Application of a papillary retention flap
Machine translation
Original article is written in RU language (link to read it) .
There are many techniques for using the papillary flap for both resective and regenerative purposes. This article describes the design of a papillary retention flap that relies on a palatal approach and has demonstrated successful long-term outcome.
Learn more about the types of flaps and their design in the webinar Working with soft tissues around implants: incision techniques and flap formation .
The papillary preservation technique described here is a modification of the Friedman bevel palatal flap that bypasses the interproximal and buccal tissue while leaving the papillary tissue intact. The indications for such manipulation are very specific, and its use is somewhat limited. However, the papillary flap is designed to reduce the depth of the periodontal pocket exceeding 5 mm and regenerate the hard and connective tissue in these areas.
Treatment of periodontitis ideally includes: removal of the pathogen, correction of the host's immune response, and regeneration of lost hard and soft tissue structures. It may not be possible to fully realize individual goals, let alone all of them, whether through non-surgical or surgical treatment. However, there is an acceptable clinical compromise: if the clinician achieves at least a reduction in pocket depth, then the patient, by using adequate oral hygiene practices and adhering to a strict schedule with his or her physician, can maintain that pocket depth while avoiding worsening. In most cases, reduction in pocket depth occurs due to gum retraction (or resection) rather than through restoration of connective tissue. In a patient at risk in the maxillary anterior sextant, any treatment, including SRP (scaling and root planning), can cause “black triangle disease.”
Patients should be aware of the possibility of soft tissue recession and its consequences (food entrapment, speech difficulties, cosmetic imperfections) after initial nonsurgical surgery. Clinicians can influence the level of mucosa postoperatively to a certain extent by designing flaps that will minimize changes in papillary anatomy. There are many techniques for using the papillary flap for both resective and regenerative purposes. A systematic review and analysis of flap procedures since 2012 suggested that they are becoming more popular and have better results.
This article describes the design of a papillary retention flap that relies on a palatal approach and has long-term outcome (28 years). By using the modified beveled Friedman palate flap technique, we avoid any manipulation of the interproximal or buccal tissue. Therefore, there are specific indications and limitations for its use. Indications include intraosseous and periosteal defects of the palatal region and interproxmal defects with an intact buccal wall. For aesthetic areas, intraosseous defects >4mm are a contraindication. For pockets on the palatal surface >5 mm (periosteal defects), intraosseous defects on the buccal surfaces may be a contraindication. SRP and professional oral hygiene are recommended in advance in all cases. For defects limited to the palatal and proximal surfaces, contraindications are: the need for facial prosthetics and subsequent crown lengthening.
The purpose of the papillary retention flap is to reduce the periodontal pocket depth beyond 5 mm and, if possible, to regenerate the hard and connective tissue in these areas.
Technique
The technique, which is illustrated in photographs 1 to 25, includes non-surgical and surgical stages. The non-surgical phase includes SRP, treatment of gingival inflammation and strict plaque control. If these problems are not resolved at the first stage, the course of the process after surgery can be unpredictable.
After completing the first stage of treatment, the doctor approves the treatment - papillary retention flap. Its use avoids manipulation of the mucous membrane on the proximal surfaces in the area of the enamel-cementum border. We reconstruct the pocket using palatal tissue. The first horizontal incision with an inward bevel is made approximately half the depth of the palatine pockets (photos 1-4). A palate with a higher vault (and a larger mucosal area) requires the incision line to be at a depth of 1-2 mm. If we have a shallower palate, then the cut begins at half the depth of the pocket. In either case, the initial incision is made at an angle, distal to the teeth involved, and remains tortuous.
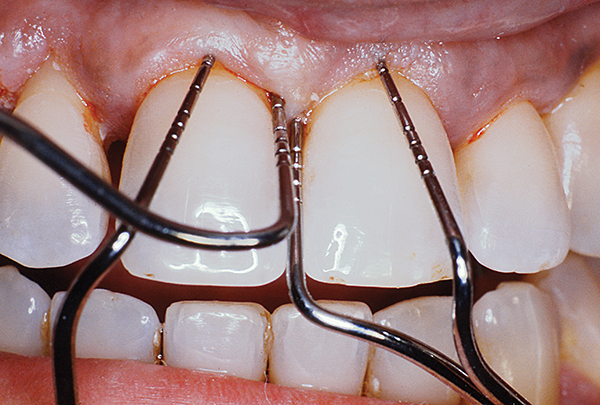
Fig.1
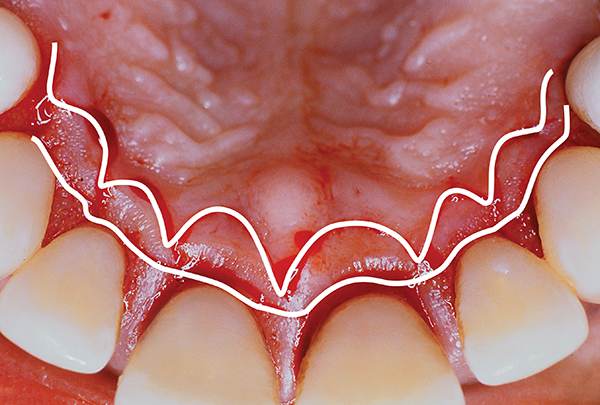
Fig.2
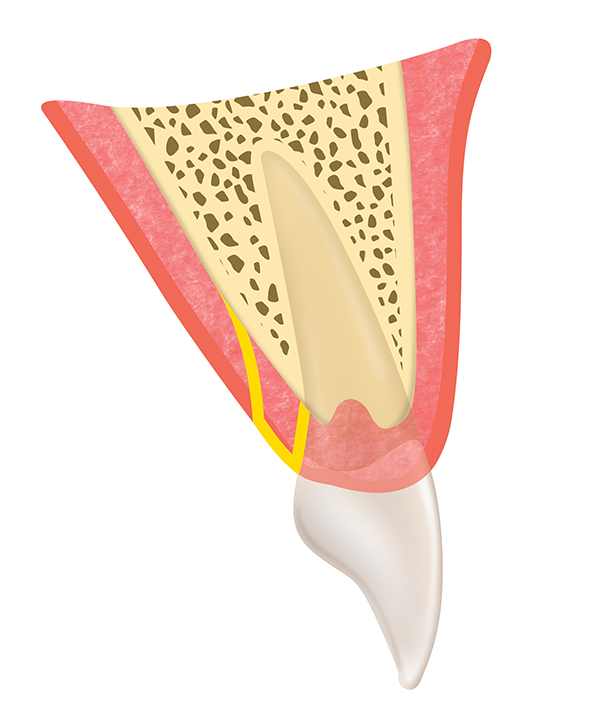
Fig.3
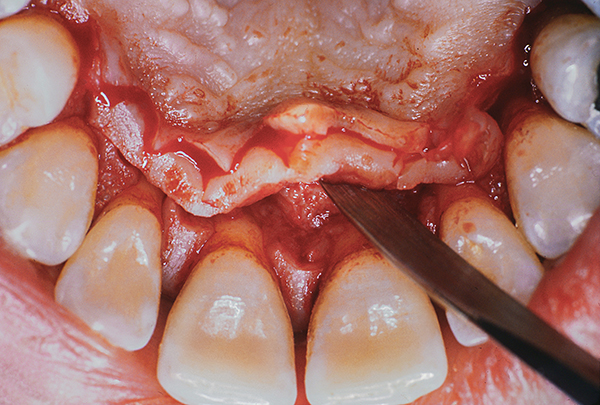
Fig.4
The second incision is made parallel and coronally oriented. It is tortuous and is located at an angle to the bone crest (photo 2-5). The proximal tissue remains intact. Once the second incision is made, we peel away the soft tissue (photos 4-5). Degranulations covering palatal or interdental bone defects can be treated by root planning combined with recontouring or regeneration. Vertical defects can be regenerated. Typically, freeze-dried bone autograft and a resorbable collagen membrane are used for this. The graft may include: biological modifiers, platelet-rich fibrin, platelet-rich plasma, bone protein and other bioinductive agents.

Fig.5
The palatal flap is sutured to the intact proximal and buccal mucosal surfaces using horizontal or vertical mattress sutures to ensure good attachment of the flap to the bone, as shown in Photos 6,7,10,11,19.

Fig.6

Rice. 7
Case 1: generalized progressive periodontitis – 3-year follow-up
Healthy, non-smoking 34-year-old woman. There is significant horizontal and vertical bone loss. Panoramic radiography showed 50% loss of alveolar bone (Figure 8). Periodontal pocket 6-9 mm deep. Initial therapy including oral hygiene education and SRP (4 times) was completed.
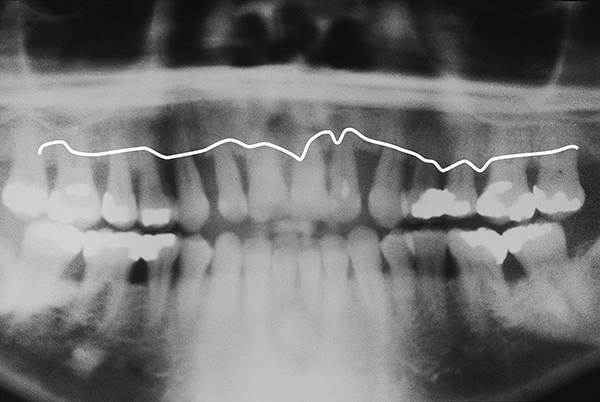
Fig.8
After this stage, the gums seemed less inflamed (photo 9). The surgical stage was performed using a papillary retention flap from the mesial edge of tooth 5 to the mesial edge of tooth 12 (Figure 10-12). Palatal and interproximal root surfaces, including the buccal surface of the proximal root. Sutures were applied: simple intermittent and vertical mattress sutures. The use of vertical mattress sutures made it possible to avoid the development of “black triangle disease” after surgery by minimizing tension on the tips of the papillae (photos 11, 12).

Fig.9
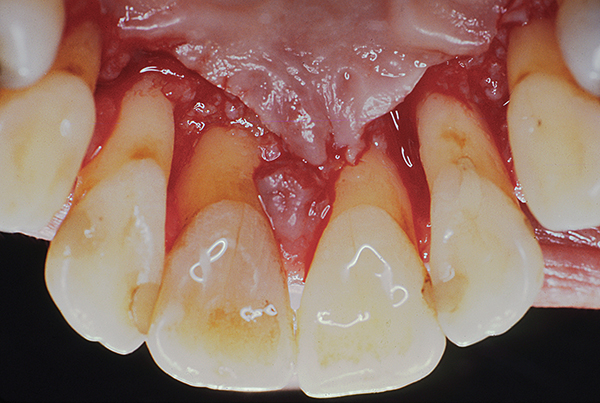
Fig.10

Fig.11

Fig.12
Healing proceeded without complications, the patient adhered to the 3-month observation schedule. Three years after surgery. The patient has a stable pocket depth of 3 mm or less (photo 13). Over time, no significant recession was observed and the gingival margin in the palate remained at the apical level (Figure 14, 15).

Fig.13

Fig.14

Fig.15
Case 2: Generalized chronic periodontitis of severe severity, follow-up for 31 years
A healthy, non-smoking 42-year-old man with severe generalized chronic periodontitis (Figure 16, 17). The initial mobility of the anterior teeth of the upper jaw is 1-2 degrees, pocket depth is 7-9 mm (palatal - 8 mm, vestibular - 2-3 mm). The patient noticed mobility and tooth decay. In addition, he was concerned about aesthetics (presence of diastema).

Fig.16
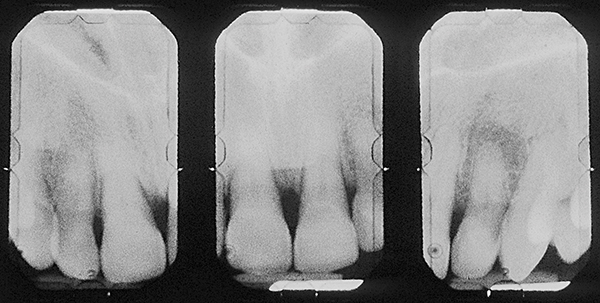
Fig.17
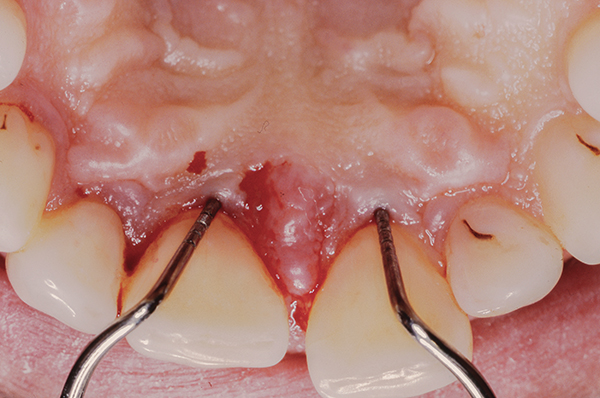
Fig.18
Initial therapy included oral hygiene and SRP. After which the pocket on the vestibular side was 1-2 mm, and on the palatal surface it remained the same (photo 18). After initial therapy, we applied a papillary retention flap to the maxillary anterior sextant.
After periodontal treatment was completed, minor orthodontic treatment was performed to address the gaps between teeth and correct the bite.

Fig.19

Fig.20

Fig.21
Case 3: Support for “Hopeless Teeth” for 28 years
A healthy, nonsmoking 38-year-old patient presented for a periodontal examination after being referred for extraction of all teeth. The diagnosis is generalized progressive periodontitis of severe severity. An x-ray revealed 60-70% bone loss (Figure 23). The interdental and palatal pockets had a depth of 6-9 mm. There was mobility.
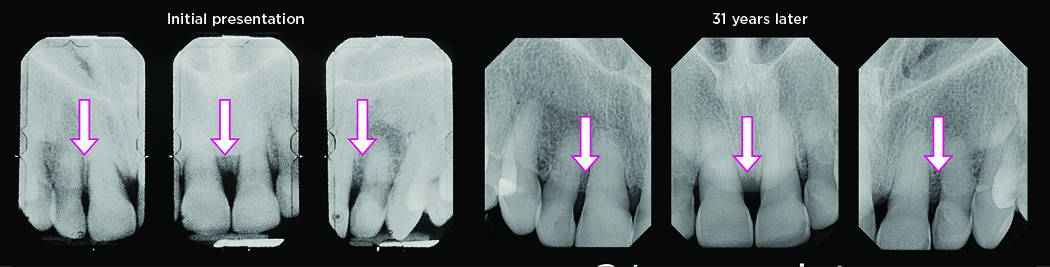
Fig.22
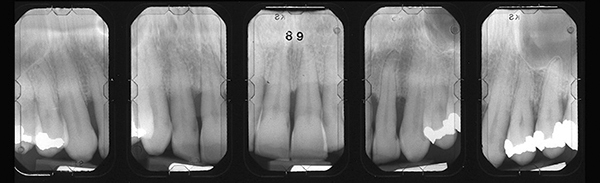
Fig.23
The patient was advised on oral hygiene and SRP. After this, the depth of the pockets was 6 mm, so surgical treatment was chosen to further reduce the pockets. In the area of the anterior sextant of the maxilla, surgery was performed using a Widmann flap. The patient was registered and underwent regular examination.
After 28 years, the patient retained all of his teeth except one, which had to be removed for endodontic reasons. Bone loss was stopped and the level of atrophy remained stable (Figures 24,25).
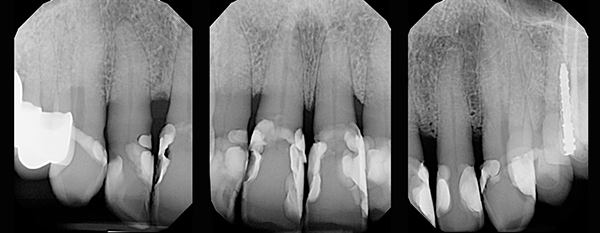
Fig.24

Fig.25
Conclusion
The flap design proposed by Friedman included: specially shaped incisions, root surface treatment, bone recontouring, and suturing in the correct order. The flap design presented here allows the papillary tissue to be left intact.
As demonstrated in the examples above, the results in pocket reduction and aesthetic restoration achieved with the use of the papillary retention flap have stood the test of time. Patients who have undergone this treatment continue to have regular check-ups with their doctor and maintain proper hygiene. Therefore, clinicians should carefully screen patients before surgery to select those who will subsequently adhere to recommendations. Only in this case the achieved result will be preserved for a long time.
More detailed and up-to-date information on the webinar Coronal displacement flap - surgical elimination of gum recession in the area of one or several teeth .
http://www.aegisdentalnetwork.com/
