Chronic apical periodontitis
Machine translation
Original article is written in RU language (link to read it) .
This article will discuss in detail chronic apical periodontitis, clinical picture, diagnosis and treatment features. We will also touch on the features of the clinic and the treatment of traumatic and drug-induced periodontitis.
On the histological aspects of the formation of periapical foci of destruction at the webinar Treatment of patients with periapical pathology: diagnosis, treatment, prognosis .
ICD classification – 10
K 04.4 Acute apical periodontitis of pulpal origin
K 04.5 Chronic apical periodontitis
Apical granuloma
K 04.6 Periapical abscess with fistula
- Dental
- Dentoalveolar
- Periodontal abscess of pulpal origin
By 04.60 Having communication with the HF sinus
By 04.61 Having communication with the nasal cavity
By 04.62 Having communication with the oral cavity
K 04.63 Having a connection with the skin
K 04.69 Periapical abscess with fistula, unspecified
K 04.7 Periapical abscess without fistula
- Dental
- Dentoalveolar
- Periodontal abscess of pulpal origin
- Periapical abscess without fistula, unspecified
K 04.8 Root cyst
K 04.89 Root cyst, unspecified
K 04.9 Other unspecified diseases of the pulp and periapical tissues
Classification of periodontitis according to I. G. Lukomsky
Acute periodontitis
- Serous
- Purulent
Chronic periodontitis
- Fibrous
- Granulating
- Granulomatous
Exacerbation of chronic periodontitis
Chronic apical periodontitis
Chronic apical periodontitis is most often an asymptomatic inflammation in the tissues of the apical periodontium, which is manifested by radiological changes at the apex of the tooth roots.
Many dentists use the clinically convenient classification of I. G. Lukomsky. It makes diagnosis easier.
Chronic fibrous periodontitis
Occurs as an outcome of acute periodontitis or treatment of granulating and granulomatous periodontitis. Traumatic etiology is also important due to overload, which occurs with the loss of a large number of teeth or non-physiological articulation.
Chronic fibrous periodontitis is detected on an x-ray as an expansion of the periodontal fissure in the apex area and is almost never accompanied by destruction of the adjacent bone.

Chronic granulating periodontitis
It is the most active form among all chronic periodontitis and is the outcome of an acute process.
The patient complains of unpleasant, slightly painful sensations when biting on the causative tooth.
Externally, the patient looks normal, sometimes there is an enlargement of the submandibular lymph nodes. In the oral cavity we see hyperemic mucosa in the tooth area, painful on palpation. A distinctive feature of this type of periodontitis is the presence of a fistula in the projection of the root apex. It may ooze pus or bulge granulations. Young granulation tissue grows through damaged cement or even dentin into the bone marrow spaces, often growing along the walls of the fistula tract. The tooth is destroyed or intact. Percussion is weakly positive.
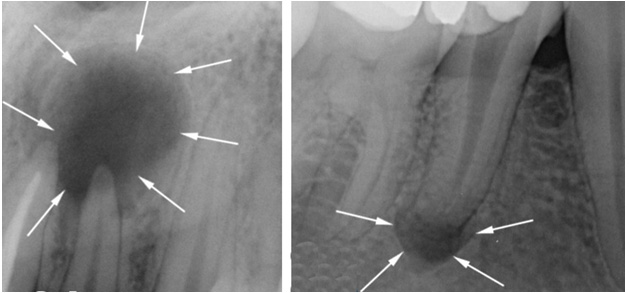
On the x-ray we see a clearing area due to bone destruction in the area of the root apex. The lesion has unclear contours and comes in different sizes.

Chronic granulomatous periodontitis
This type of periodontitis is asymptomatic and manifests itself clinically only during exacerbations. These manifestations can be of the type of granulating periodontitis in the form of fistulas and hyperemia of the mucous membrane.
The difference between granulomatous periodontitis and granulating periodontitis is the presence on the radiograph of a clearing focus at the apexes of the roots with a clear round shape (apical granuloma).
Currently, doctors are moving away from grading the size of the lesion: 0.5 cm - granuloma, 0.6-0.8 cm - cystogranuloma, more than 0.8 cm - radicular cyst.
Cyst
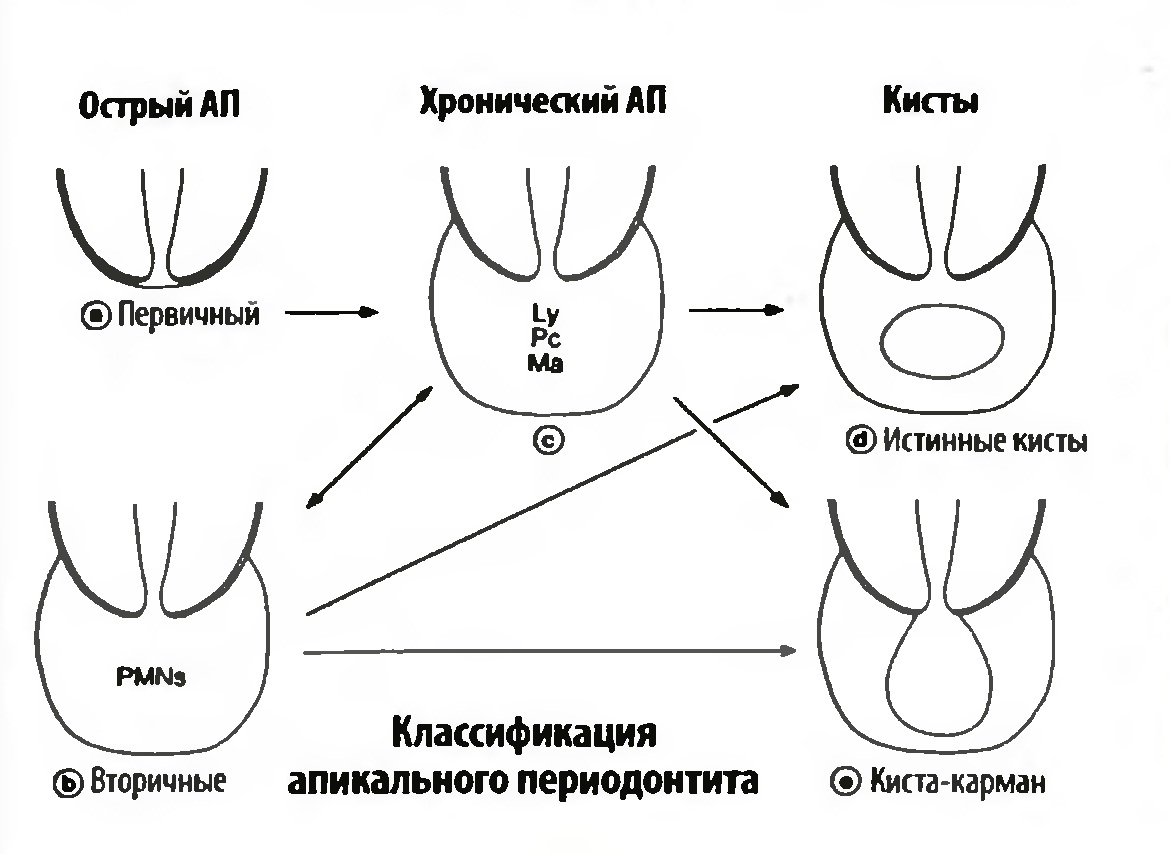
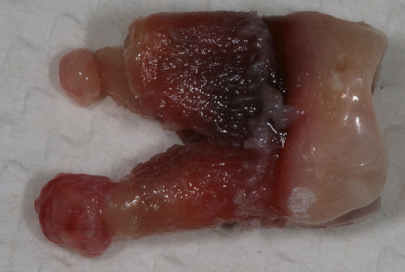
A cyst is a cavity that has an epithelial lining and cystic contents. There are two types of cysts: true and pocket.
The true one is completely covered by the epithelial lining, and the pocket one communicates with the root canal, it seems to grow from it.
Cyst formation occurs in 3 stages.
At the first stage, most likely, the epithelial cells of the Malasse islets proliferate under the influence of growth factors.
During the second stage, an epithelial cavity is formed.
These epithelial cells are directed away from their food source, die, and neutrophils drag their remains into the area of necrosis. Microcavities are formed, which then merge into one and become limited by stratified squamous epithelium.
There is another theory - the theory that the epithelium covers all open connective tissue areas due to necrosis.
At the third stage of cyst formation, after the death of neutrophils, there are reserves of prostaglandins, as well as cytokines produced by macrophages and T lymphocytes. Together they activate osteoclasts and trigger bone resorption.
Pocket cysts have a different mechanism of development. There is a large accumulation of neutrophils near the apical foramen in response to root canal infection. The cells die, as before, and this microabscess is closed by proliferating epithelium. A so-called epithelial ring is formed. Neutrophils that remain outside the channel die and form a microcavity. The presence of infection outside the canal further attracts neutrophils, expanding the microcavity to larger sizes. A pocket cyst is called such because of its similarity to the expansion of the root canal, an increase in the periodontal pocket.
Traumatic periodontitis
Periodontal trauma is one of the initiating factors in the occurrence of hemorrhage and the development of ischemia, which directly leads to the formation of pulp necrosis. The focus of necrosis attracts bacteria, colonizes them and infects the periodontium. With an increase in the number of microorganisms, acute inflammation begins. Traumatic periodontitis develops.
With chronic long-term trauma, periodontal restructuring occurs gradually, first due to its adaptation, then as chronic inflammation with lacunar resorption of the compact lamina.
The main reason for the development of pathology is the inflammatory response. As a result of occlusal trauma, inflammatory mediators are produced in the pulp; they are considered a protective reaction to mechanical aggression. They disrupt microcirculation and increase vascular permeability. The pulp dies.
When pulp necrosis reaches the apical periodontium, due to its cytotoxic effect, interleukins activate osteoclasts and bone resorption.
Medicinal periodontitis
Drug-induced periodontitis develops when aggressive liquids or drugs, such as arsenic paste, formalin, tricresol formalin, and phenol, enter the periodontium. Penetration into the periodontium occurs through the root canal.
This also includes periodontitis, which develops in response to the removal of phosphate cement, resorcinol-formalin paste, pins and other filling materials into the periodontium during the treatment of pulpitis. Drug-induced periodontitis also includes periodontitis due to allergies as a result of the use of drugs that can cause a local immune response (antibiotics, eugenol, etc.).

Foreign bodies
Gutta-percha, paper pins, calcium residues and a wide variety of other things can be found in the periapical tissues.
The apical periodontium always reacts to foreign bodies. They can enter through the root canal, through an injured mucous membrane or periodontal pocket.
In the case of paper pin penetration, it should be remembered that the human body does not know how to process cellulose, so the foreign body is surrounded by a bacterial plaque that maintains inflammation.
Gutta-percha is a biocompatible material. However, at the same time it can give a reaction from the apical periodontium. Studies in guinea pigs have shown that large particles of gutta-percha are encapsulated and surrounded by collagen fibers, while small particles support a local tissue reaction. And magnesium and silicon, which are contained in excess gutta-percha, can cause resorption.

Diagnosis of chronic apical periodontitis
Diagnosis of chronic apical periodontitis is similar to that in the case of acute apical periodontitis. This means we use basic and additional diagnostic methods.
The main ones include clarifying the patient’s complaints, medical history, probing, percussion, palpation and determining tooth mobility.
The patient’s complaints are most often absent, but they may complain of discomfort while eating when biting.
Probing is painless, palpation of the mucous membrane in the apical area is also painless. Percussion is weakly positive.
Additional special methods include determining the electrical excitability of the pulp (reduced to 200 μA), determining occlusion (the presence or absence of a traumatic factor), fistula tract, and temperature tests.
NB! We definitely do an X-ray examination.

Treatment of chronic apical periodontitis, traumatic and medicinal periodontitis
After diagnosis, they begin to draw up a treatment plan for chronic apical periodontitis, based on clinical and radiological data.
Treatment of traumatic periodontitis begins with identifying and eliminating the traumatic factor.
Treatment of medicinal periodontitis consists of antiseptic treatment of the root canal system, refilling when a foreign body is detected in the apical periodontium. When exposed to aggressive liquids outside the apex, place a cotton ball on the orifice or place a cotton ball in the canal moistened with an antidote (for example, for arsenic anhydride, the antidote is 5% unithiol solution or 2-3% iodine tincture). With arsenic periodontitis, pain is observed when biting on a tooth; there are rarely pathological changes in the mucous membrane.
When sodium hypochlorite is removed beyond the apex, sharp bursting pain, bruising, and swelling on the affected side are observed. The root canals are washed abundantly with saline solution, the area of the root apex is injected with saline solution in an amount 10 times greater than the volume of hypochlorite. Filling is started at the next visit if there is no progression of the pathological process.
Antibiotics, anti-inflammatory and antihistamine drugs are prescribed.
Common among the treatments for all types of apical periodontitis is endodontic treatment of the causative tooth.
Learn more about diagnosing apical periodontitis in the online lesson Finding foci of apical periodontitis on CBCT .
