Dental implant planning
Machine translation
Original article is written in RU language (link to read it) .
Having carried out all the necessary examinations of the patient and analyzed the results obtained, the surgeon, orthopedist and dental technician can begin planning treatment, which will consist of several stages: surgical and orthopedic.
At the stage of planning dental implantation, the most important task is to choose the most rational type of prosthetics, select the optimal number of implants, certain types of them, and settle on a specific implantation technique.
Learn more about how to avoid the development of peri-implantitis in the online course Implantation without peri-implantitis .
The condition of the teeth preserved in the oral cavity determines the method of prosthetics; in addition, the choice is influenced by anatomical prerequisites, on which the possibility of using certain models of implants depends. It is imperative to take into account the patient’s financial capabilities and wishes.
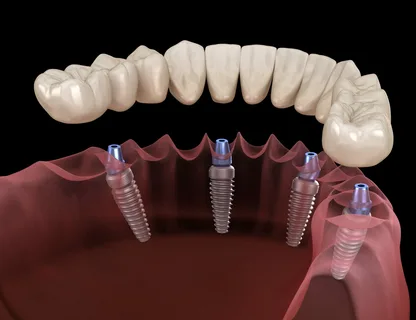
Figure 1. Dental implantation.
Together with implants, fixed bridge structures, conditionally removable and beam superstructures are used, which are necessary to ensure the fixation of complete removable dentures.
The type of implant is selected based on an analysis of the volume of remaining bone tissue, the shape of the edentia, the architectonics of the bone and the design of the prosthesis. The main criterion for the success of dental implantation is sufficient bone volume. After installation, the implant must be completely surrounded by a dense mass of vital bone structure, and the thickness of the bone tissue in the thinnest area cannot be less than 1.0-1.5 mm.
Two-stage cylindrical and screw implants with a cross-sectional size of 3.3 and 4.0 mm are installed when the thickness of the alveolar process is over 5.0-6.0 mm, respectively; single-stage screw implants with a cross-sectional size of 2.8-3.0 mm are installed when the thickness of the alveolar bone is process over 4 mm, plate structures - with a thickness of 3 mm.

Figure 2. Single implants.
The choice of the number of implants is influenced by the following factors:
type of edentia,
method of prosthetics,
length of the defect.
In accordance with the Muratori principle, against the background of secondary adentia, if the prosthesis is located exclusively on implants, the number of the latter should correspond to the number of extracted teeth. If the prosthesis rests on teeth in addition to implants, then you can limit yourself to installing a minimum number of implants, which will be determined by the extent of the defect. In the case of complete edentia, it is recommended to use at least six implants if fixed prosthetics are planned, two to four if removable.
When choosing the number of implants to install, you should follow the rule: the gap between adjacent implants, as well as between implants and remaining teeth, is 3 mm.
The implant design is also selected based on the type of bone architecture of the patient. Bone architecture is a term that denotes the proportional ratio of compact and spongy bone tissue, while the density of the trabeculae of the spongy layer is additionally taken into account. The number of structural elements located per unit volume of the bone structure determines the degree of bone density and the likelihood of osseointegration.

Figure 3. The phenomenon of osteoporosis in bone tissue.
Taking into account the above, the ratio of the compact layer and the spongy layer in different parts of the jaw and in different jaws is different. The approximate ratio of compact and spongy substance in the lower jaw is 1:1, in the upper jaw – 1:3.
The well-known classification by Lekholm and Zarb is based on the key phenotypes of bone tissue architecture; it includes the following types of bone:
Class 1 is bone tissue, which is represented predominantly by a homogeneous compact substance (ratio 2:1);
Class 2 - this dense compact substance surrounds a highly organized spongy substance (1:1 ratio);
Class 3 is a thin compact plate surrounding a highly organized spongy layer (ratio 1:3);
Class 4 is a thinned compact plate surrounding a spongy layer, characterized by a low density of the trabecular network (1:4 or more).
The bone architecture is assessed based on computed tomography data; it determines primary stability during dental implantation and subsequently functional load.
With types I and II of architectonics, good density of the compact substance, there is a possibility of thermal injury during the preparation of the bone bed, however, in such a clinic, any types of implants can be used.
In types III and IV architectonics, when signs of regional osteoporosis are determined, the use of implants, the design of which is equipped with a large surface area, is indicated.

Figure 4. All on 4 implantation.
The type of edentia has a direct impact on the choice of implant type. Screw implants have proven themselves well for the restoration of single defects in the dental arch. For end and included defects, any types of intraosseous implants are used.
When choosing an implant, it is important to consider the design of the future prosthesis. If a bridge is to be made, the remaining teeth are included as a support; in this case, implants of any type can be selected. There is a rule regulating the use of plate implants for end defects; according to it, at least two abutment teeth must be included in the bridge prosthesis. If this rule is not followed, functional overload that occurs in the long term will lead to undesirable complications (implant mobility, peri-implantitis, implant fracture).
Conditionally removable denture structures are used if only implants are used as support; there is no need to prepare the teeth adjacent to the defect. In this case, plate implants cannot be used. With one exception: plate implants act as additional support, and the prosthetic design, in addition to them, includes cylindrical and screw implants.
Plate implants are contraindicated when using beam superstructures; here it is advisable to install screw or cylindrical implants.
Indications and contraindications for dental implantation
The following indications for implantation exist:
terminal bilateral and unilateral defects on the jaw;
included defects;
complete edentia on one of the jaws;
single defect of the dentition.
Contraindications for implantation can be divided into local and general.

Figure 5. All on 6 implantation.
General contraindications
decompensated stages of somatic diseases;
diseases of the endocrine system;
systemic lesions of the musculoskeletal and hematopoietic systems;
mental illness;
allergies to drugs and materials used in dentistry;
smoking;
bruxism.
Local contraindications
significant atrophy of the alveolar bone, undercutting of the lower jaw is so pronounced that it does not allow the implant to be installed and securely fixed;
the structure of the bone substance is significantly impaired;
chronic inflammation or neoplasms in the area of the planned intervention;
significant reduction in bite height due to pathological abrasion;
acquired or congenital deformities of the jaws, including dentoalveolar lengthening, which is accompanied by a decrease in the interalveolar distance to 5 mm or less;
diseases of the mucous membrane that do not allow achieving stable remission:
TMJ lesions;
The level of personal hygiene is extremely unsatisfactory.
During dental implantation, local contraindications are identified during the examination, basic and additional examination methods, which assess the condition of the teeth preserved in the oral cavity, the size of the dental arch defect, the thickness of the alveolar ridge, the condition of the mucosa, in the defect area - the interalveolar height, the depth of the vestibule, the presence of pathology from the side of the temporomandibular joint, the state of the bite.
An X-ray examination is mandatory, at least orthopantomography, but computed tomography is more informative; these studies help assess the condition of the remaining teeth and the height of the alveolar ridge. These radiographs help to clarify the distance from the top of the alveolar process to the mandibular canal or the bottom of the maxillary sinus. Orthopantomography distorts real values vertically by approximately 10-30%, and horizontally by 50-70%. Computed tomography allows for more accurate assessment of the architecture and volume of bone tissue. Dental radiography provides more accurate indicators of a toothless defect compared to orthopantomography.
If you are interested in this topic, pay attention to the webinar Individual implantation for bone deficiency .
