Complications during tooth extraction. Dislocation, fracture, aspiration
Machine translation
Original article is written in RU language (link to read it) , PT language (link to read it) .
In previous articles about complications that arise during and after tooth extraction, we found that dentists quite often encounter various problems during extraction operations. In this article, we will look at complications during tooth extraction such as fracture of the alveolar process of the jaw, dislocation and fracture of the lower jaw, and aspiration.
Principles of providing assistance for fractures of the alveolar processes and bones at the webinar Fractures of teeth and jaws in children and adults .
Fracture of the alveolar process of the jaw
A fracture of the alveolar process of the jaw can occur either due to the fault of the doctor (rough work, violation of the removal technique) or due to a pathological process (soldering of the tooth to the alveolar wall).
Types of fractures of the alveolar part of the jaw:
- fracture within the alveolus of the tooth being removed;
- fracture within the periodontium of several teeth;
- fracture of the alveolar process extending beyond the dentition (fracture of the tubercle of the upper jaw).
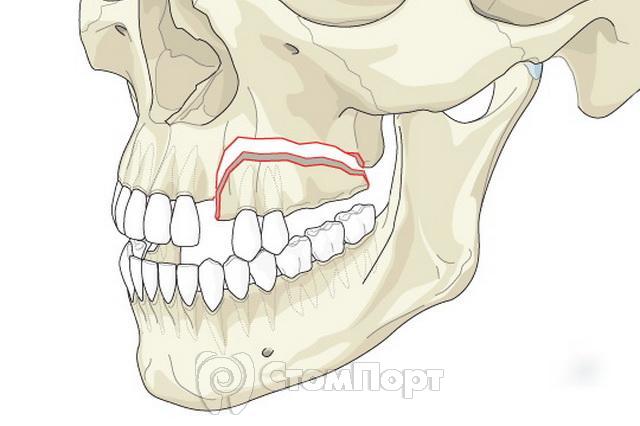
Causes of fracture:
- Compression of the bone during fixation of the forceps.
- Too active dislocation, which leads to bending and breaking of the alveolar wall.
- Pathological processes leading to a decrease in bone strength (cysts, tumors, osteomyelitis).
- Osteoid type of articulation.
Diagnosis of a fracture of the alveolar process of the jaw
Diagnosis of a fracture of the alveolar process of the jaw is based on the nature of the complaints, medical history, examination and x-ray examination.
Sometimes when a fracture occurs, you can hear a characteristic sound - a crack.
When the alveolar process of the upper jaw is fractured along with the tubercle, quite severe bleeding from the venous plexus may occur.
Symptoms:
- the appearance of foamed blood in the wound;
- passing a stream of air into the mouth during an increase in pressure in the nasal cavity (oronasal test);
- the appearance of blood from the nasal passage on the affected side.

Treatment of a fracture of the alveolar process of the jaw
If the fragment of the alveolar process remains connected to the soft tissues, then it is fixed with a metal splint. Otherwise, the fragment is removed and the sharp edges are smoothed. After this, an osteotropic biological preparation can be injected into the alveolus, and the edges of the gums can be brought together with sutures.
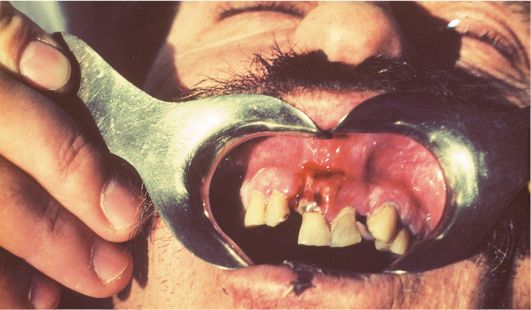
Fracture of the lower jaw
A fracture of the lower jaw most often occurs during the removal of molars with an elevator or chisel. The use of a chisel and hammer to “gouge out” a tooth or root, which was previously recommended, makes the danger of such a complication real. Therefore, a chisel should not be used to remove teeth. It is less traumatic and more effective to use an electric drill with rotating cutting tools (burs, cutters) for this purpose.

A fracture can be considered pathological if a history shows the presence of an inflammatory disease - cysts, tumors, tooth retention, osteomyelitis. Such pathological conditions lead to a decrease in strength, which in turn is a risk factor for fracture.
If a pathological fracture occurs during tooth extraction, it is necessary to carry out transport immobilization of the lower jaw with a chin-parietal bandage and refer the patient to a maxillofacial hospital.
A jaw fracture that occurs during tooth extraction cannot always be recognized immediately. After surgery, the patient may complain of pain in the jaw, difficulty opening the mouth and chewing. A thorough clinical examination and x-ray can determine the presence of a fracture.

Dislocation of the lower jaw
If the mouth is opened wide during anesthesia and tooth extraction, dislocation of the lower jaw may occur. This complication is more common in patients with habitual dislocation. The occurrence of dislocation can be facilitated by relaxation of the masticatory muscles under the influence of conduction anesthesia.
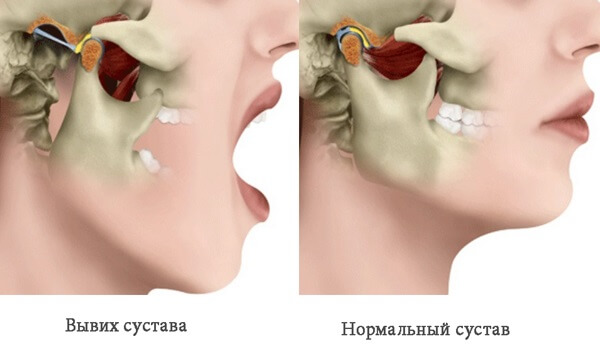
Clinic and diagnosis of dislocation of the lower jaw
The clinic and diagnosis of mandibular dislocation is based on the patient’s complaints and clinical examination. The main complaint is pain in the parotid region and the inability to close the teeth. Pain in patients with habitual dislocation may be moderate, as in patients who have undergone conduction anesthesia
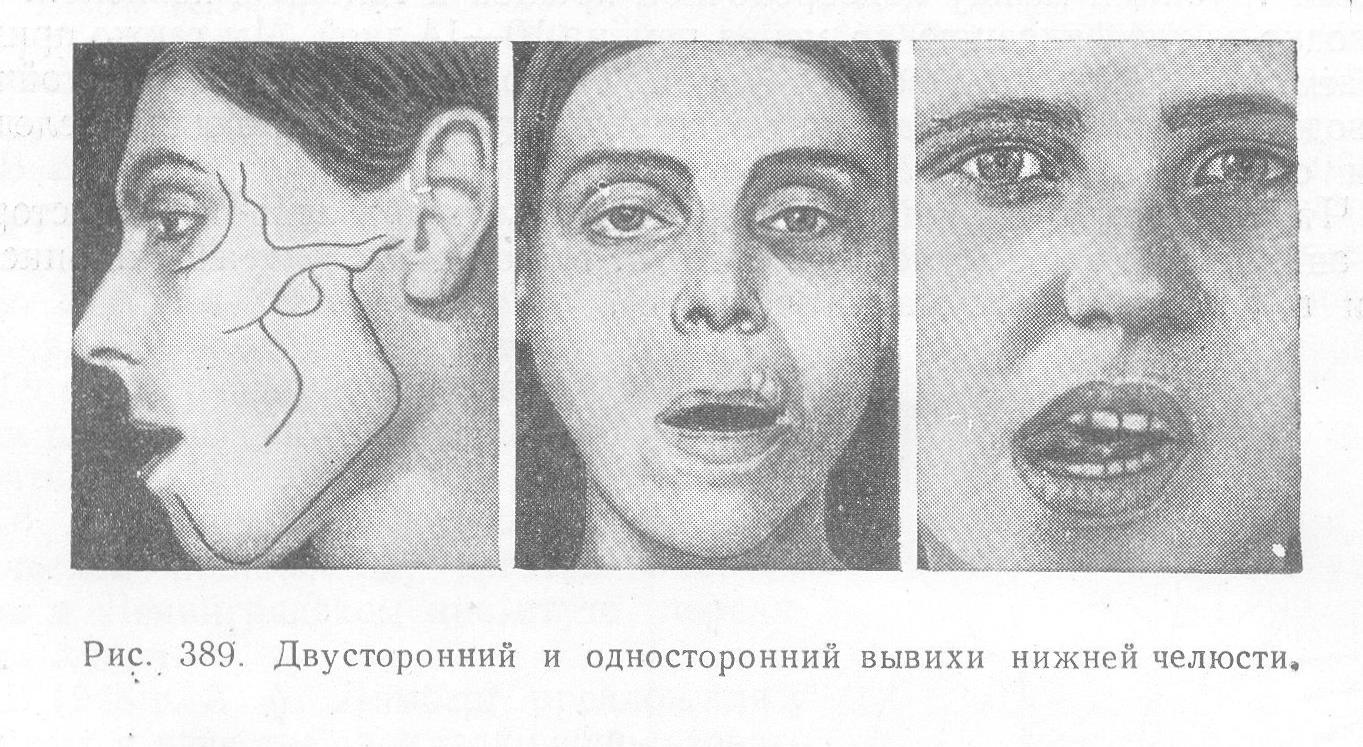
Clinical manifestations: the patient cannot close his mouth; in case of unilateral dislocation, the jaw is shifted to the healthy side; in case of bilateral dislocation, it is shifted forward.
A symptom of elastic mobility is characteristic of a dislocation. The doctor, grasping the lower jaw on both sides with his index fingers and thumbs, attempts to establish it in a position of central occlusion. To some extent this is successful, but as soon as you stop holding the lower jaw, it returns to its original position.
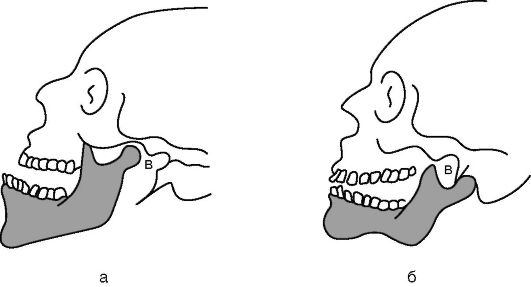
Dislocation of the temporomandibular joint a - anterior b - posterior

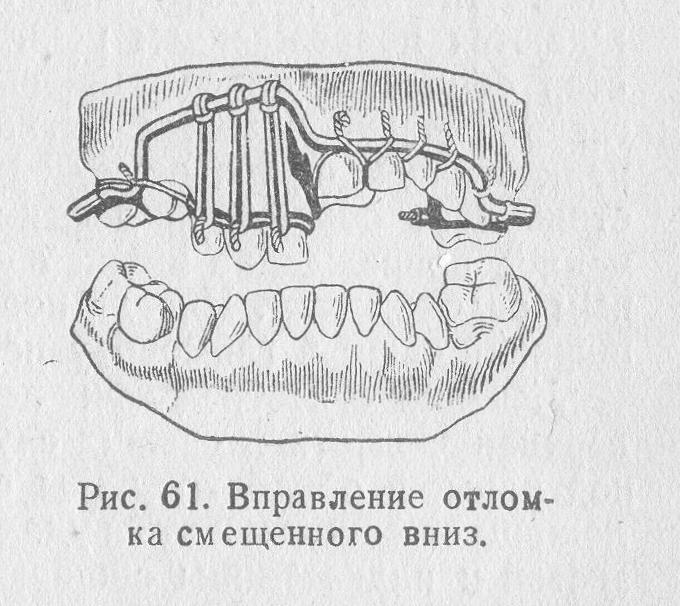
Treatment of lower jaw dislocation
We complete the tooth extraction and then treat the dislocation of the lower jaw.
First way . The chair is lowered, its back is set vertically. The patient rests the back of his head against the headrest and fixes his hands on the armrests. The doctor stands in front of the patient, wraps the thumbs of the right and left hands with gauze napkins or a towel. He then grabs the lower jaw with both hands so that the thumbs rest on the chewing surface of the molars, and the rest cover the lower edge of the jaw. After this, the doctor presses firmly with his thumbs on the molars, moving the lower jaw down. Without ceasing to push the lower jaw down, the doctor moves it posteriorly. The sound of a click and the disappearance of the symptom of elastic fixation indicate that the dislocation has been eliminated. Having warned the patient about the possibility of recurrence of the dislocation when the mouth is opened wide, the doctor applies a chin-parietal bandage to the patient to limit the opening of the mouth. It is recommended to wear the bandage for 5-6 days.
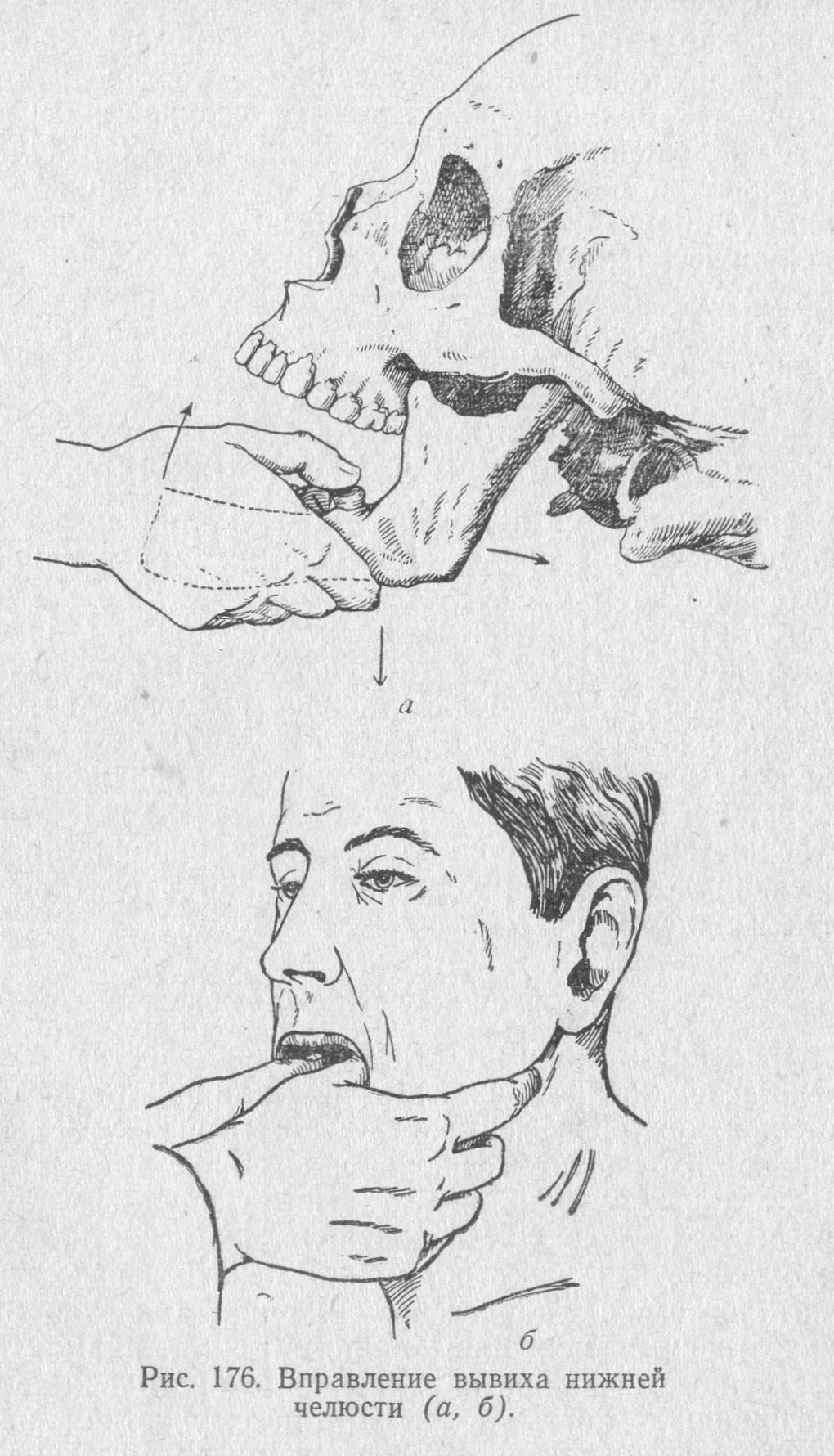
Second way . The patient is seated in a chair in the same position. The doctor stands in front of the patient, inserts the index fingers of the right and left hands into the vestibule of the mouth and moves them along the anterior edge of the branch as high as possible, to the top of the coronoid process. Then the doctor sharply and firmly presses on the anterior edge of the coronoid process. The essence of the method is that, having felt pain in the area of the anterior edge of the coronoid process, the patient tries to avoid it by eliminating the pressure of the doctor’s fingers. He cannot move his head and entire body backwards, as they rest against the back and headrest of the chair. Therefore, subconsciously he tries to move the lower jaw down and back, i.e. carry out the movement of the lower jaw that is necessary to eliminate the dislocation. In this case, the doctor does not have to overcome the force of contraction of the masticatory muscles, as is done when using the first method to reduce a dislocation.
Aspiration
Another complication that can arise during tooth extraction is aspiration.
Aspiration is the penetration of foreign bodies into the airways during inspiration. During tooth extraction surgery, there are cases of aspiration of the tooth, parts of the tooth, needles, cotton swabs, and burs.
The occurrence of aspiration is facilitated by a decrease in the gag reflex after anesthesia and the position of the patient in a chair or operating table with the head thrown back. The foreign body may be located above the vocal cords, in the larynx, trachea and bronchi.
Aspiration Clinic
Clinical signs of aspiration: sudden barking cough, severe shortness of breath, cyanosis of the skin, lips and oral mucosa, motor restlessness and “disappearance” of the extracted tooth, part or instrument.

Urgent Care. The patient is transferred to a sitting position with the torso tilted forward and down, and he is asked to “clear his throat.” In between coughing attacks, the oropharynx is examined and palpated, pulling the tongue forward. If a foreign body is detected in the oropharynx, it is removed with tweezers or a finger.
If a foreign body is not found in the oropharynx, and signs of asphyxia (suffocation) increase, one can think about the presence of a foreign body in the hypopharynx or larynx. In such a situation, one of the staff of the medical institution calls the resuscitation team by phone and prepares everything necessary for tracheotomy. Meanwhile, the doctor, having seated the patient on a stool and standing behind him, clasps his chest with his hands. Then he sharply compresses the chest, lifting the patient, thereby forcing exhalation. He repeats this artificial respiration technique several times. If these resuscitation measures do not help, asphyxia increases, and a tracheotomy is performed.

Prevention of aspiration
Prevention of aspiration consists of the following measures: careful use of small instruments, checking the fixation of the needle on the syringe, careful removal technique. If any tooth fragments disappear, it is necessary to examine the oral cavity and, if a foreign body is found, remove it.
If small instruments, teeth, or their fragments get into the oral cavity, the patient should be asked to lean forward and spit the contents of the oral cavity into the spittoon, rinse the mouth with water and spit again.
Learn more about complications during tooth extraction in the webinar Tooth extraction: step-by-step protocol. Treatment of complications .
