Color Change, Tooth Sensitivity, Aesthetic Self-Perceptions and Quality of Life after At-Home Dental Bleaching
ABSTRACT
Objective: The aim of this study was to determine the color change, tooth sensitivity, aesthetic self-perception and quality of life after at-home dental bleaching. There are additional details about at-home bleaching that you can obtain on our course "Teeth whitening: all techniques".
Material and Methods: Dental examination was performed and the initial color of the upper right incisor was recorded using a spectrophotometer (Easyshade Compact, Vita Zahnfabrik) and CIELab parameters. Individual vinyl trays were delivered to the patients (n=37) who were instructed to use the carbamide peroxide 16% (Total Blanc Home C16%, DFL) for 2 hours daily for 2 weeks. One-week after the end of treatment, measurements were repeated to calculate color (ΔEab, ΔE00) and whiteness index (ΔWID) variations. Oral Health Impact Profile (OHIP) and Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ) questionnaires were applied before and 30 days after treatment. Tooth sensitivity was by checked by visual analogue scale (VAS). Spearnan’s correlation tests were used to verify the possible relation between color change parameters and sensitivity. The Wilcoxon test was applied for results obtained by OHIP and PIDAQ questionnaires.
Results: Significant color change was observed after 14 days, regardless of the considered parameter. There was no significant correlation between sensitivity and color change. The dental self-confidence domain increased after bleaching (p = 0.029) and the psychological impact decreased (p = 0.001).
Conclusion: At-home dental bleaching was effective on the overall whitening and the color change was not related to tooth sensitivity. The bleaching treatment had a positive impact on the quality of life, reducing psychological discomfort and improving dental self-confidence and aesthetic self-perception.
INTRODUCTION
Oral health and functional rehabilitations were for a long time considered the primary goals in the dental treatment. However, due to scientific developments on the field of preventive dentistry and material’s science, aesthetics also became a key aspect of successful treatment [1]. Aesthetic evaluation is usually obtained through clinical parameters and objective criteria. Usually it was based on the professional’s observations and instrument readings but with fewer considerations on patient’s point of view – a fundamental aspect of evidence-based dentistry [2].
In this scenario, tooth color is one of the most commonly perceived aspects in a smile and can negatively affect aesthetic self-perception. Studies report that a large number of individuals are unsatisfied with their teeth´s appearance, and that more than half of this dissatisfaction may be related to the color of the teeth [3]. It is known that those who are satisfied with their appearance tend to be more extroverted and socially successful [4]. Thus, to assess patient’s aesthetic perceptions is as important as the dentist´s point of view in order to evaluate the success of a dental treatment [2,5-7]. A study has shown significant differences in aesthetic perception between patients and dentists [8] and the reasons for these differences may be at psychological and abstract levels, such as the ideal self-image for each person, personal motivation and cultural differences. In addition, the dentist tends to evaluate the results of a treatment in a fragmented way, while the patient evaluates the overall composition of the results [9].
Different techniques and materials can be used for tooth whitening and therefore many studies have been performed but just a few considering patient’s opinions [5-7]. Meireles et al. [10] applied the Oral Impact on Daily Performance (OIDP) questionnaire and detected a positive impact of the dental bleaching, with patients showing more their teeth after the procedure. On the other hand a difficult in dental hygiene and sensibility were also reported in that study. Fernández et al. [11] applied PIDAQ (Psychosocial Impact of Dental Aesthetics Questionnaire) and detected a positive impact on patient´s dental confidence and psychosocial well-being after dental bleaching. Another study, however, using the Oral Health Impact Profile (OHIP) did not find a significant association between dental bleaching and overall oral health quality of life [12].
As can be seen, there is an opposition of scientific findings regarding the effect of whitening on aesthetic self-perception and quality of life. One possibility that may be related to the variability of results is that the color change may vary according to each patient, as well as the potential for sensitivity to treatment. In fact, one may question whether the color change promoted by the material used may be associated with sensitivity and it is essential to establish whether this correlation is possible and could affect the results obtained. Thus, the present investigation aimed to determine the color change, tooth sensitivity, aesthetic self-perceptions and quality of life after at-home dental bleaching.
The research hypotheses were that the whitening treatment (1) improves patients’ quality of life and (2) aesthetic self-perceptions, but (3) the color change is directly associated with sensibility.
MATERIALS AND METHODS
This study was approved by the research ethics committee from the Veiga de Almeida University (UVA), according to protocol number 2.213.422. For the report of this clinical trial, recommendations of the CONSORT statement (Consolidated Standards of Reporting Trials statement) was followed.
Study setting and locations
This was a observational controlled equivalence trial. The clinical phase of the current study was performed from February 8, 2017, to February 8, 2018, in the Clinics of the School of Dentistry from the Veiga de Almeida University.
Recruitment and eligibility criteria
Patients for this clinical trial were recruited through posters fixed in the University walls and social media. All eligible volunteers read and signed the informed consent form before start the study. Volunteers should meet the following inclusion criteria: (a) be at least 18 years old; (b) have a good general health; and (c) have the six anterior maxillary teeth free of caries or extensive restorations. On the opposite, the exclusion criteria were: (a) untreated periodontal disease; (b) previous dental hypersensitivity; and (c) continuous use of analgesic or anti-inflammatory drugs; (d) tooth color A1 or lighter according to VITA Classic Color Scale (VITA Zahnfabrik, Germany).
Sample size calculation
To calculate the sample size, a power test (1-β) of 90% and a type I error (α) of 5% was considered. The variability data was extracted from a pilot study and found a standard deviation value of ΔEab of 1.5. The perceptibility threshold of 1.2 calculated in a previous study [13] was used as the acceptable difference. Thus, the average effect size was 0.8 (1.2/1.5) and a sample size of 28 participants was estimated for meeting these conditions. Since this was the first clinical trial conducted by this group of researchers at this site - and for this reason it was not possible to calculate the dropout rate - 40 patients were considered for study participation.
Intervention
At the first appointment, the participants filled out an anamnesis questionnaire about their general health, current and past medical history, use of medications and complaints regarding to oral health.
Three dentists, with more than 5 years of clinical experience (CVB, KBA and LMAC) performed the bleaching procedure. Dental examination was performed, and the baseline shade of the right maxillary incisor was recorded with a digital spectrophotometer (Easy Shade Compact, VITA Zahnfabrik, Germany) at the central third. Impressions of maxillary and mandibular arches were taken with alginate-based material (Hydrogum, Zhermack SpA, Italy) to obtain gypsum stone-based models and to fabricate custom trays by using a soft vinyl material and a vacuum-formed process.
One week after the first appointment the volunteers received the vinyl tray and the syringe of the carbamide peroxide gel (Total Blanc Home 16%, DFL, Rio de Janeiro, Brazil). The volunteers were instructed to deposit one drop of the product on the buccal face of all the apparent smile teeth in the tray. The tray was then positioned in the upper and lower arches, and excess product was removed. The volunteers received a syringe of the product, which was applied daily for 2 hours (according to manufacturer instructions) over the following two weeks. After each bleaching period, volunteers were instructed to remove the tray, rinse teeth with water and brush their teeth as usual. All patients received oral hygiene kits containing dental fluoride toothpaste (Colgate-Palmolive, New York, United States). The volunteers were then instructed to stop the bleaching treatment one week before the second appointments.
Outcomes
Questionnaires application – OHIP-14 and PIDAQ
Two questionnaires were applied to the participants before the first appointment and 30 days after the bleaching procedures: the Oral Health Impact Profile (OHIP-14) and the Psychosocial Impact of Dental Aesthetics Questionnaire (PIDAQ).
The OHIP-14 is a questionnaire composed of 14 questions, used to measure the impact of oral health on the individual’s quality of life. The participants should respond if any problems with their mouth or teeth interfere with their daily activities, such as talking, eating, tasting food, relaxing or relating to others. The possible responses for each question were: 0 = never, 1 = hardly ever, 2 = occasionally, 3 = fairly often, and 4 = very often. These individual scores were added to give a summary score ranging from 0
to 56. The greater the sum, the poorest the oral health related quality of life. OHIP-14 is divided into seven dimensions: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability and social disability. The outcomes were defined as the sum of the OHIP-14 and the dimension scores. The Portuguese version of OHIP-14 was used [14].
PIDAQ is an instrument with 23 statements, and for each of them the participants should select one of five sequential alternatives, from ‘I do not agree’ to ‘I totally agree’. The statements refer to the respondent’s feelings about the appearance of his/her teeth, such as whether he/she likes to see his own teeth in the mirror or in photos, hides his teeth while smiling, is envious of the nice teeth of other people, or if he cares about what other people think of his teeth. PIDAQ statements are grouped into four dimensions: dental self-confidence; social impact, Psychosocial impact and aesthetic concern. The outcomes were defined as the sum of the PIDAQ questionnaire and the dimensions scores. The Portuguese version of PIDAQ, validated for a population of young adults in Brazil [15], was used in this study.
Color assessment
Spectrophotometer analyses were performed before (first appointment) and after at-home dental bleaching (after 21 days, meaning one week after the last application) in the upper right incisor to calculate the bleaching potential. Readings, in triplicate, were taken in the middle third of the tooth and the L*a*b*c*h* parameters were recorded. Color difference (ΔE) was calculated by the CIELAB (ΔE ab) [16] and CIEDE2000 (ΔE00) [17] formulas: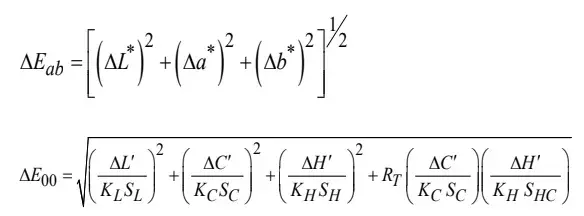
considering: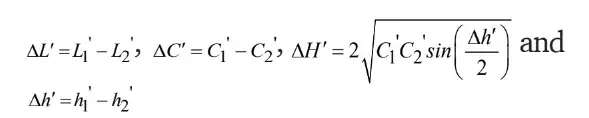
where ' ΔL , ' ΔC and ' ΔH are the mathematical differences in lightness, chroma, and hue between two different measurement periods and RT (rotation term) is a function that accounts for the interaction between chroma and hue differences in the blue region and for dental color space, it is close to zero [18]. KLSL, KCS C, and K HS H are empirical terms used for weighting the metric differences to the CIEDE2000 differences for each coordinate. Parametric factors were set to KL = 2, KC = 1, and KH = 1 according to the better performance of the ΔE00 equation [19]
The CIELAB-based whiteness index (WID) was calculated to determine tooth whiteness level, and considered the parameters established by Pérez et al. [20]: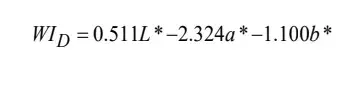 This calculation was performed with data obtained before (WID1) and after (WID2) the bleaching treatment. The formula ΔWID= WID2 − WID1 was used to calculate eventual differences of whitening level before and after the treatment and considered parameters that were previously proposed by Pérez et al. [21].
This calculation was performed with data obtained before (WID1) and after (WID2) the bleaching treatment. The formula ΔWID= WID2 − WID1 was used to calculate eventual differences of whitening level before and after the treatment and considered parameters that were previously proposed by Pérez et al. [21].
Tooth sensitivity evaluation
Dental sensitivity was recorded by using the visual analogue scale (VAS) method. In the second appointment, patients were asked about the intensity of spontaneous discomfort caused by the treatment and their responses were scored on the scale from 0 to 10, where 0 indicated that patients did not present any painful symptoms and 10 indicated the occurrence of severe sensitivity.
Statistical analysis
For the overall scores of OHIP-14 and PIDAQ the means and standard deviations were calculated, and for each domain Wilcoxon test (SPSS 21.0, IBM, USA) before and after bleaching. The level of significance adopted was 0.05. Descriptive analyses were performed for the data on color measurements and sensitivity level. To determine if the colorimetric variations are associated to the tooth sensitivity, Spearnan’s correlation tests (95%) were applied.
RESULTS
Forty patients were initially enrolled in the current evaluation and the final sample consisted of 37 (n=37), being 33 women (86.8%) and five men (13.2%). The average age was 23.1±4.6 years, with 22.6±4.0 years for men and 26.2±7.2 years for women.
The results of OHIP-14 questionnaire are shown in Table I. There were no differences in OHIP-14 overall score at baseline and one month after bleaching (p=0.166). The same occurred for six of the seven dimensions of OHIP-14. The exception was the psychological discomfort that significantly reduced after bleaching (p=0.034).
Table II shows the results of PIDAQ questionnaire. The overall score on the PIDAQ was not significantly different before and after bleaching (p=0.264). However, when the dimensions are considered separately, it can be observed that dental self-confidence increased after bleaching (p=0.029), whereas the psychological impact decreased (p=0.001).
The average color change obtained after 14 days of dental whitening were ΔEab = 4.4±1.4 for the CIELab parameter, ΔE00 = 4.2±2.1 for the CIE2000 parameter and ΔWID = 3.6±2.1 for the whitening index. There were no significant correlations between sensitivity and the colorimetric parameters (Figure 1). Almost 70% of the sample showed no sensitivity during tooth whitening treatment (Figure 2).
Table I - Distribution of scores of overall OHIP-14 and its seven dimensions, before and after bleaching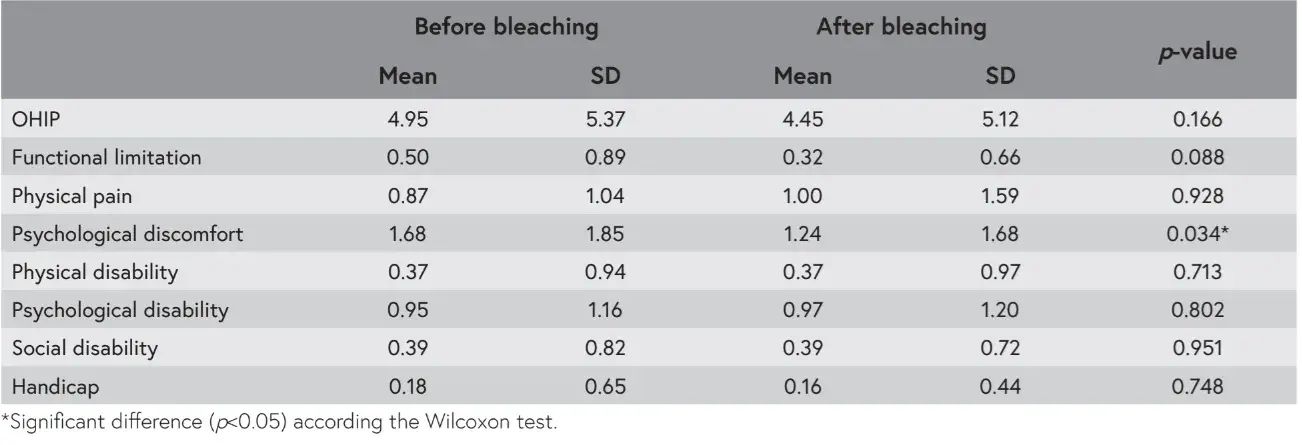
Table II - Distribution of scores of overall PIDAQ and its four dimensions, before and after bleaching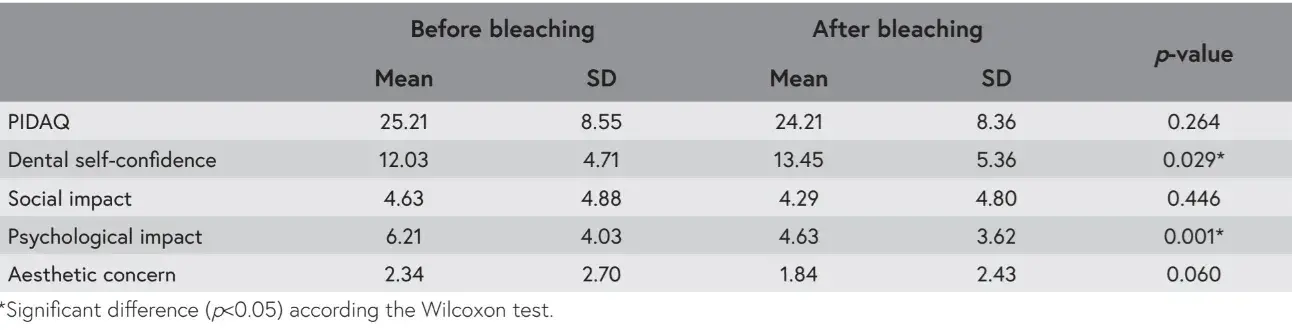
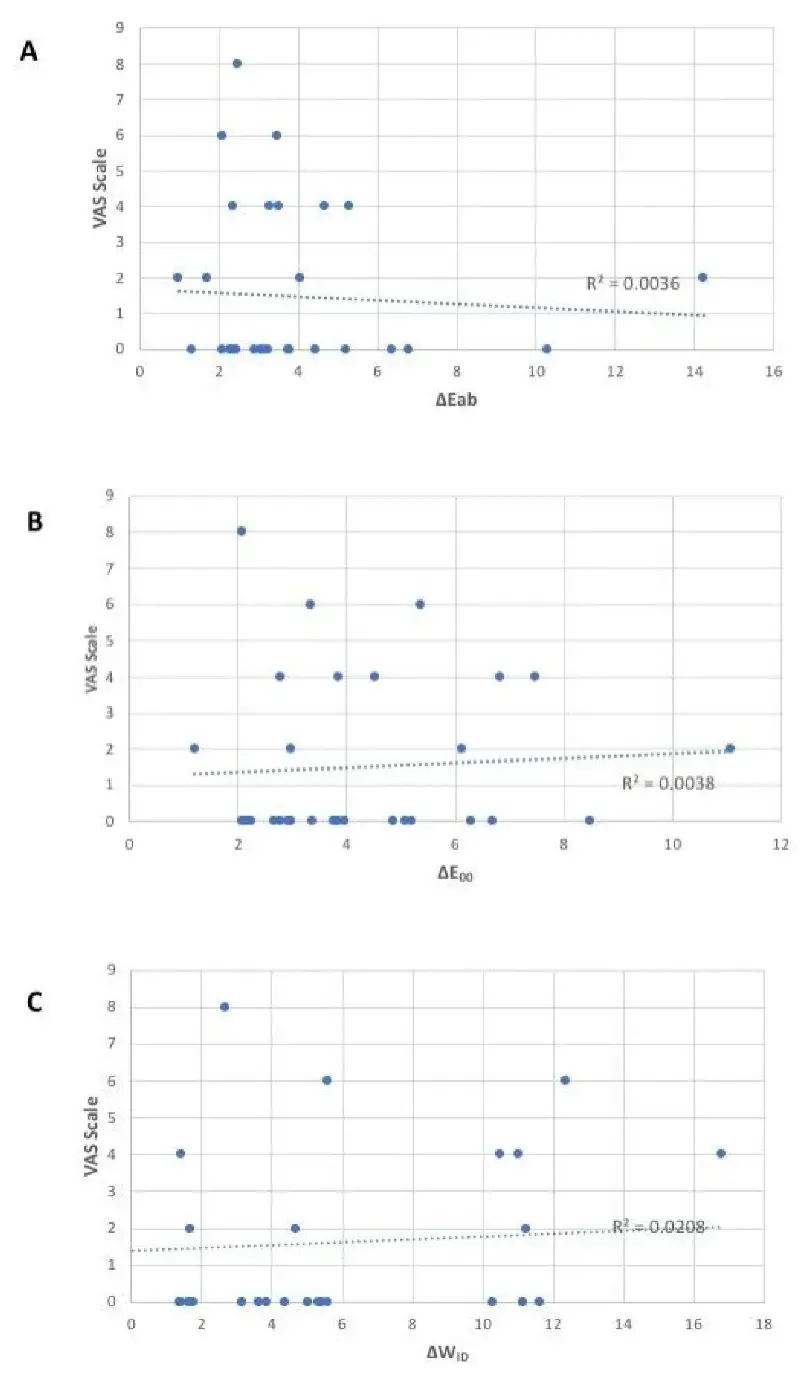 Figure 1 - Relation between colorimetric parameters variations – (A) ΔEab, (B) ΔE00 and (C) ΔWID) and sensibility.
Figure 1 - Relation between colorimetric parameters variations – (A) ΔEab, (B) ΔE00 and (C) ΔWID) and sensibility.
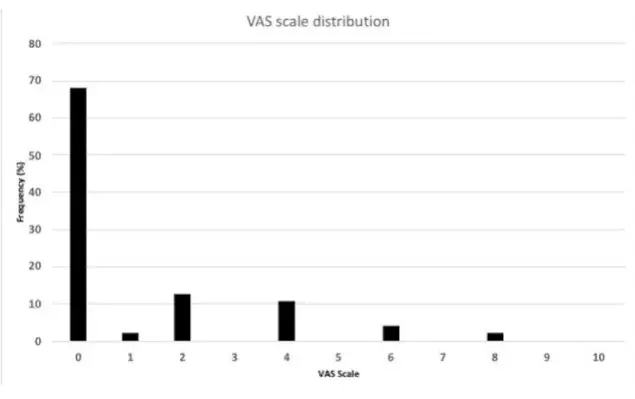 Figure 2 - Frequency (in percentage, %) of answers according the VAS scale.
Figure 2 - Frequency (in percentage, %) of answers according the VAS scale.
DISCUSSION
The outcomes indicate that dental bleaching can reduce psychological discomfort and psychological impact of dental aspects and can improve dental self-confidence, confirming the first and second hypotheses. Additionally, as it will be discussed, there was no relation between color change and sensibility, rejecting the third hypothesis.
It has been considered that clinical parameters are no longer sufficient to evaluate the success of a dental treatment and traditional measurements should be supplemented by information obtained from the patient [5-7]. In this sense the current study applied the OHIP-14 and PIDAQ questionnaires and the overall results tend to indicate that both were not affected by at-home dental bleaching. Although, it is mandatory to evaluate specific domains separated and therefore significant improvements are detected. The psychological discomfort has been significantly reduced, which means that after bleaching the individuals presented fewer feelings of worry and self-consciousness due to problems with the oral appearance [12]. Similarly, the psychological discomfort was significant reduced in OHIP questionnaire.
Dental bleaching also reduced the psychological impact of dental aspects, a dimension of PIDAQ that evaluates inferiority and unhappiness when individuals compare themselves to others. Besides, dental self-confidence was improved, which means that after bleaching the appearance of the teeth impact less on the emotional state and self-confidence of the individuals. This results are in agreement with other studies that showed increasing of patients’ satisfaction with their dental appearance after bleaching [5,6,9-11]. The findings of Fernandez at al [11]. showed a positive impact of bleaching even greater than the results obtained in this study, since impacted the overall scores of OHIP-14 and PIDAQ and all the dimensions of PIDAQ after one month. These differences can be explained by different methodologies and by the scores at baseline. First, they have used a different version of OHIP-14, called OHIP-Esthetics, and for this reason, comparisons cannot be done. Secondly, their population had a higher PIDAQ score at baseline, which probably reflects individuals more concerned and self-conscious of their appearance. These individuals may perceive minor variations more accurately. The findings of another study [12] showed no changes in overall OHIP-49 after bleaching, but an increase in physical pain (due to an increase in dental sensitivity) and a decrease in handicap. No difference in this domain was detected in this study since dental sensitivity was zero in almost 70% of the cases, which characterizes the procedure as not painful. Less than 10% of the sample reported having pain or tenderness during whitening. Beside the use of the complete version of OHIP (while we have used the short version), their population is much older (over 50 years) than that of the current study is (23 years). It was reported that older people perceive less impact regarding aesthetics, while younger people are more concerned with their teeth color [22].
Dental color, despite being one of the several factors that contribute to the aesthetic balance of the smile, is the single most important factor in this process because the color disharmony is more quickly noticed than other aesthetic anomalies [6,23]. One of the great divergences in the whitening studies is the evaluation of the whitening effect. Since 2000, the American Dental Association has recommended two methods, which are color measurement instruments (colorimeter or spectrophotometers) and reference color scales [24] and therefore a clinical spectrophotometer was used was used to calculate color variation. The outcomes of the current investigation indicate that the whitening treatment was effective, as the calculated color change is superior to that for perceptibility and acceptability thresholds regardless of the colorimetric parameter, ΔEab,, ΔE00 or ΔWID [13,18,21].
Dental sensitivity is a common effect after whitening and may be dependent on treatment time, concentration of peroxide and type of whitening agent. In the present study there was any report of high sensitivity according the VAS scale, 70% of the subjects showed any sign of sensitivity there was no correlation between the color change and postoperative sensitivity.
Such outcomes indicates that the carbamide peroxide 16% used for two weeks was effective, safe and that eventual sensitivity was related to individual perceptibility. Furthermore, the treatment safeness is also reinforced by the fact that the average age of the participants in the current investigation was 23 years old, that avoiding possible interference due to the physiological changes of dental tissues due to age like sclerotic dentin deposition.
It is important to highlight that the current outcomes considered a convenience sample, since it was composed by undergraduate dental students that were looking for a dental bleaching procedure. We can expect that these individuals have more concerns about their appearance than the usual population, and for this reason, aesthetic treatments are more prone to cause positive impact on them. On the other hand, dental students may be very demanding with their dental appearance because they may consider that dentists have the obligation to present nice teeth. Another limitation is that the impact of dental bleaching on oral heath related quality of life was assessed one month after treatment and not in the long term. Future investigations about the longevity of this impact would be interesting.
You have the opportunity to gather more in-depth information about teeth whitening on our course "Dental bleaching: the science based techniques for every day" by Marcos Barceleiro.
CONCLUSIONS
It can be concluded that at-home dental bleaching with carbamide peroxide 16% for two weeks presented positive impact in oral health related quality of life and aesthetic perceptions by reducing psychological discomfort and the psychological impact of dental aspects; improved dental self-confidence and promoted significant whitening with low level of tooth sensitivity, without correlation between these two variables.
List of authors:
Larissa Maria Cavalcante, Cynthia Fernandes Villar Baptista Bomgiovanni, Karinne Bueno Antunes, Eduardo José Veras Lourenço, Patricia Nivoloni Tannure , Luis Felipe Schneider
References
Lobo M, Liberato WF, Vianna-de-Pinho MG, Cavalcante LM, Schneider LFJ. Adhesion and optics: the challenges of esthetic oral rehabilitation on varied substrates-Reflections based on a clinical report. J Prosthet Dent. 2021;125(1):15-7. PMid:32059856.
Goulart MA, Condessa AM, Hilgert JB, Hugo FN, Celeste RK. Concerns about dental aesthetics are associated with oral health related quality of life in Southern Brazilian adults. Cien Saude Colet. 2018;23(11):3957-64. PMid:30427465.
Al-Zarea BK. Satisfaction with appearance and the desired treatment to improve aesthetics. Int J Dent. 2013;2013:912368. PMid:23509462.
Klages U, Claus N, Wehrbein H, Zentner A. Development of a questionnaire for assessment of the psychosocial impact of dental aesthetics in young adults. Eur J Orthod. 2006;28(2):103-11. PMid:16257989.
Bersezio C, Martín J, Herrera A, Loguercio A, Fernández E. The effects of at-home whitening on patients’ oral health, psychology, and aesthetic perception. BMC Oral Health. 2018;18(1):208. PMid:30537968.
Pavicic DK, Kolceg M, Lajnert V, Pavlic A, Brumini M, Spalj S. Changes in quality of life induced by tooth whitening are moderated by perfectionism: a randomized, double-blind, placebo-controlled trial. Int J Prosthodont. 2018;31(4):394-6. PMid:29624630.
Kothari S, Jum’ah AA, Gray AR, M Lyons K, Yap M, Brunton PA. A randomized clinical trial investigating three vital tooth bleaching protocols and associated efficacy, effectiveness and participants’ satisfaction. J Dent. 2020;95:103322. PMid:32200009.
Mehl C, Harder S, Lin J, Vollrath O, Kern M. Perception of dental esthetics: influence of restoration type, symmetry, and color in four different countries. Int J Prosthodont. 2015;28(1):60-4. PMid:25588175.
Krug AY, Green C. Changes in patient evaluation of completed orthodontic esthetics after dental bleaching. J Esthet Restor Dent. 2008;20(5):313-9. PMid:18837755.
Meireles SS, Goettems ML, Dantas RV, Bona AD, Santos IS, Demarco FF. Changes in oral health related quality of life after dental bleaching in a double-blind randomized clinical trial. J Dent. 2014;42(2):114-21. PMid:24316342.
Fernández E, Bersezio C, Bottner J, Avalos F, Godoy I, Inda D, et al. Longevity, esthetic perception, and psychosocial impact of teeth bleaching by low (6%) hydrogen peroxide concentration for in-office treatment: a randomized clinical trial. Oper Dent. 2017;42(1):41-52. PMid:27571237.
Bruhn AM, Darby ML, McCombs GB, Lynch CM. Vital tooth whitening effects on oral health-related quality of life in older adults. J Dent Hyg. 2012;86(3):239-47. PMid:22947847.
Paravina RD, Ghinea R, Herrera LJ, Bona AD, Igiel C, LinningerM, et al. Color difference thresholds in dentistry. J Esthet Restor Dent. 2015;27(Suppl. 1):S1-9. PMid:25886208.
Zucoloto ML, Maroco J, Campos JA. Psychometric properties of the oral health impact profile and new methodological approach. J Dent Res. 2014;93(7):645-50. PMid:24782438.
Sardenberg F, Oliveira AC, Paiva SM, Auad SM, Vale MP. Validity and reliability of the Brazilian version of the psychosocial impact of dental aesthetics questionnaire. Eur J Orthod. 2011;33(3):270-5.
Commission Internationale de l’Eclairage. Colorimetry: technical report. 3rd ed. Vienna: Bureau Central de la CIE; 2004. (CIE Pub.; no. 15).
Luo MR, Cui G, Rigg B. The development of the CIE 2000 colour-difference formula: CIEDE2000. Color Res Appl. 2001;26(5):340-50.
Pérez MM, Saleh A, Yebra A, Pulgar R. Study of the variation between CIELAB ΔE* and CIEDE2000 color-differences of resin composites. Dent Mater J. 2007;26(1):21-8. PMid:17410889.
PechoOE, GhineaR, AlessandrettiR, PérezMM, Della BonaA. Visual and instrumental shade matching using CIELAB and CIEDE2000 color difference formulas. Dent Mater. 2016;32(1):82-92. PMid:26631341.
Pérez MM, Ghinea R, Rivas MJ, Yebra A, Ionescu AM, Paravina RD, et al. Development of a customized whiteness index for dentistry based on CIELAB color space. Dent Mater. 2016;32(3):461-7. PMid:26778404.
Pérez MM, Herrera LJ, Carrillo F, Pecho OE, Dudea D, Gasparik C, et al. Whiteness difference thresholds in dentistry. Dent Mater. 2019;35(2):292-7. PMid:30527588.
Hägglin C, Berggren U, Lundgren J. A Swedish version of the GOHAI index. Psychometric properties and validation. Swed Dent J. 2005;29(3):113-24. PMid:16255355.
Soares KD, Nascimento-Júnior EM, Peixoto AC, Faria e Silva AL. Changes in dental esthetic perceptions of patients subjected to in-office tooth bleaching. Braz Dent Sci. 2018;21(2):230-6.
Siew C. ADA Guidelines for the acceptance of tooth-whitening products. Compend Contin Educ Dent Suppl. 2000;28(28):S44-7. PMid:11908348.
