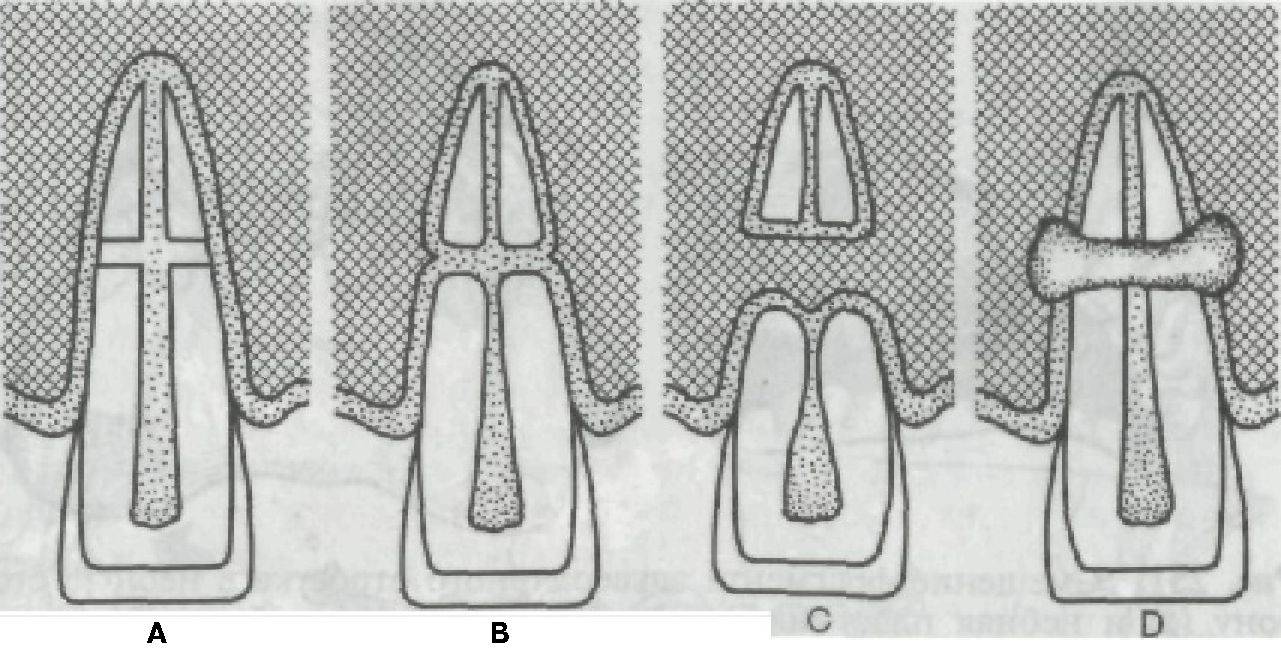
Tooth luxation
Tooth luxation is a tooth injury with damage to the supporting apparatus. To put it more simply, the tooth is displaced and the periodontal ligaments are damaged. A tooth dislocation can be:
- incomplete tooth dislocation;
- impacted dislocation (intrusive);
- complete tooth dislocation.
Tooth dislocation can be caused by various factors, for example:
- hit;
- injury;
- dislocation of a nearby tooth due to aggressive tooth extraction, or due to incorrect selection and application of forceps for tooth extraction;
- biting into hard food;
- bad habits (opening bottle caps with teeth; biting hard wire).
Symptoms of tooth dislocation
Symptoms of incomplete tooth luxation
Symptoms of incomplete tooth dislocation are pain when biting on a tooth, pain when chewing food, bleeding of the causative tooth, and its displacement.
Symptoms of impacted tooth dislocation
Symptoms of an impacted (intrusive) tooth dislocation will be shortening or complete disappearance of the visible part of the tooth crown, the tooth is motionless, percussion is slightly painful. It must be remembered that with impacted dislocation of the central incisors on the upper jaw, the teeth may
penetrate the nasal cavity.

Symptoms of complete tooth dislocation
The patient can bring the tooth in his palm.
Treatment of tooth luxation
Treatment of incomplete tooth luxation
Treatment for incomplete tooth dislocation involves repositioning the tooth and splinting it. Reposition must be performed no later than 2 hours from the moment of injury, otherwise the risk of developing pulp necrosis increases.
Treatment of impacted (intrusive) tooth dislocation
Treatment of impacted (intrusive) tooth dislocation consists of orthodontic reposition for 3-4 weeks.
Treatment of complete tooth dislocation
Treatment for complete tooth avulsion consists of replantation, splinting and endodontic treatment.
Only those that have been outside the mouth for no more than two hours are suitable for replantation of natural teeth. Drying of tooth cells leads to early resorption. But if such a nuisance does occur, patients should place the tooth either in a glass of milk, or hold it behind the cheek or under the tongue.
About the features of preparing an injured tooth at webinar 1.3 and 2.3 - tooth restoration due to injury .
